Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Pectus excavatum is a depression of the anterior chest wall. It can be present at birth or may develop during childhood or early adolescence. The depression usually gets deeper as the child grows. During puberty, the deformity can worsen precipitously in as little as 6 months. Patients with a mild or moderate excavatum are generally asymptomatic and are treated with an exercise and posture program. Patients younger than 11 years with less than 1.5 cm in depth respond well to vacuum bell therapy and are offered this therapy.
Patients with a severe pectus excavatum (approximately one-third of the total) suffer from cardiac and pulmonary compression and frequently present with dyspnea on exertion, chest pain, decreased endurance, and exercise intolerance. Patients who are clinically diagnosed as having a severe deformity undergo a workup to confirm objectively the need for operative correction.
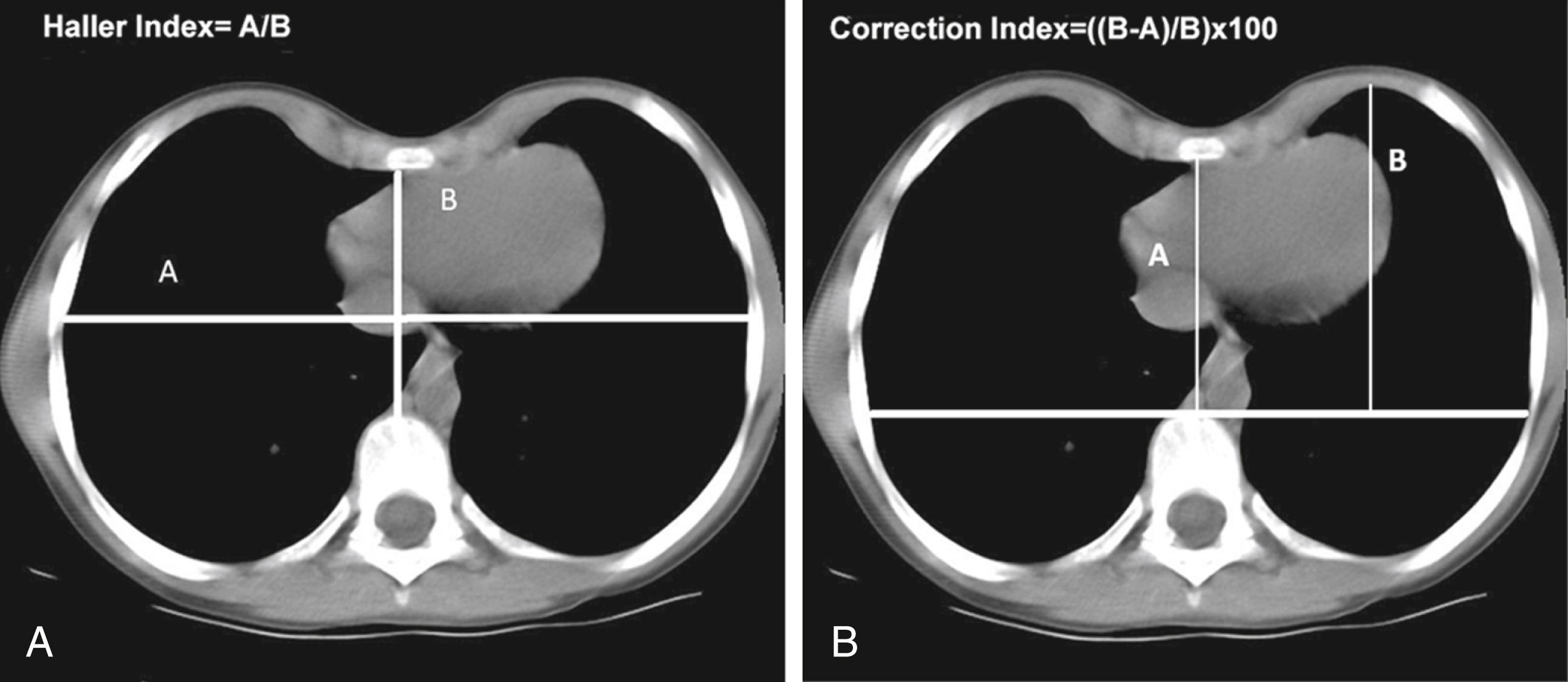
Evaluation of clinical severity can include a computed tomography (CT) or magnetic resonance imaging (MRI) scan of the chest, pulmonary function tests (PFTs), and cardiology evaluation ( Fig. 40-1 ). The three-dimensional imaging allows evaluation of the anterior chest wall and demonstrates cardiac compression and displacement. CT scanning permits objective assessment of the severity of the depression by comparing the ratio of the transverse internal thoracic diameter to the anteroposterior diameter at the deepest part of the depression (Haller index). Haller and associates proposed that an index of greater than 3.25 constitutes a severe depression ( Fig. 40-2A ). 1 The Correction Index (CI), as proposed by the Kansas City group, is also utilized. With the CI, a value greater than 10% indicates a severe deformity ( Fig 40-2B ). 2
