Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Despite the widespread availability of effective antiretroviral regimens in the United States, opportunistic infections are still seen frequently at many health care facilities, especially those serving populations with poor access to health care.
The annual incidence of new diagnoses of HIV in the United States was about 34,000 cases in 2019, representing about a 17% decline since 2016. Among the estimated 1.2 million people living with human immunodeficiency virus (HIV) in the United States, nearly 87% know they are infected, about 75% have received some HIV medical care, and about two thirds are virally suppressed.
About 20% of persons diagnosed with HIV in the United States have a CD4 lymphocyte count less than 200 cells/μL at the time of diagnosis. As a result, a substantial number of people living with HIV in the United States continue to be susceptible to a wide range of opportunistic infections because either they do not know they are infected with HIV and/or they are not receiving effective care.
Globally, the prevalence of HIV is about 38 million adults, with an annual incidence of 1.5 million new infected adults. Of all people worldwide living with HIV, about 85% know their status, about 75% are accessing treatment, and about 65% are virally suppressed.
Even for patients who initiate antiretroviral therapy and adhere carefully to their regimens, opportunistic infections can occur in the first few weeks or months before immunity is substantially improved, as measured by the circulating CD4 count and the HIV viral load. Immunity improves substantially as soon as the viral load is suppressed below the level of assay detection. Although the level of infections risk is substantially reduced once HIV viral suppression is achieved, the absolute risk remains elevated for most opportunistic infections until the CD4 count rises above 50 to 200 cells/μL, depending on the specific opportunistic infection. In addition, some opportunistic infections (especially tuberculosis [ Chapter 299 ], pneumococcal bacteremia [ Chapter 268 ], and dermatomal herpes zoster [ Chapter 346 ]) occur despite HIV viral suppression and CD4 counts above 200 cells/μL.
As patients with HIV live longer, they are developing increasing chronic morbidity and mortality due in part to latent viruses such as human papillomavirus ( Chapter 344 ), hepatitis C virus ( Chapter 135 ), hepatitis B virus ( Chapter 135 ), JC virus ( Chapter 341 ), and human herpesvirus 8 (HHV-8) ( Chapter 359 ). The progression of hepatitis C and hepatitis B virus liver disease is accelerated in HIV-infected