Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The most common pulmonary neoplasm is a metastasis from outside the lungs. Based on autopsy data, the lungs are involved by metastases in 25% to 55% of malignant diseases. In up to 25% of those cases, the pulmonary parenchyma and pleura are the only sites of distant spread. Because the majority of pulmonary metastases occur at a late stage and often are not sampled, the most common lung tumor encountered by a practicing pathologist is a primary bronchogenic carcinoma. Distinguishing a primary from a secondary pulmonary neoplasm requires experience and skill. This chapter provides a concise discussion of the pathobiologic principles and clinicoradiologic findings of metastases in the lungs and offers a sociotechnological framework for the pathologist to identify such lesions with a high level of certainty.
Much of what we know about pulmonary metastatic disease has been learned through observational studies, including histologic and cytologic assessments and clinical data. Extrapulmonary malignancies may spread to the lungs by metastasis through the vascular system or the lymphatic system, or by direct extension from a site adjacent to the lungs. Primary lung cancers may spread to different parts of the lungs by vascular metastasis or aerogenously by dissemination through the alveolar pores of Kohn. The clinical and radiologic features of a specific malignancy depend on these avenues of spread.
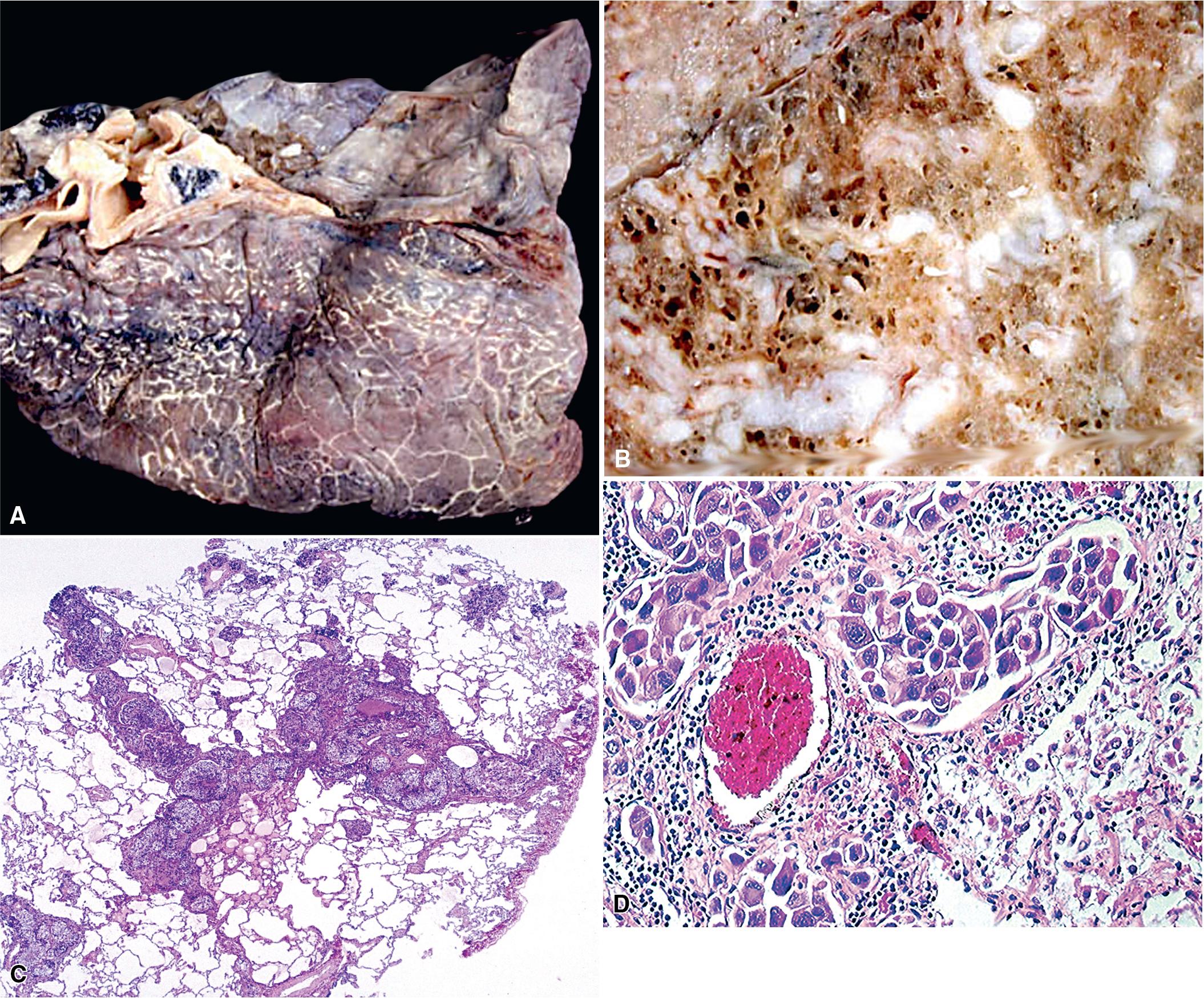
Hematogenous spread is the most common form of pulmonary metastasis as the lungs receive the entire cardiac output and contain a huge capillary bed. The detailed principles underlying vascular metastasis have been outlined elsewhere. Malignant tumors may contain clones of cells with differing metastatic potential with some clones acquiring the ability to enter the bloodstream as microemboli. At selected distant sites, these malignant clonal cells adhere to the endothelial basement membranes and extravasate into the extracellular matrix to form metastatic deposits. In this paradigm, a micrometastasis proliferates to yield a larger mass, which later, often as long as several years, may become visible radiographically or be associated with clinical signs and/or symptoms. Most pulmonary metastases show nests of neoplastic cells surrounded by a variable quantity of fibrous stroma. At this stage, no malignant cells typically are found in the pulmonary arterial, venous, or capillary system unless they arrive later in a newer microembolus.