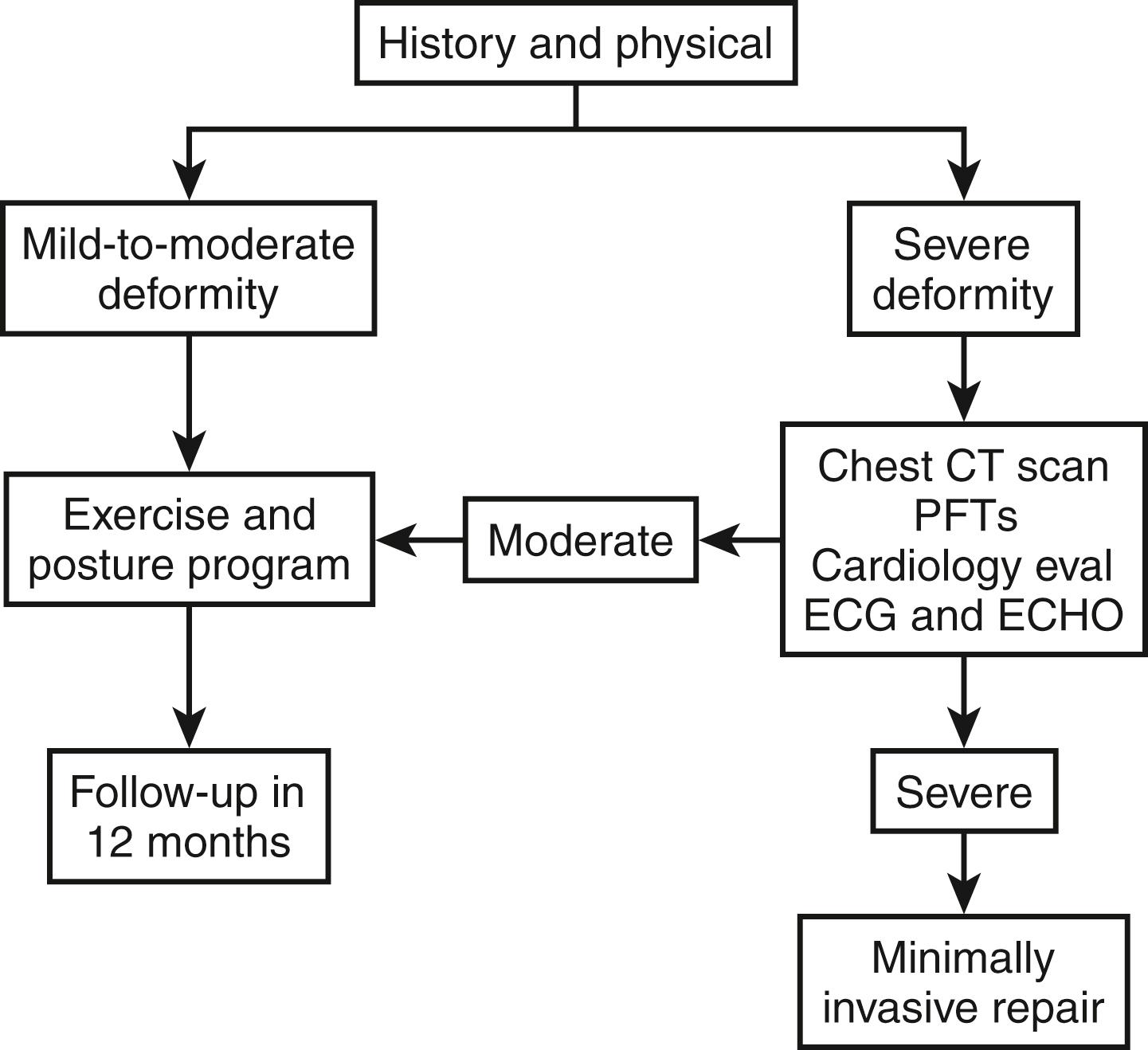
If indicated, PFTs are obtained to evaluate for restrictive airway disease. Exercise pulmonary function studies may show a limitation in oxygen uptake (VO 2max ) and a decreased ability to perform cardiopulmonary work. A cardiology evaluation is sought on many patients. The electrocardiogram (ECG) and echocardiogram may reveal conduction pathway abnormalities, mitral valve prolapse, right ventricular wall abnormalities, or other effects of cardiac compression. These tests can help determine whether the patient is an appropriate candidate for a corrective operation.
Operative correction is indicated by the presence of two or more of the following criteria:
A Haller index greater than 3.25, with cardiac or pulmonary compression, or a CI greater than 10%
Pulmonary function studies that indicate restrictive airway disease
A cardiology evaluation including ECG and echocardiogram showing that the cardiac compression is causing murmurs, mitral valve prolapse, cardiac displacement, conduction abnormalities, or other adverse functional effects
Documentation of progression of the deformity with associated symptoms
Failed previous repair
The operation is best performed between 10 and 25 years of age, and ideally at 12 to 14 years. At that age, the chest is very malleable. However, the Nuss procedure has been successfully applied to patients as old as 70 years. At the present time, it is recommended that the support bars remain in place for 2 to 4 years. Patients whose bars are removed before puberty have an increased risk of recurrence. Older patients sometimes require two and occasionally three bars.
