Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The advent and refinement of minimally invasive surgery (MIS) techniques within the realm of oncologic hepatobiliary surgery (see Chapter 127 ) has paved the way for the collateral development of this field in living donor liver transplantation (LDLT) (see Chapter 121 ). Further to the initial French report of laparoscopic donor left lateral segmentectomy two decades ago, there has been a gradual accrual of literature in the arena of MIS living liver donation, with subsequent description of laparoscopic-assisted/hybrid or hand-assisted donor hepatectomy. , Indeed, the feasibility of pure laparoscopic liver donation has been recognized in more recent years, with the predominant experience being reported from Far Eastern nations and Europe. , In addition, whereas the vast majority of these reports have focused on laparoscopic techniques, the impetus on robotic living liver donation has as yet been comparatively lacking in traction. ,
The fundamental premise of living donation is one of donor safety, as this procedure comes with no physiologic benefit to the donor (see Chapters 105 , 109 , and 121 ). As such, every effort should be made to minimize the risk of donor complications through the judicious selection of lobe laterality, leaving at least 30% functional liver remnant (FLR) (see Chapter 4 ) in the donor while permitting a minimum graft-recipient weight ratio (GRWR) of 0.8 or graft volume to standard liver volume (GV/SLV) of 35% to 40%. Adequate experience of the surgical team is also crucial. Invariably, most described series of laparoscopic living donation have been undertaken by surgeons with proficiency in both laparoscopic oncologic hepatic resections (see Chapters 127D and 127E ) and open liver donation (see Chapter 121 ), and this is of paramount importance in the safe undertaking of this procedure. , These facets notwithstanding, laparoscopic living donor hepatectomy serves to improve the recovery of the donors through the already known benefits related with MIS that include less intraoperative blood loss, shorter hospital stay, reduced postoperative analgesic requirements, and earlier return to normal activity. ,
The candidacy of a prospective donor may vary across institutions and will not be discussed in detail in this chapter (see Chapters 105 , 109 , and 121 ). However, it is noteworthy to consider the difference in donor selection when the laparoscopic approach is considered. Considering the safety of the donor, with the addition to the complexity of the operation, it is recommended to start selecting donors with smaller livers, sufficient future remnant volume (see Chapter 4 ), and favorable anatomy before the learning curve of the program is accomplished. The presence of unfavorable hilar anatomy (see Chapter 2 ) as evidenced by early bifurcation of ipsilateral portal vein or bile duct is usually associated with wider Glissonian pedicles, and safe dissection and optimal division are more difficult, which may result in increased complications such as stricture or leakage of the bile duct. , With accumulation of experience, it is known that these obstacles can be overcome, but the application of a laparoscopic approach can yield increased frequency of multiple bile ducts of the graft, adversely affecting the recipient outcome. Therefore expansion of selection criteria for donors should be done with caution, weighing the advantages and the disadvantages of both the donor and the recipient outcome to have optimal results. ,
We elaborate on our setup and technique for purely laparoscopic right, left with middle hepatic vein (MHV) and caudate lobe, left without MHV and caudate, and left lateral sectionectomy below.
Our preference for patient positioning is akin to the “French” system, where the donor is placed in a modified lithotomy position with legs abducted in stirrups to 20° to 30° ( Fig. 128.1 ). For right hepatectomy, a degree of left tilting of the torso is beneficial for mobilization of the right lobe and facilitated by the placement of a cushion or rolled blanket behind the right scapular region. The patient should be firmly secured to the operating table to prevent sliding due to changes in table positioning during surgery.

The primary surgeon stands between the patient’s legs while the camera operator is to the left of the patient’s left leg. The first assistant is positioned to the left of the patient’s torso, right of the camera operator ( Fig. 128.2 ). The scrub nurse is to the left of and behind the primary operator and surgical instruments are placed in this area.

The maintenance of low-volume anesthesia during liver parenchymal transection is key to curtail intraoperative blood loss (see Chapters 25 and 121 ). Good communication between the anesthesia and the surgical teams is key. The placement of a central venous catheter is not uniformly performed, and reliance on other indices of fluid status such as stroke volume variability can help further abrogate interventional risks to a living donor. To prevent kidney injury while maintaining a low-volume status during transection, the patient is kept dry throughout the operation until the parenchymal transection is complete, at which point the anesthesia team is informed to refill the depleted volume with intravenous (IV) bolus to reach euvolemic state before the surgery ends. If colloids are deemed to be necessary, they are given after the parenchymal transection is complete. Transversus abdominis plane (TAP) block with bupivacaine is routinely used for better postoperative pain control as part of our enhanced recovery after surgery (ERAS) protocol (see Chapter 27 ).