The rate at which potentially metastasizing cellular subclones develop in primary tumors varies considerably. The probability that such lesions will spread hematogenously depends on both tumor-related factors and conditions in the milieu of the host tissues. Some malignancies, such as osteosarcoma, often shed micrometastases before the primary tumor is detected clinically. Other tumors may show metastasis only very late in their biologic evolution.
The clinical presentation of patients with hematogenous pulmonary metastases is variable. Many patients have no symptoms and lesions are detected only through imaging studies undertaken for cancer staging purposes or for surveillance during cancer treatment. The radiographic appearance of a metastatic malignancy to the lung may show a single central or peripheral mass, multiple central or peripheral masses, diffuse infiltrates, or a combination of the latter two possibilities. Metastases tend to manifest as having smooth or rounded contours radiographically in contrast to much more irregular shapes of primary carcinomas. If a patient is symptomatic, the clinical findings reflect the location and extent of the metastatic deposits and commonly include chest pain, dyspnea, cough, hemoptysis, and wheezing.
In addition to microembolization, extrapulmonary tumors may spread to the lungs as macroscopic emboli that involve large or medium-sized pulmonary arteries. Large-vessel tumor emboli may cause acute heart failure, sudden death, rapidly evolving pulmonary hypertension, and pulmonary infarcts. The tumors that most commonly give rise to macroscopic emboli are those associated with major systemic veins (e.g., renal or hepatic carcinomas invading the renal and hepatic veins) and primary tumors of the heart (myxomas and sarcomas).
