Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
As explained in some detail in Chapter 26 , microbial keratitis is a particular type of corneal infiltrative event (CIE) characterised by the fact that replicating microorganisms are the cause. Microbial keratitis can be ‘self-limiting’, whereby it develops to a certain level of severity and then subsides, perhaps only resulting in mild discomfort at the peak of its development. A case of microbial keratitis may be self-limiting because the causative microorganisms cease replicating, possibly as a result of some action taken by the lens wearer, such as removing the lenses or instilling eye drops.
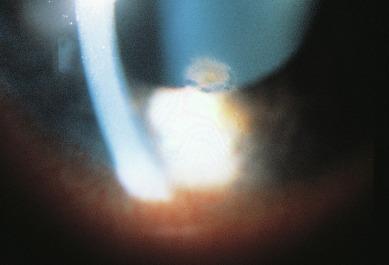
If not treated early (or not self-limiting), microbial keratitis can be progressive and potentially devastating to the cornea. It is the most severe reaction which can occur in response to contact lens wear. The patient may suffer from considerable pain and must incur the discomfort, cost and inconvenience associated with the acute management of this condition. In very severe cases, the patient may suffer partial or complete loss of sight. In perhaps the most severe case microbial keratitis ever recorded, the patient ended up with bilateral large, deep corneal ulcers and hypopyon. The right eye perforated spontaneously, and the patient developed secondary glaucoma and bilateral optic atrophy. All of this resulted in total bilateral blindness ( Fig. 27.1 ). Others have also reported cases of microbial keratitis leading to blindness resulting from continuous lens wear.
Microbial keratitis is defined as an inflammation of corneal tissue caused by direct infection by microbial agents, such as a bacteria, fungi, protozoa and viruses. Bacterial, fungal and protozoan keratitis can be directly caused by contact lens wear, and these forms of keratitis will be considered separately throughout this chapter. Contact lens wearers may coincidentally contract viral infections, such as epidemic keratoconjunctivitis (which is non-ulcerative) or herpes simplex keratitis (which is ulcerative), but there is no reason to believe that contact lens wear itself is a contributing factor to the development of the infection.
The terms ‘infectious keratitis’ and ‘microbial keratitis’ are essentially synonymous. The term ‘ulcerative keratitis’ has also been used as a synonym for microbial keratitis; however, this usage is not always correct because a given case of microbial keratitis may not necessarily be ulcerative, and an ulcerative keratitis may not necessarily be microbial.
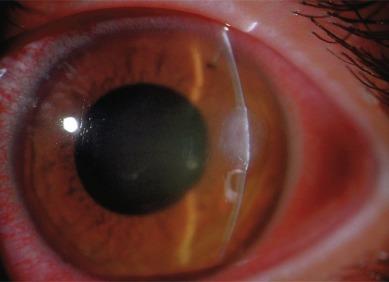
An early symptom of bacterial keratitis is a foreign body sensation in the eye associated with an increasing desire to remove the lenses. In the case of an actual foreign body, or that of other causes of lens-related ocular discomfort, lens removal leads to immediate relief. Continuing or worsening discomfort after lens removal should lead a clinician to suspect microbial keratitis. Associated symptoms include pain, eye redness, swollen lids, increased lacrimation, photophobia, discharge and loss of vision ( Fig. 27.2 ).

Besides the obvious signs of eye redness and lacrimation, an area of infiltration will typically be observed at the site of infection ( Fig. 27.3 ). In the early stages, infiltrates may be confined primarily to the epithelium. As the disease progresses, the stroma becomes increasingly hazy, and the epithelium above the infiltration begins to break down, leading to corneal staining of the ulcer and surrounding cornea ( Fig. 27.4 ). The appearance of bacterial keratitis in the early stages ( Figs. 27.3 and 27.4 ) is indistinguishable from a so-called contact lens peripheral ulcer (CLPU) (see Chapter 26 ).

Conjunctival redness may be initially confined to the limbal and bulbar regions adjacent to the field of infection, providing an important clue to the clinician as to its location. This clue is soon lost as the condition advances and the eye becomes more inflamed with circumlimbal conjunctival redness ( Fig. 27.2 ).
Bacterial keratitis can have a rapid and devastating time course. The initial focal ulcer (as shown in Figs. 27.3 and 27.4 ) can progress to form a swirling, circular, milky-white infiltrate ( Fig. 27.5 ). Worsening of the condition will lead to the formation of a creamy, pussy ulcer ( Fig. 27.6 ), anterior chamber flare, iritis and hypopyon. The time course from initial symptoms to the appearance in Figure 27.6 can be as rapid as 4 to 6 hours. A serous or mucopurulent discharge will be evident. If not properly treated, the stroma can melt away, leading to corneal perforation in a matter of days ( Fig. 27.1 ). A grading scale for microbial keratitis is displayed in Appendix A ; the sequence of grades also provides an illustration of the sequence of events as the keratitis increases in severity.

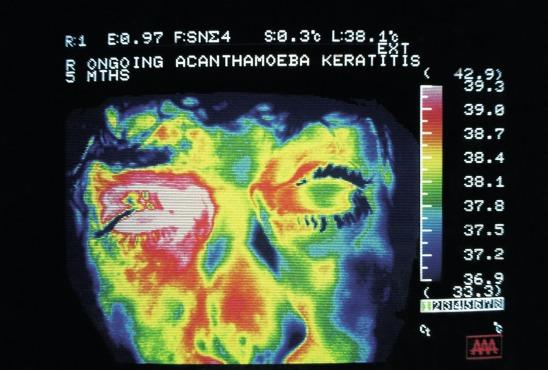
The time course of keratitis due to amoebic protozoa is not as rapid as for bacterial keratitis; typical signs include corneal staining, pseudo-dendrites, epithelial and anterior stromal infiltrates, which may be focal or diffuse, and a classic radial keratoneuritis ( Fig. 27.7 ) – the last being a circular formation of opacification which becomes apparent relatively early in the disease process. A fully developed corneal ulcer may take weeks to form. The pain associated with Acanthamoeba keratitis is so severe that it has been described as causing the patient to become almost suicidal. Figure 27.8 is an ocular thermogram of the face of patient suffering from contact lens–induced Acanthamoeba keratitis. As can be seen from the temperature scale to the right of this figure, the red and pink colouration around the right eye indicates higher temperatures, consistent with severe ocular inflammation.