All patients treated with an operation are also treated with an aerobic exercise, deep breathing, and posture program starting at their first consultation. They are encouraged to continue with the exercise program until 1 year after bar removal. Before surgery, all female patients are evaluated for metal allergy, and are those with a personal or family history of metal allergy. If patients are allergic to metallic objects (usually a nickel or copper allergy), then a titanium bar is used.
After induction of anesthesia and administration of intravenous cefazolin, the patient is positioned supine with both arms abducted 75 degrees at the shoulder, with the elbows slightly flexed. The wrists are elevated on rolled-up foam and secured on arm boards. Photographs are taken of the chest before the operative correction begins.
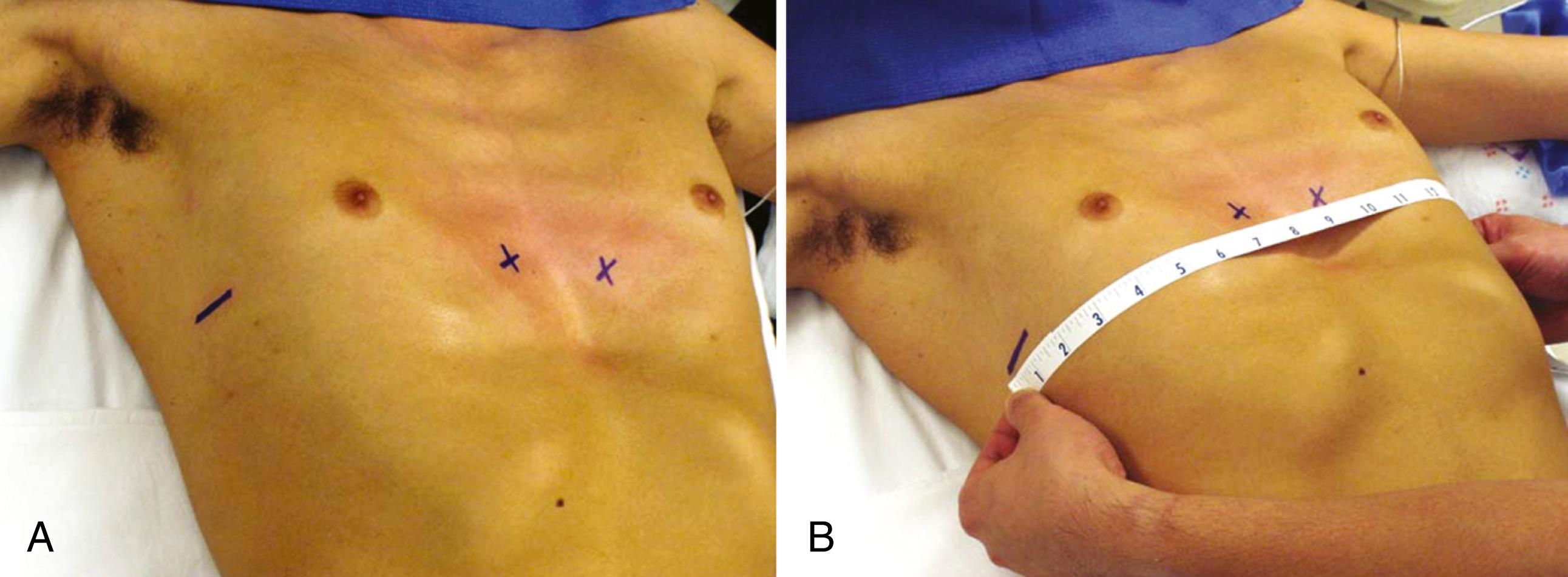
The surgeon is positioned on the patient’s right, and the surgical assistant is on the patient’s left. The deepest point of the pectus excavatum at the lower end of the sternum is marked. This mark sets the horizontal plane for bar insertion. At least one support bar should be under the bony sternum. If the bar is not under the sternum, there will not be correction of the deformity. It may be necessary to add a second bar superiorly or inferiorly, especially if the deepest point of the depression does not correspond to the inferior end of the sternum but to the xiphisternum or adjacent caudal costal cartilages. The intercostal spaces that are in the same horizontal plane as the deepest point of the pectus excavatum are marked with an X, slightly medial to the top of the pectus ridge. The Xs are the points where the bar will enter and exit the mediastinum. The proposed lateral thoracic incision sites are marked as a horizontal line from the anterior to the midaxillary lines ( Fig. 40-3A ). The chest is measured from the right midaxillary line to the left midaxillary line, and a Pectus Bar (Zimmer Biomet Inc., Jacksonville, FL) is selected on the basis of this measurement minus 1 inch (2 cm) ( Fig. 40-3B ).
Following preparation and sterile draping, the bar is bent into a smooth convex shape leaving a 2- to 4-cm flat section in the middle to support the sternum. (If desired, the manufacturer will bend the bar at the factory on the basis of the patient’s chest CT scan for an additional fee.) The bar should fit loosely on each side and not compress the chest wall muscles.
Currently, most pectus surgeons use one of two operative approaches for this procedure, and these two operative approaches will be discussed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here