In rare cases, hematogenous spread consists of tumor-related thrombotic pulmonary microangiopathy , with occlusive luminal tumor plugs in arterioles and capillaries without interstitial involvement or the formation of masses. Neoplasms that may show this pattern of metastatic spread include carcinomas of the breast, gastrointestinal tract, liver, pancreas, uterus, gallbladder, prostate gland, and ovary. Soares et al. reported that most malignant tumors that occlude small pulmonary vascular channels also may contain malignant cells within larger vessels. Patients with metastatic microvascular occlusion typically present with severe pulmonary hypertension, progressive dyspnea, and cor pulmonale. ,
As a general rule, all caval venous blood flows through the lungs, and portal venous return passes through the liver. Consequently, depending on the primary site of the tumor, metastases preferentially are seen in one of these two organs. Malignant neoplasms that arise in sites with other pathways of vascular drainage (e.g., prostatic tumors preferentially shed into the paravertebral venous plexus) infrequently involve the lungs secondarily. Arterially borne metastases to the lungs are relatively rare and are usually mediated by the bronchial arteries. The most common source of such lesions is a primary lung cancer that has gained access to the pulmonary venous system.
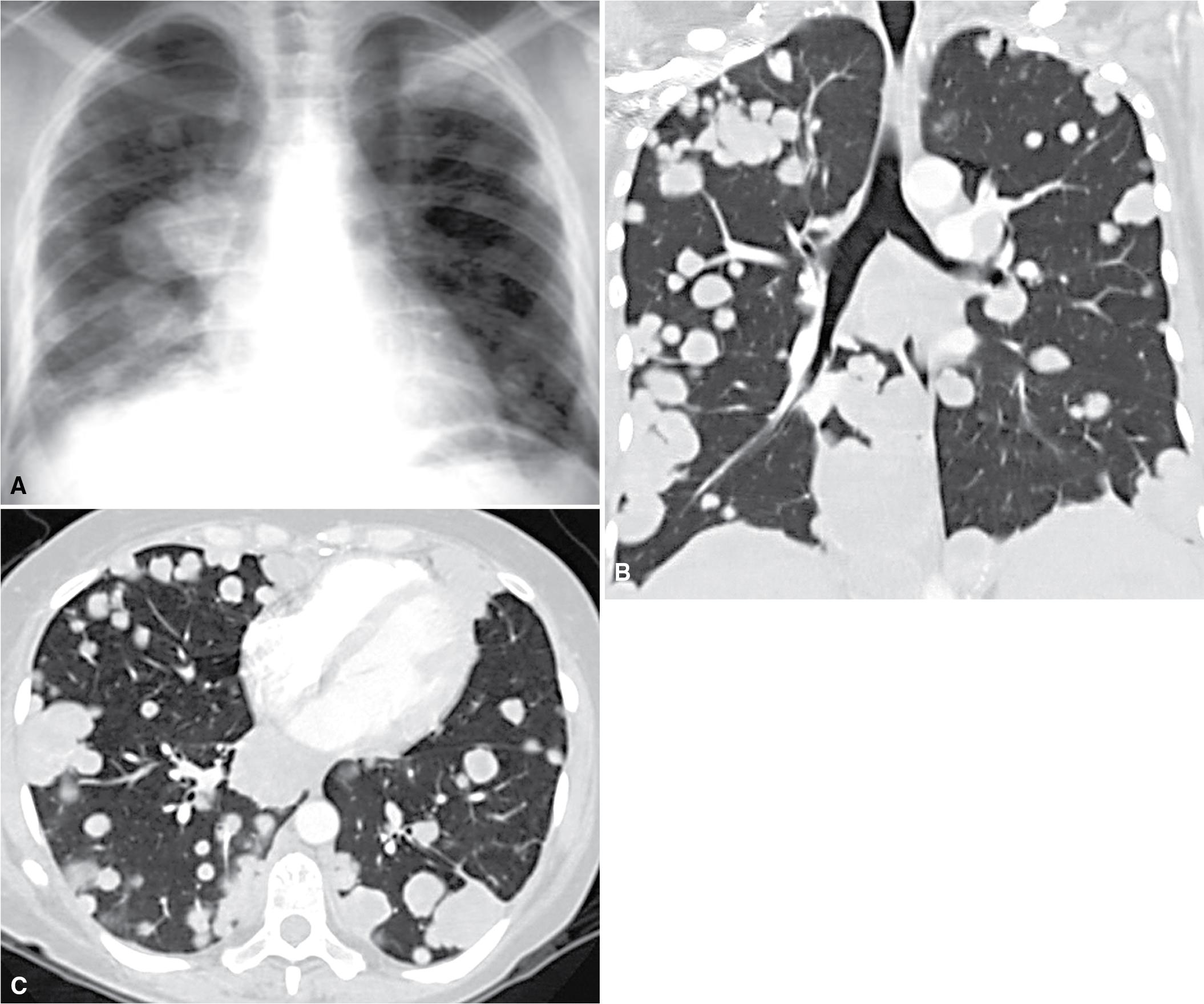
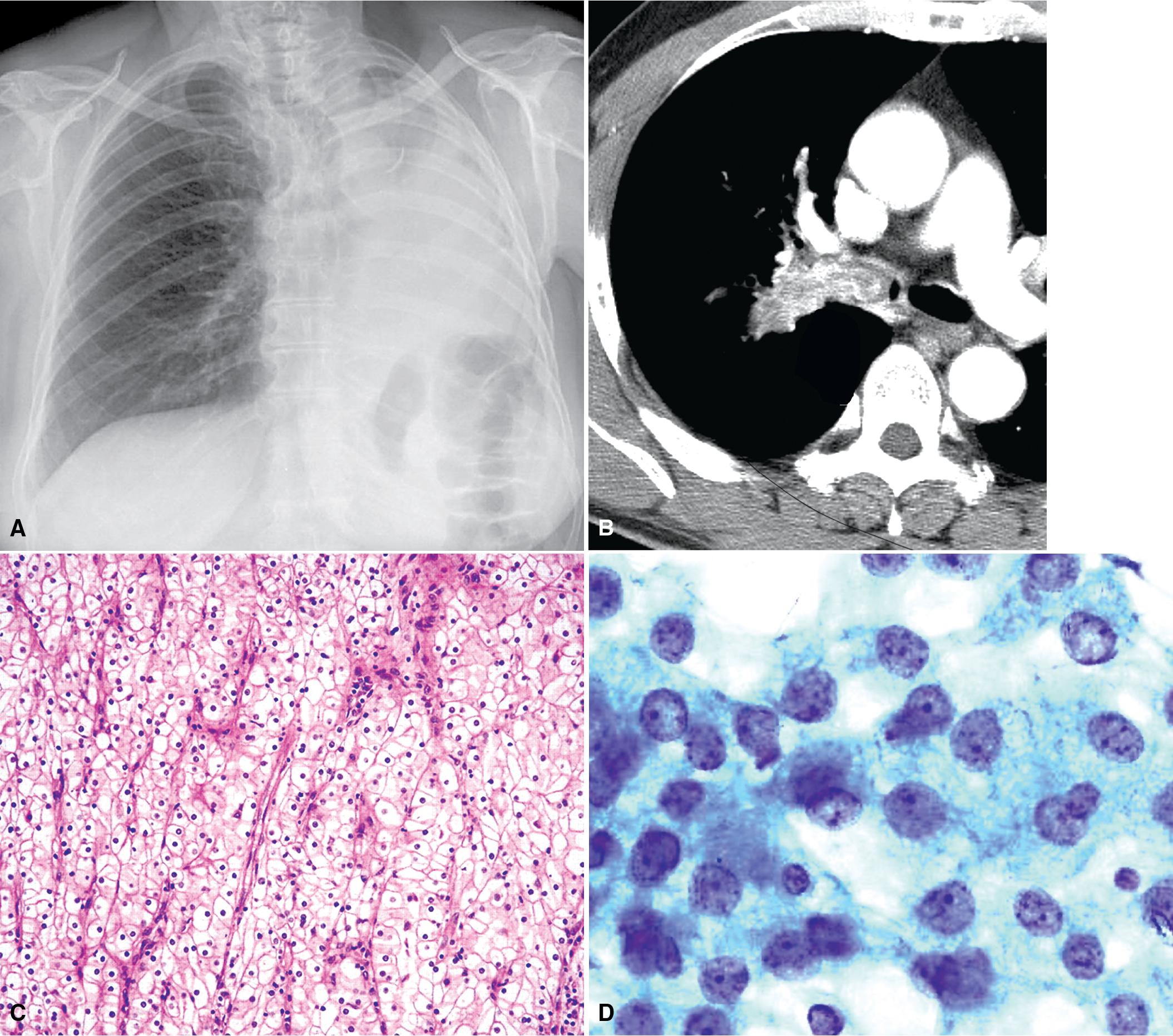
Hematogenous metastasis in the lung is associated with a spectrum of radiologic findings. The most common roentgenographic appearance is that of multiple, bilateral, and variably sized masses ( Figs. 18.1–18.3 ). A solitary intraparenchymal nodule occasionally is seen. The metastatic implants usually appear in the mid- to lower lung fields, where the parenchymal perfusion is greatest. In up to 90% of patients with bilateral secondary disease, the lesions are peripheral and subpleural ( Fig. 18.4 ). , The variability in the size of the metastatic nodules is associated with the different temporal ages of the lesions, dissimilar growth rates, and other factors. At the time of detection, secondary malignancies usually measure less than 3 to 4 cm in diameter, which is smaller than the typical primary pulmonary carcinomas. On serial radiologic examinations, metastases tend to enlarge more rapidly than primary carcinomas, excluding small cell carcinomas.