patients compared with HIV-uninfected patients, thereby leading to earlier development of cirrhosis, liver failure, and hepatoma. Human papillomavirus is associated with high rates of cervical carcinoma and anal carcinoma, as well as oral cancers. In people living with HIV, JC virus is associated with progressive neurologic disease. Human herpesvirus-8 is associated with Kaposi sarcoma ( Chapter 359 ), multicentric Castleman disease ( Chapter 171 ), and primary effusion cell lymphoma ( Chapter 171 ). The consequences of chronic inflammation related to active or latent HIV viral reservoirs also appears to be a factor causing noninfectious complications such as accelerated atherosclerotic, cerebrovascular, renal, and hepatic diseases.
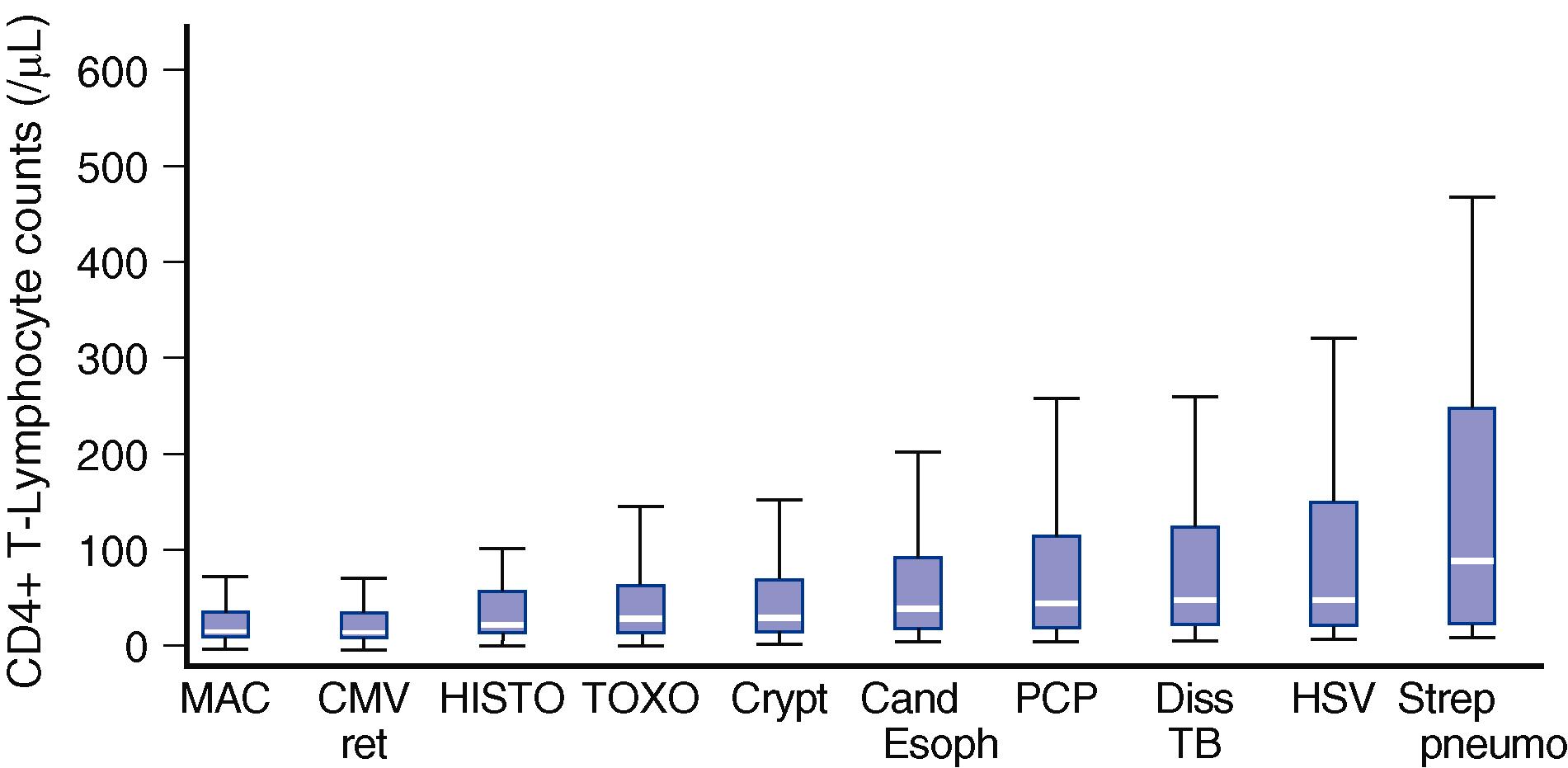
The number of circulating CD4 cells is a sensitive and specific indicator of patient prognosis and of susceptibility to specific opportunistic infections for persons with HIV/AIDS ( Fig. 358-1 ). Although CD4 cells are important to host defenses in all patients, the circulating CD4 count is much more useful in predicting susceptibility to infection for patients with HIV infection than in any other patient population. The blood HIV viral load is also an independent predictor of host susceptibility to opportunistic infection, but it is not nearly as sensitive and specific for estimating survival or for assessing susceptibility to opportunistic infection as are CD4 counts.
The specific opportunistic infections that an HIV-infected person develops are influenced not only by the person’s individual immunologic defects but also by environmental exposures. For instance, in areas of the world where exposure to Mycobacterium tuberculosis is common, tuberculosis is the major infectious cause of morbidity and mortality in people with HIV infection regardless of CD4 count, although the incidence of disease increases as the CD4 count declines. In contrast, however, in areas of the world such as the United States where tuberculosis exposure is uncommon, tuberculosis is rarely seen except in immigrants and when people living with HIV are exposed to high-risk populations, such as persons in prisons or homeless shelters. Severe manifestations of endemic fungi (e.g., cryptococcosis, histoplasmosis, and coccidiomycosis) vary in different geographic regions. Similarly, in many areas of the developing world, HIV-positive individuals are exposed to salmonella, toxoplasma, Cryptococcus, Trypanosoma cruzi , and Talaromyces more frequently than in the United States, so these diseases are more common in HIV-infected persons in those areas than in the United States.