The use of a three-dimensional (3D) flexible camera system (EndoEye Flex 3D, Olympus, Center Valle, PA) is our preference as it greatly facilitates depth perception and adequate visualization of tight corners, , thereby enabling safer dissection in the region of the root of the hepatic veins, posterosuperior right lobe, and short hepatic veins. In addition, spatial bimanual tasks such as intracorporeal suturing are eminently suited to and hastened by 3D visualization and this technology may indeed serve to reduce the learning curve for laparoscopic hepatectomy. Two 3D monitors are placed beyond either shoulder of the patient angled inward toward the surgeon and should be positioned at eye level to prevent double vision (see Fig. 128.1 ).
We also place a third monitor positioned between both 3D monitors, which is used for indocyanine green (ICG) enabled endoscopic fluorescence imaging of the bile ducts (Pinpoint, Stryker, San Jose, CA). The ICG imaging technology allows real-time visualization of the bile ducts, which greatly facilitates and improves the accuracy of bile duct division compared with conventional cholangiogram (see Chapter 24 ).
With respect to laparoscopic insufflation, our inclination is toward the use of the AirSeal system (ConMed, Utica, NY) as this enables a stable degree of pneumoperitoneum despite the use of cavitron ultrasonic surgical aspirator (CUSA, Integra, Princeton, NJ) and the frequent requirement for suctioning. This helps promote operative flow and shorten times. However, the high-flow nature of the AirSeal system may cause increased CO 2 retention; therefore we keep it at a lower pressure level of 11 cm H 2 O.
Ultrasonic shear device is deployed for dissection of the hepatic ligaments, some parts of hilar dissection, sealing vessels less than 2 mm in diameter, and for initial transection of the first 1 to 2 cm superficial layer of the liver as sizeable vascular structures are uncommon ( Fig. 128.3 ) (see Chapters 121 , 127D , and 127E ). Battery powered cordless options afford more freedom with the instrument handling, but the counterparts with cords usually afford better energy delivery with improved bleeding control. New devices are constantly being developed, and the surgeon should be familiar with the advantages and disadvantages of each product line and choose the product best suited for one’s preferences.
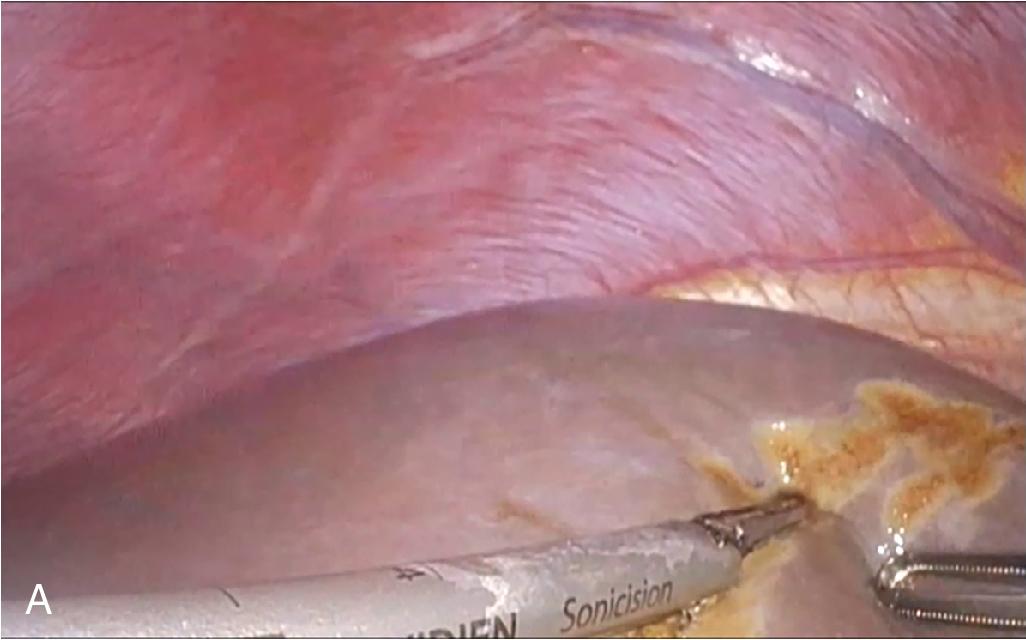
Precise dissection of the parenchyma is of vital importance in donor hepatectomy to keep the surgical field dry and have a clear vision in order to prevent any inadvertent injury to important structures or vessels (see Chapter 121 ). Crush clamp technique, either with or without coagulation function, ultrasonic shear device, and CUSA are the most commonly used methods for transection (see Fig. 128.3 ). Adding monopolar coagulator nosecone on the CUSA hand piece provides electrocautery without the need of instrumental change, which greatly improves hemostasis. Also, by turning off the laparoscopic mode, it can be used as a gentle suction device while transecting the liver. Notably, irrespective of instruments used, dissection should not be done blindly, especially in the deeper parenchyma, because this is where major bleeding events usually occur. Bipolar electrocautery has been our preferred instrument to safeguard bloodless parenchymal transection, and a second bipolar forcep in the tray allows rapid cycling of these instruments between cleaning of charred contact plates, which allows parenchymal transection without interference of surgery. A supplemental soft coagulation instrument, handled by the assistant providing additional hemostasis, offers a smoother and more efficient transection.