Tumors involving small vessels may produce linear parenchymal infiltrates. Patients who have both masses and metastases in small vessels or lymphatic spaces present with opacities and linear streaks. Embolic tumors in the large pulmonary arteries may show the radiographic appearance of an infarct, with a wedge-shaped peripheral zone of consolidation and a pleural effusion.
Solitary metastases in the lungs comprise up to 10% of all malignant tumors. Filderman and coworkers suggested that solitary metastatic lesions larger than 5 cm in diameter most likely originated in the breast, kidney, or soft tissue. Metastasis in the form of a solitary mass on plain films may appear as multiple contiguous or coalescent masses on computed tomography. Quint and colleagues reported that, statistically, patients with carcinomas of the head and neck, bladder, breast, cervix, bile ducts, esophagus, ovary, prostate gland, or stomach were more likely to have a solitary metastasis to the lung than a new primary bronchogenic tumor, even when a significant period had elapsed after diagnosis of the extrapulmonary neoplasms. On the other hand, patients with a history of malignant melanoma, sarcoma, or malignant germ cell tumor more likely had a second primary malignancy of the lung under the same circumstances.
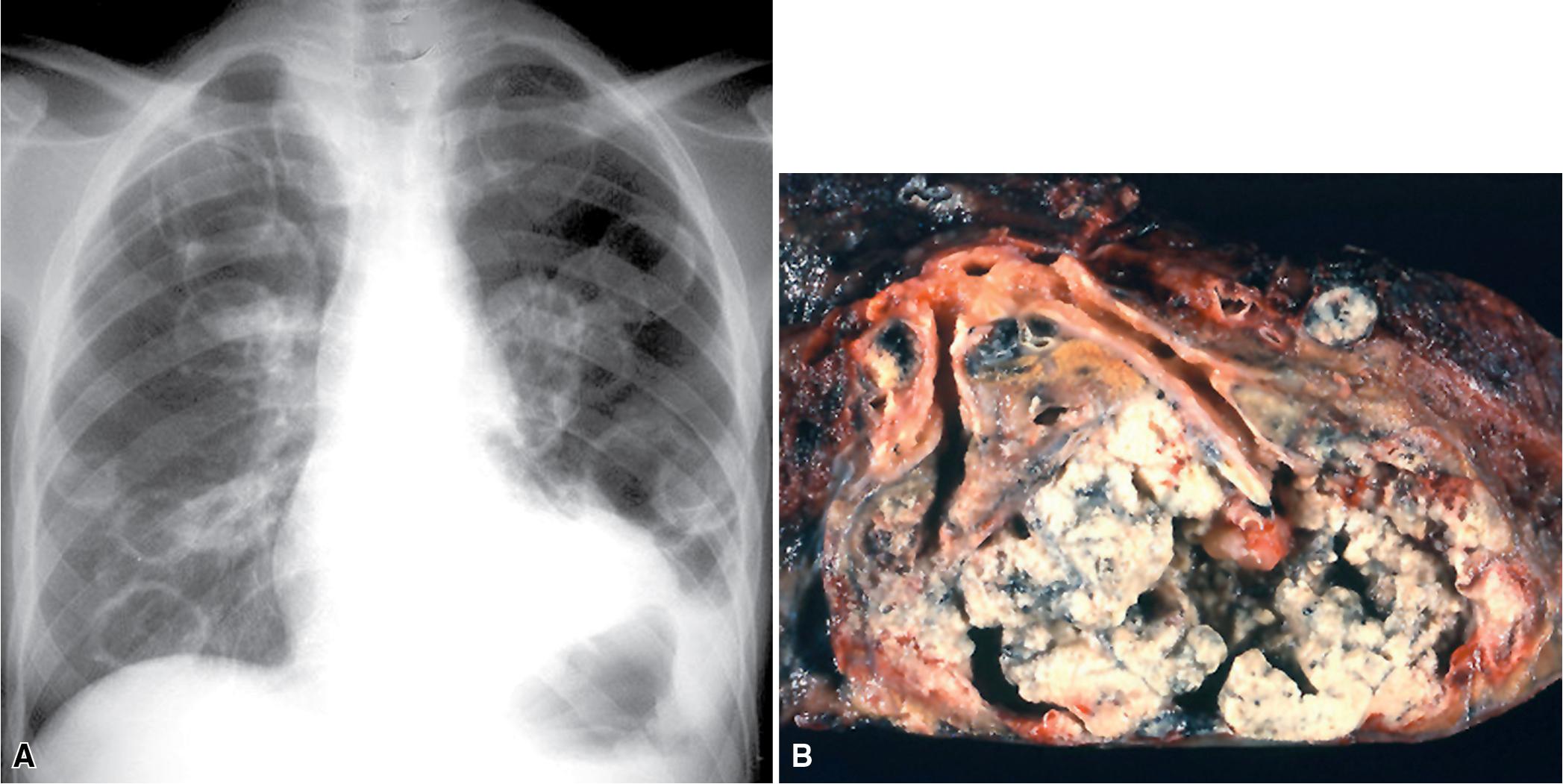
Large metastatic foci may undergo cavitation or be associated with a pneumothorax or a bronchopleural fistula ( Fig. 18.5 ). The most common secondary tumor that cavitates is a squamous cell carcinoma, often originating in the head and neck and morphologically showing extensive keratinization. Metastatic sarcoma and adenocarcinoma also may exhibit cavitation. Destructive pleural growth of a metastatic tumor may cause a pneumothorax or a transpleural fistulae, seen most frequently in pediatric mesenchymal malignancies, such as an osteosarcoma.