Studies of the human microbiome provide an interesting perspective on factors that could influence the range of pathogens causing diseases among people with HIV infection. For example, HIV-infected patients with lower CD4 counts have demonstrable changes in their respiratory microbiome compared to other patient populations—changes that tend to reverse with effective HIV treatment.
Behavioral factors are also important determinants of which opportunistic infections occur. Individuals who inject drugs ( Chapter 365 ) are more likely to be infected with hepatitis C virus and hepatitis B virus than are patients without injection drug use histories; they are also more likely to develop certain non-opportunistic processes, such as Staphylococcus aureus ( Chapter 267 ) soft tissue infections, bacteremia, and endocarditis. Men who have sex with men who develop proctitis or colitis are more likely to have rectal disease due to Neisseria gonorrhoeae ( Chapter 275 ), Chlamydia trachomatis ( Chapter 294 ; especially lymphogranuloma venereum strains), MPox ( Chapter 343 ), or Shigella ( Chapter 285 ) than individuals who are not men-who-have-sex-with-men.
The pathogens that cause active disease in persons with HIV infection ( Table 358-1 ) may be organisms that were acquired recently or may represent reactivation of latent organisms acquired months or years previously. Mycobacterium tuberculosis ( Chapter 299 ), Pneumocystis jirovecii ( Chapter 313 ), Trypanosoma cruzi ( Chapter 318 ), Leishmania donovani ( Chapter 319 ), Histoplasma capsulatum ( Chapter 308 ), Coccidioides immitis ( Chapter 308 ), herpes simplex ( Chapter 345 ), herpes zoster ( Chapter 346 ), and cytomegalovirus ( Chapter 347 ) are examples of pathogens that can cause acute disease either soon after exposure or after many months or years of latency as determined by molecular typing or clinical epidemiology. Thus, pathogens need to be considered as possible etiologic agents despite exposure that may have occurred in the distant past.
| OPPORTUNISTIC PATHOGEN | COMMON CLINICAL MANIFESTATIONS |
|---|---|
| Bacterial enteric infection (e.g., salmonella) ( Chapter 270 ) | Diarrhea, colitis, sepsis (salmonella) |
| Bartonellosis ( Chapter 291 ) | Bacillary angiomatosis, hepatic peliosis |
| Candidiasis (mucocutaneous; Chapter 310 ) | Mucosal thrush (oral, esophageal, vaginal, rectal) |
| Chagas disease ( Chapter 318 ) | Encephalitis, brain abscess |
| Coccidioidomycosis ( Chapter 308 ) | Pneumonia, sepsis |
| Community-acquired pneumonia ( Chapter 85 ) | Pneumonia, bacteremia |
| Cryptococcosis ( Chapter 309 ) | Meningitis, sepsis, pneumonia |
| Cryptosporidiosis ( Chapter 321 ) | Diarrhea, colitis |
| Cystoisosporiasis ( Chapter 324 ) | Diarrhea, colitis |
| Cytomegalovirus ( Chapter 347 ) | Retinitis, colitis, esophagitis |
| Hepatitis B virus ( Chapter 135 ) | Hepatitis, hepatocellular carcinoma |
| Hepatitis C virus ( Chapter 135 ) | Hepatitis, hepatocellular carcinoma |
| Herpes simplex virus ( Chapter 345 ) | Oral mucositis, cutaneous and perirectal ulcers |
| Histoplasmosis ( Chapter 308 ) | Sepsis, pneumonia, meningitis |
| Human herpesvirus-8 ( Chapter 359 ) | Multicentric Castleman disease, primary effusion cell lymphoma, Kaposi sarcoma |
| Human papillomavirus ( Chapter 344 ) | Cervical, anal, and oral carcinoma |
| JC virus (progressive multifocal leukoencephalopathy; Chapter 341 ) | Encephalitis |
| Leishmaniasis ( Chapter 319 ) | Cutaneous, mucocutaneous, and disseminated disease |
| Malaria ( Chapter 316 ) | Malaria |
| Microsporidiosis ( Chapter 324 ) | Diarrhea |
| Mycobacterium avium complex ( Chapter 300 ) | Lymphadenopathy, disseminated disease |
| Mycobacterium tuberculosis ( Chapter 299 ) | Pneumonia, meningitis, pericarditis, lymphadenitis, disseminated disease |