The ability to control major bleeding is essential in ensuring the safety of the donor operation (see Chapters 25 , 101 , and 121 ); therefore a well-considered strategy is required before undertaking a laparoscopic program. Although blood loss is usually insignificant and patients do not require any transfusion, it is our preference to always have the suction device attached to the Cell Saver (Haemonetics, Boston, MA) in case significant bleeding occurs and autotransfusion becomes necessary. The use of bipolar electrocautery, energy-assisted coagulative devices, and/or vessel clips is typically the first step toward establishing hemostasis and is usually met with success. Temporary packing of the field with hemostatic agents (e.g., oxidized cellulose derivatives) or sponge and revisiting the area a few minutes later often proves beneficial.
In case of more brisk bleeding as will be seen with larger caliber vessels, bleeding control often only can be achieved through direct repair of the bleeding site either by clipping or suturing. In such circumstances, ensuring low central venous pressure, including the use of 30% reverse-Trendelenburg positioning, with temporary increase of the insufflation pressure up to 15 mm Hg can help reduce the rate of bleed (see Chapters 25 , 127D , and 127E ). Temporary reduction of the tidal volume is proven to be effective as well. Regardless of the method used, reducing bleeding through counterbalance using pneumatic pressure should be done judiciously. CO 2 gas embolism and hypercarbia inevitably occur, and although usually clinically insignificant when the duration is short, prolonged use may result in significant respiratory acidosis and hemodynamic instability. Finally, the application of the Pringle maneuver (see Chapters 101 , 121 , 127D , and 127E ) can provide a summative effect to hemostatic control and can be resorted to without concern for graft outcomes in those recipients with projected good GRWR.
Laparoscopic vascular clamps should always be prepared and be available in the operating room in case it becomes necessary for rapid bleeding control ( Fig. 128.4 ) (see Chapters 127D and 127E ). The threshold to convert to open (see Chapter 121 ) must remain low to ensure donor safety, but it is crucial that conversion is not rushed through because loss of the pneumoperitoneum will result in increased bleeding. Step-by-step strategy during conversion should be preplanned, and the whole team should be familiar with the process to prevent chaos.

Following establishment of pneumoperitoneum via the periumbilical 12 mm port, a 12 mm port is placed at the right subcostal region along the right anterior axillary line and a 5 mm (assistant) port is placed next in the left subcostal anterior axillary line (see Fig. 128.2 ).The round and falciform ligament is sectioned with an energy device in a caudocranial direction. At its inferior aspect, dissection is kept close to the abdominal wall so as to remove redundant fat with the ligament, and once anterior to the liver, this line is continued approximately 1 cm away from the liver surface. Dissection is thus carried out toward the diaphragm and base of the hepatic veins, exposing and dividing loose areolar tissue at the anterior apex of the bare area of the liver. The 12 mm epigastric (primary surgeon) midline port is now placed and another 12 mm (assistant) port is also inserted in the midline subxiphoid region, a few centimeters cranial to the aforementioned trocar. The right subcostal and the epigastric midline port are the main ports used by the primary surgeon, and the camera is positioned between these thus offering a good triangulation along the line of Cantlie (see Fig. 128.2 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here