Lymphogenous metastasis accounts for 5% to 8% of pulmonary metastases, although one study reported that up to 56% of pulmonary metastases were lymphogenously mediated. Most patients with lymphatic-borne lung metastases have a poor prognosis, with 90% of patients dying within 6 months.
The radiographic appearance of lymphangitic metastasis is variable and in 50% of cases, chest x-rays show no apparent abnormality. Yang and Lin described four radiologic patterns when lymphangitic metastasis are detectable on chest x-ray :
Bilateral linear infiltrates without hilar enlargement or intrapulmonary masses
Hilar masses with centripetal parenchymal extension, seen most commonly in patients with cervical, gastric, and breast cancers ( Fig. 18.6 )
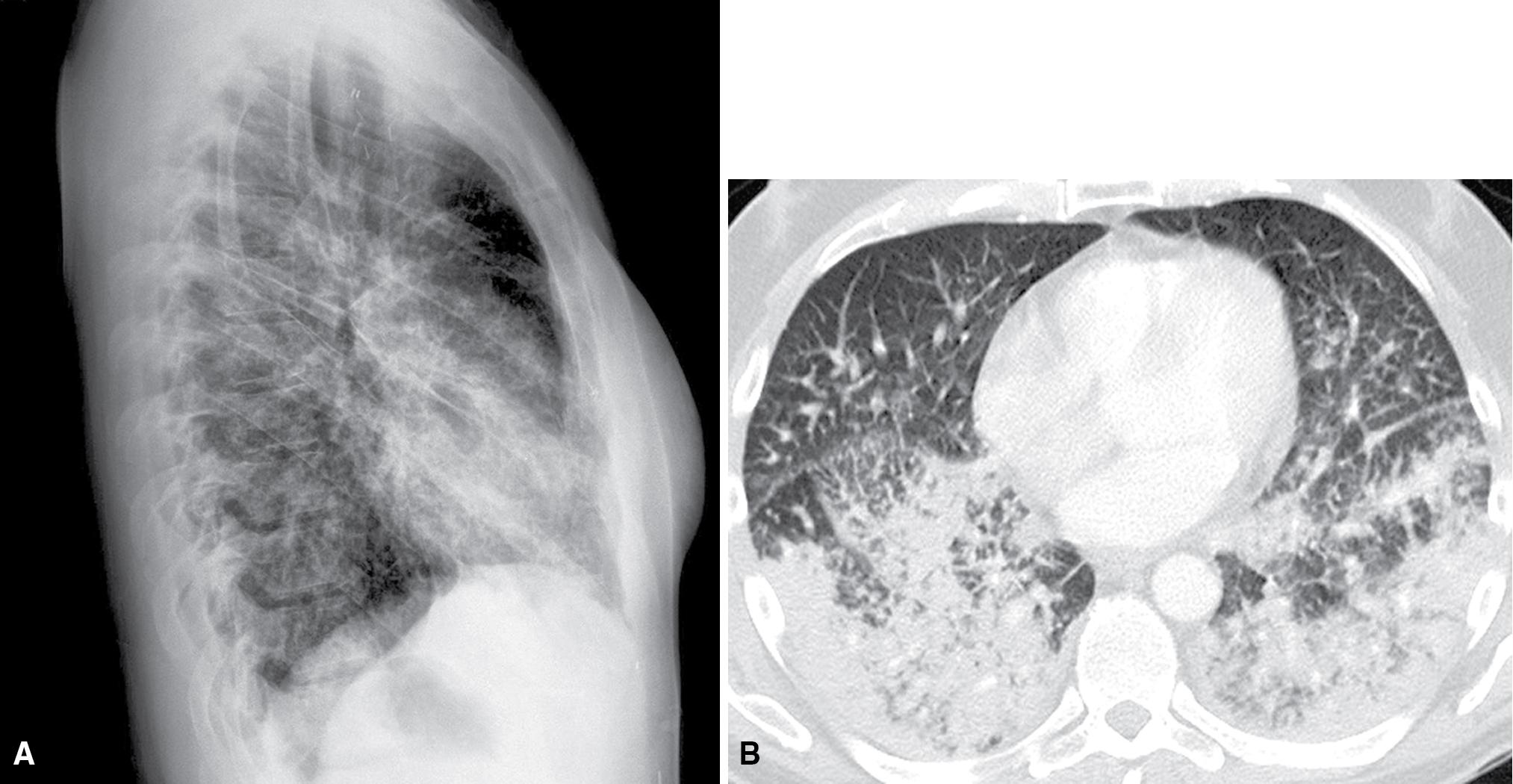
Focal linear infiltration of the parenchyma associated with a central primary tumor
Parenchymal radiations from a peripheral primary tumor
In first two metastatic patterns, pleural and/or hilar lymph nodal involvement may be seen. More than 90% of these cases are metastatic adenocarcinomas. It is estimated that fewer than 1% of patients with pulmonary metastases from tumors arising outside the thorax also have hilar adenopathy. Although this figure may appear low, hilar lymphadenopathy in patients with secondary pulmonary malignancies is not uncommon in absolute terms because of the high prevalence of patients with metastatic disease.