| Pneumocystis jirovecii ( Chapter 313 ) | Pneumonia |
| Syphilis ( Chapter 295 ) | Genital ulceration, uveitis, otitis, neurologic disease |
| Talaromycosis ( Chapter 308 ) | Pulmonary, cutaneous, disseminated disease |
| Toxoplasma gondii ( Chapter 320 ) | Brain abscess, disseminated disease |
| Varicella-zoster virus ( Chapter 346 ) | Dermatomal zoster, carotid vasculitis, stroke |
Opportunistic infectious diseases in people with HIV and AIDS often have clinical manifestations and natural histories that are different than in other immunosuppressed patients. In patients with AIDS, for example, Pneumocystis pneumonia ( Chapter 313 ) is much more likely to manifest with subacute symptoms over many days or weeks compared with the more acute presentation over a few days in HIV-uninfected cancer patients who are receiving chemotherapy, patients receiving high-dose corticosteroids, or transplant recipients. When patients are diagnosed with Pneumocystis pneumonia, patients with AIDS at initial presentation are usually less hypoxemic and have less impressive radiographic infiltrates despite the longer duration of symptoms before diagnosis. The number of organisms found in sputum or bronchoalveolar lavage specimens is also greater in patients with AIDS than in other immunosuppressed patients, despite the less severe symptoms. Patients with AIDS also are more likely to develop treatment-limiting toxicity associated with trimethoprim-sulfamethoxazole and to have multiple relapses if they are not placed on chemoprophylaxis or chronic suppressive therapy.
For infections due to Toxoplasma gondii ( Chapter 320 ), patients with HIV/AIDS characteristically develop toxoplasma encephalitis, whereas other immunosuppressed populations more often develop disseminated visceral disease involving the liver, spleen, or kidneys. Similarly, cytomegalovirus in patients with HIV/AIDS most often causes retinitis and colitis, whereas cytomegalovirus retinitis is relatively uncommon but pneumonia is frequent in patients undergoing hematopoietic stem cell or solid organ transplantation.
Some pathogens that frequently cause disease among patients with HIV/AIDS had rarely been recognized as causes of life-threatening human disease before the HIV/AIDS epidemic. Examples include Mycobacterium avium complex ( Chapter 300 ), Cryptosporidium ( Chapter 321 ), Microsporidium ( Chapter 324 ), and Bartonella ( Chapter 291 ). Conversely, some pathogens that are associated with disease in other immunosuppressed patients, including patients with compromised cell-mediated immunity, are rarely seen in patients with HIV/AIDS. Examples include Listeria monocytogenes ( Chapter 272 ) disseminated herpes simplex, ( Chapter 345 ), disseminated herpes zoster ( Chapter 346 ), and disseminated Strongyloides stercoralis ( Chapter 327 ). The reasons why some pathogens are unexpectedly frequent or unexpectedly unusual despite similar environmental exposures have not been fully elucidated.
With better antiretroviral treatment and prophylaxis against opportunistic infection, the spectrum of clinical opportunistic infections has evolved. For example, disseminated Mycobacterium avium complex, cytomegalovirus retinitis, cryptosporidiosis, and microsporidiosis now occur far less frequently in the United States and Western Europe than before. Much of the shift is undoubtedly due to earlier diagnosis of HIV before severe immunosuppression occurs as well as to better access to effective and durable antiretroviral therapy. In developing countries, where patients more often still present with full-blown AIDS, however, tuberculosis, cryptococcal meningitis, pneumococcal disease, and bacterial and protozoal enteritis remain major AIDS-related opportunistic complications.