Fungal keratitis also seems to develop over a more prolonged time course, in a similar manner to amoebic keratitis. Hu et al. presented a case series of patients with contact lens–associated fungal keratitis and reported a key symptom common to all cases reviewed – a sharp pain on removal of the lens from the eye after experiencing initial discomfort. This was followed by increased tearing, redness and photosensitivity. Vision deteriorated over a period of days. The form of presentation varied. One patient showed a round central stromal infiltrate, about 5 mm in diameter, corresponding to a deep corneal ulcer. In another patient, slit lamp examination with fluorescein staining showed a 4 × 3 mm, multi-lobed, central corneal infiltrate with complete loss of the overlying epithelium. One day later, the infiltrate appeared fluffy. In a third patient, a central corneal ulcer was seen with a paracentral opacity. There was also significant conjunctival and scleral injection and grade 2 cell and flare in the anterior chamber.
Ng et al. diagnosed 16 patients (17 eyes) with Fusarium keratitis associated with contact lens wear. One patient had bilateral involvement. Six patients had a central lesion; four had paraxial lesions; one had paraxial and peripheral lesions; and the rest had peripheral lesions.
Of the 66 patients with fungal keratitis examined by Khor et al., 30 had involvement of the right eye, 34 had involvement of the left eye, and two had bilateral eye involvement (68 infected eyes). Nine eyes (13.2%) had been treated with corticosteroid eye drops before the diagnosis of fungal keratitis. At presentation, the best-corrected Snellen visual acuity in the affected eye was 20/60 or better in 51 patients (75%), 20/80 to 20/200 in 11 patients (16.2%) and count fingers or worse in 6 patients (8.8%). Of the 68 eyes, 11 eyes (16.2%) had infiltrates which were described as central (involving the visual axis), 42 eyes (61.8%) had paracentral infiltrates, and 15 eyes (22.1%) had peripheral infiltrates. There were 25 eyes (36.8%) with classic fungal satellite lesions, five eyes (7.4%) with a ring infiltrate and 47 eyes (69.1%) with documented anterior chamber inflammation (consisting of anterior chamber cells or frank hypopyon) ( Fig. 27.9 ).
The hazy region of infiltration observed clinically in patients with microbial keratitis is presumed to be composed primarily of inflammatory cells but will also include the causative microorganisms, serum and proteins, as well as lipid which may leak from the limbal vessels.
Sankaridurg et al. developed an animal model (guinea pig) of endotoxin-mediated stromal infiltration. Histopathological examination of the affected regions of the stroma revealed focal or diffuse infiltration of polymorphonuclear leucocytes.
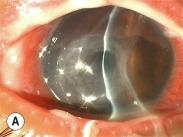
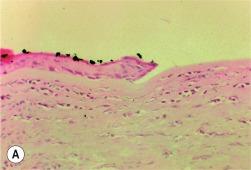
In an extraordinary study, Holden et al. obtained biopsy samples of the cornea and conjunctiva of three patients suffering from low-grade contact lens–associated keratitis. All three patients were using extended-wear hydrogel contact lenses. The diameter of the three infiltrates ranged from 0.3 to 0.6 mm. Histopathological examination of the corneal sections revealed a focal area of epithelial loss surrounded by a severely attenuated epithelium in all three patients ( Fig. 27.10 A ). Bowman’s layer appeared to be intact and of normal thickness in two patients, but there was a localised area of loss in the other patient ( Fig. 27.10 B). The anterior corneal stroma was infiltrated with numerous polymorphonuclear leucocytes beneath the area of epithelial compromise ( Fig. 27.10 C). The conjunctival epithelium appeared normal, and diffuse inflammatory cell infiltration, predominantly with mononuclear cells, was observed in the conjunctival stroma.
Konstantopoulos et al. demonstrated the utility of anterior segment optical coherence tomography for assessing the morphological characteristics of corneal pathological changes during the course of microbial keratitis. Seven patients (eyes) with suspected microbial keratitis underwent standard clinical examination and treatment based on slit lamp clinical examination findings. Anterior segment optical coherence tomography scanning was performed on presentation and at two follow-up appointments. All scans were carried out with the scanning beam passing through the centre of the infiltration and at a specific meridian. Examination was carried out by the same operator.
Corneal infiltration was imaged as a hyper-reflective area in the corneal stroma on high-resolution anterior segment optical coherence tomography scans. Retro-corneal pathological features and anterior chamber inflammatory cells could be imaged.
Corneal and infiltrate thickness could be measured with callipers in six cases. The depth of infiltrates into the cornea was measured as ranging from 180 to 590 μm (the latter measurement essentially representing full corneal thickness). In one case, corneal and infiltrate thicknesses could not be measured because of a thick inflammatory plaque attached to the endothelium. In this case, the width of the plaque was measured on serial scans. The authors concluded that anterior segment optical coherence tomography imaging provides a range of parameters which can be used to assess microbial keratitis and the treatment response objectively.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here