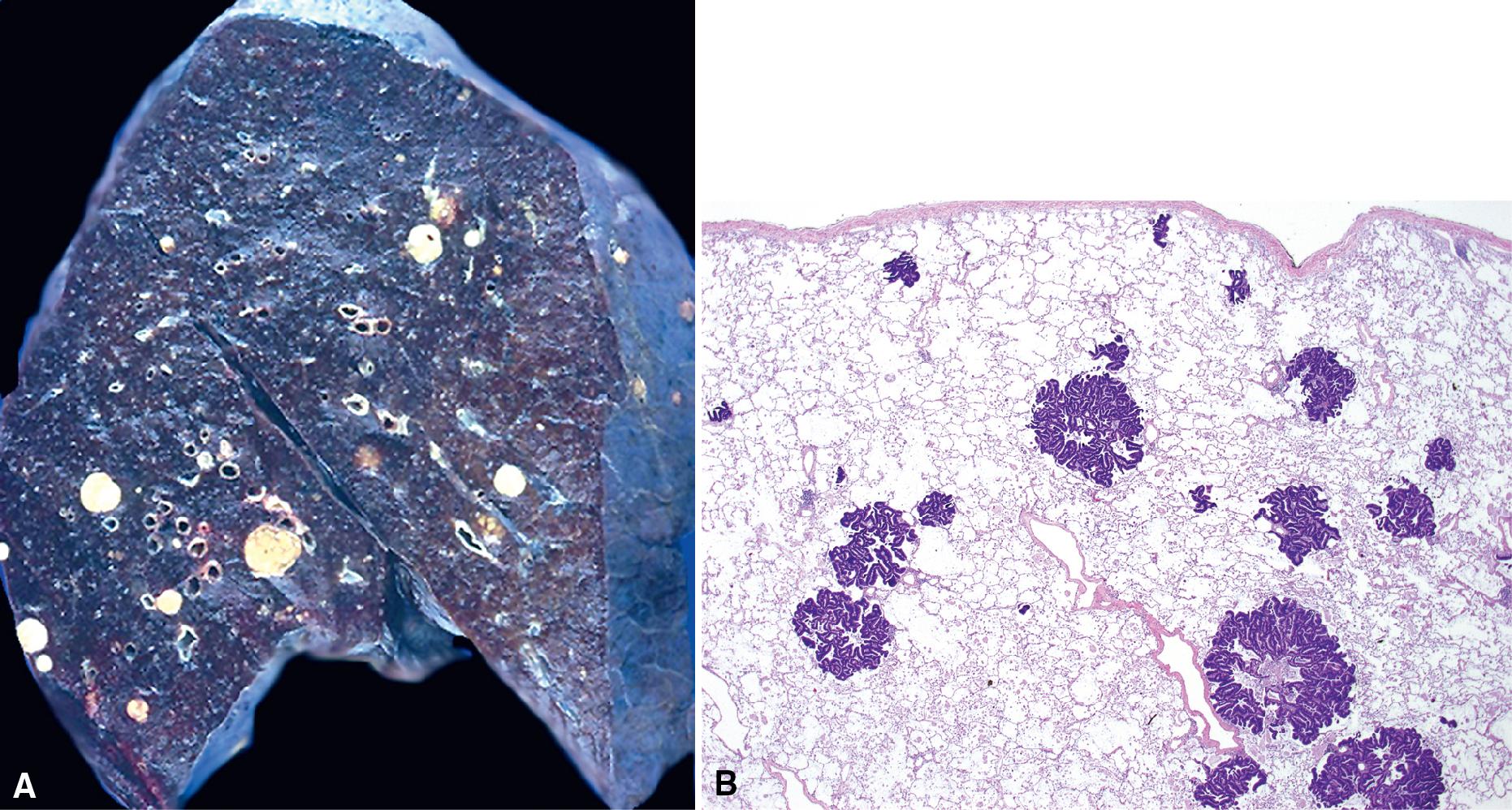
Carcinomas may gain access to the pulmonary lymphatic system by: (1) retrograde spread, (2) direct invasion of the pulmonary lymphatics, and (3) passage through adjacent blood vessels. This last process is the most common with tumor first spreading hematogenously to the lung followed by focal areas of interstitial growth. The neoplastic cells then may enter the lymphatics and permeate further throughout the lungs ( Fig. 18.7 ). Tumor in alveolar spaces may likewise be absorbed through the lymphatics adjacent to terminal bronchioles. Patients who have lymphangitic intrapulmonary metastases generally have had previous hematogenous spread. Direct lymphatic invasion is most often associated with tumors arising in the breast or stomach , , with metastases almost exclusively detected in the pulmonary lymphatic spaces, without the formation of mases. Other metastatic carcinomas capable of showing the same pattern of spread include malignancies from the ovary, thyroid, bladder, esophagus, liver, and appendix after the development of pseudomyxoma peritonei. , ,
Metastatic disease arising through direct seeding occurs when a malignant tumor gains access to a serosally lined cavity, such as the pleural space. Neoplasms that directly seed the pleura include primary lung cancers and malignancies of various lineages that originate in the chest wall or mediastinum. Primary lung tumors, such as a peripheral pulmonary carcinoma, may grow through the visceral pleura, which is less common in cases of chest wall sarcoma. The malignant carcinoma cells attach themselves to multiple pleural sites and invade the subjacent tissues. Multiple subpleural nodules may coalesce to form a large serosally-based lesion.