For an infection in any patient population, management is likely to be more effective and to be associated with fewer complications if the specific microbial cause is conclusively identified, the appropriate specific therapy is started quickly, and unnecessary drugs are avoided. For patients with HIV infection, such an approach is especially appropriate given the broad range of opportunistic and nonopportunistic infections that could cause a particular syndrome ( Table 358-2 ), as well as the noninfectious causes, including drug toxicities, that can masquerade as infections.
| INFECTIOUS SYNDROME | OPPORTUNISTIC OR NONOPPORTUNISTIC CAUSE | EMPIRIC THERAPY |
|---|---|---|
| Diarrhea/colitis | Clostridium difficile, Salmonella species, Shigella species, Cryptosporidia, Microsporidia | None unless persistent or severe or bloody; then consider a fluoroquinolone |
| Pneumonia | Pneumococcus, community-acquired viruses, atypical bacteria, pneumocystis, Mycobacterium tuberculosis , cryptococcus, histoplasmosis | Azithromycin plus ceftriaxone plus trimethoprim-sulfamethoxazole |
| Meningitis | Pneumococcus, cryptococcus, meningococcus | Ceftriaxone plus liposomal amphotericin B |
| Retinitis | Cytomegalovirus | IV ganciclovir, oral valacyclovir, or oral famciclovir |
| CNS mass lesion | Toxoplasma, lymphoma, cryptococcus, aerobic and anaerobic bacteria, Mycobacterium tuberculosis | Trimethoprim-sulfamethoxazole |
| CNS = central nervous system; HIV = human immunodeficiency virus. | ||
The diagnostic tests to identify specific opportunistic infections are usually no different in patients with HIV infection or AIDS than in other patients. For the evaluation of a febrile patient with HIV infection and a CD4 lymphocyte count less than 200 cells/μL, blood cultures for routine bacteria and fungi, a serum cryptococcal antigen test, a Toxoplasma IgG test, and a syphilis serologic test often provide a useful baseline. If the patient has pulmonary dysfunction, Gram stain and routine culture of expectorated or induced sputum are usually useful. If a history of appropriate geographic exposure is present, serum and urine histoplasma antigen and Coccidioides antibodies also can be informative.
Conversely, some clinical microbiologic tests that are useful in other immunosuppressed patient populations are not necessarily useful to diagnose opportunistic infections in patients with HIV infection. For example, blood polymerase chain reaction (PCR) for cytomegalovirus is very useful in patients who have received hematopoietic stem cell transplants, because their positive and negative predictive values are high. In patients with HIV infection, however, cytomegalovirus PCR positivity correlates mainly with the degree of immunosuppression and does not have sufficient accuracy to be useful for assessing the cause of end organ disease. Blood PCR tests for Epstein-Barr virus, varicella zoster virus, or herpes simplex virus also are not useful in most circumstances for similar reasons.
An increasing number of laboratories are offering molecular tests for opportunistic pathogens, but care must be taken to be certain that these tests are not detecting colonization rather than true infection. People living with HIV may be colonized with more pathogens and for longer periods of time than patients without HIV infection. For example, PCR for Pneumocystis in bronchoalveolar lavage may have excellent negative predictive value, but its positive predictive value is low because some immunosuppressed patients are asymptomatically colonized with Pneumocystis .
Imaging is an important aspect of patient evaluation. Patients with HIV infection may have pathologic processes despite a paucity of symptoms or even normal readings on routine chest radiographs, for example. A computed tomography (CT) of the lungs may reveal unexpected pathologic findings such as diffuse interstitial infiltrates suggestive of Pneumocystis pneumonia despite the absence of cough, shortness of breath, or oxygen desaturation. Such a finding could lead to ordering an induced sputum or bronchoalveolar lavage and establishing the diagnosis of an infection at a time when disease is mild and the likelihood of successful treatment is high. CT of the abdomen also should be considered in patients with prolonged fever or wasting and low CD4 counts even in the absence of abdominal symptoms, because such a study may reveal unexpected adenopathy or organ infiltration that could be readily biopsied. Positron emission tomography and nuclear scans may have roles for identifying the infectious cause of clinical syndromes, but the use of such scans is not well standardized, and the results are not organism specific.
Effective therapy for opportunistic infections in people living with HIV may require longer courses of treatment than in immunocompetent patients, especially if immunity is not reconstituted by antiretroviral therapy. Moreover, Pneumocystis pneumonia, cytomegalovirus retinitis, Mycobacterium avium complex bacteremia, and cryptococcal meningitis often relapse or recur if patients with HIV/AIDS are not either reconstituted immunologically with antiretroviral therapy or treated with chronic suppressive therapy for their specific opportunistic infection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here