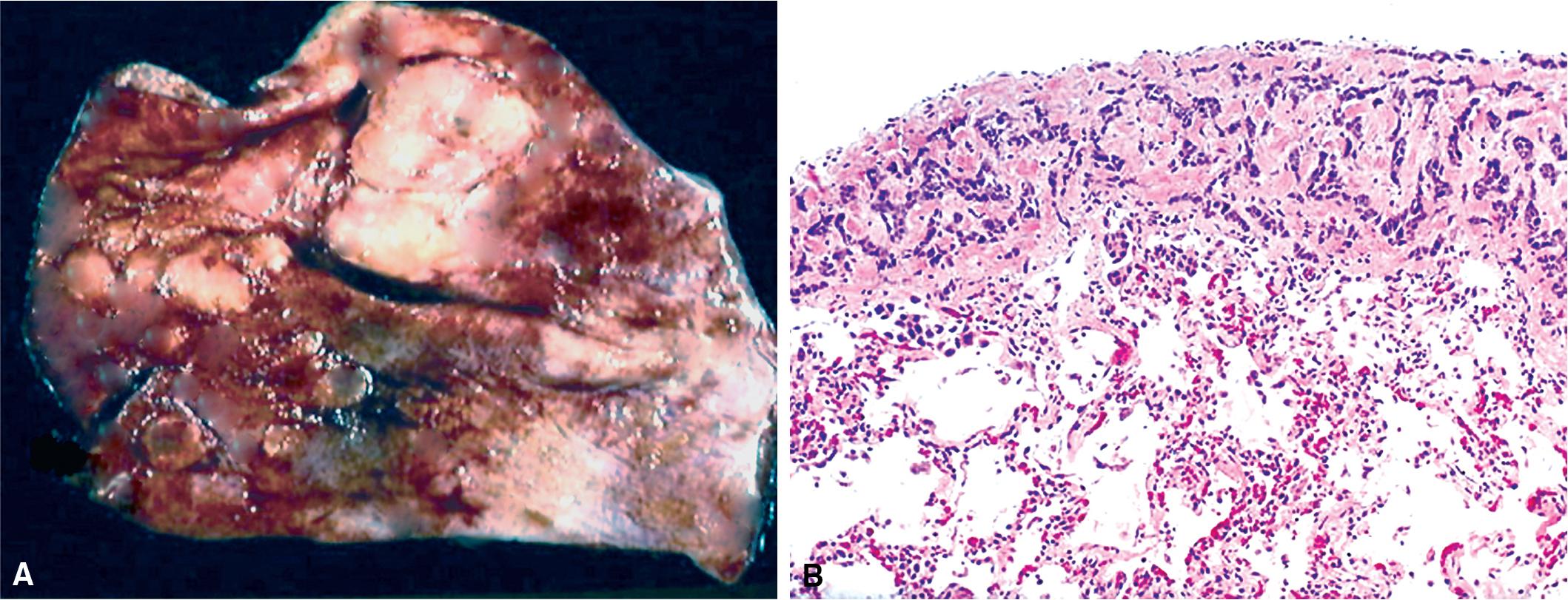
Metastases are the most common form of pleural malignancy. Most derive from primary neoplasms of the chest wall, mediastinum, or lungs, although extrathoracic primary malignancies are also well represented. The largest tumor nodules tend to be basally situated ( Fig. 18.8 ).
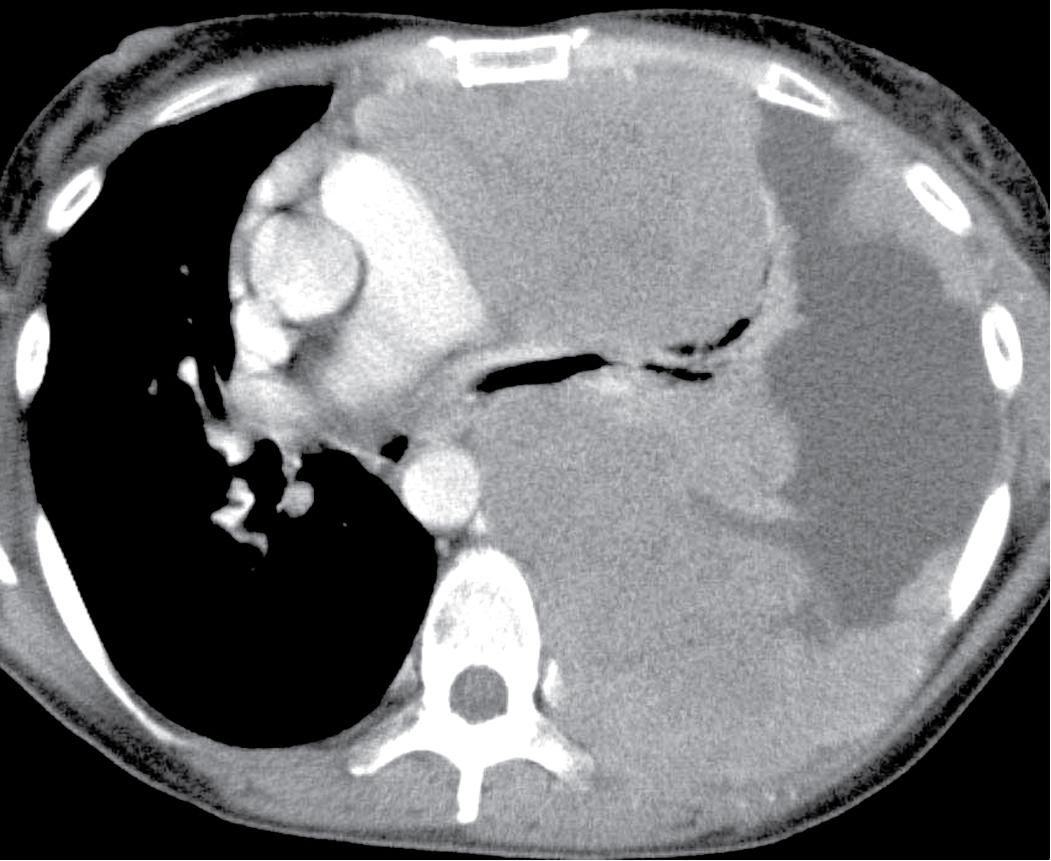
At least two-thirds of malignant pleural effusions may be diagnosed by cytologic sampling. More than 90% of cases are recognized on the first specimen, , with sensitivity predictably increasing with successive sampling. Three specimens are recommended if the clinical suspicion of pleural metastasis is high.
Malignancy is second only to congestive heart failure as a cause of a pleural effusions. Neoplastic effusions may be quite massive, ranging up to 2500 mL in volume and these effusions often are hemorrhagic. Malignant involvement of the pleura also may be associated with scant serous fluid production. Not all pleural effusions in patients with a history of malignancy contain tumor cells, and benign effusions in such cases may be secondary to lymphatic obstruction, altered lymphatic drainage as a result of chemotherapy or radiation therapy, heart failure, or other causes. Because most sarcomas do not spread via lymphatic channels, metastases in the lung and pleura are not usually accompanied by a malignant effusion. Up to 90% of malignant pleural effusions caused by metastatic lung or breast cancers are ipsilateral with regard to the site of the original tumor. Patients with malignant pleural effusions typically have a poor prognosis and most die within a few months after diagnosis. Selected subgroups of patients, such as those with lymphoma, breast cancer, or some pediatric malignancies, may fare somewhat better.
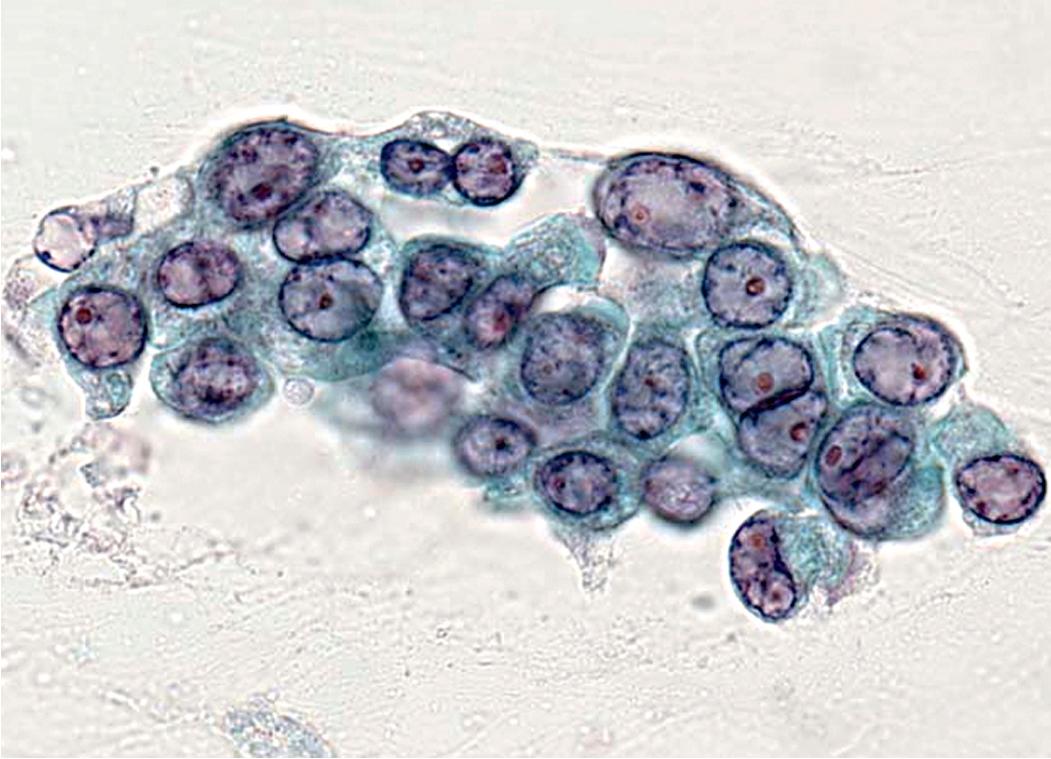
Chretien and Jaubert reported that 42% of cytologically sampled pleural effusions contained malignant cells. The likely site of tumor origin in such cases depended on patient demographics, although most series reported that primary pulmonary carcinomas were the most common. , Adenocarcinomas of the lung are the most common malignancy to involve the pleural fluid ( Fig. 18.9 ), followed by small cell carcinoma. , Squamous cell carcinomas of the lung rarely involve the pleural fluid. The most common extrathoracic malignancies involving the pleural fluid arise in the breast, gastrointestinal tract, ovary, and lymph tissue (e.g., non-Hodgkin lymphoma). , , Up to 7% of metastatic carcinomas in the pleura are classified as carcinoma of an unknown primary (CUP) site. In one analysis of malignant pleural effusions, women predominated by a ratio of 2:1, although no gender predilection was observed in other published series. Epithelioid mesotheliomas often are associated with a pleural effusion, which may be very difficult to diagnose cytologically because the cells are often very bland in appearance.
Endobronchial metastases are considered as a separate category because of their distinctive clinical symptoms including adult-onset asthma. The reported incidence of endobronchial and endotracheal pulmonary metastatic disease is 1% to 18%. , , The most common sites of tumor origin in patients from North America and Western Europe are the breast, bone, soft tissue, large intestine, kidney, and skin (melanoma). , More than one-third of endobronchial metastases are sarcomatous. , In populations with a high prevalence of acquired immune deficiency syndrome, the most common secondary malignancies of the bronchi are Kaposi sarcoma and malignant lymphoma. Nasopharyngeal and laryngeal carcinomas are frequent sources of endobronchial metastasis in Asia.
Endobronchial metastases usually are a result of hematogenous or lymphogenous spread. , , Aerogenous spread may occur with an upper-airway malignancy. Tumors that originate in the lung, hilar lymph nodes, or mediastinum may spread by direct extension into the bronchial system. Early in the course of growth, endobronchial lesions typically cause symptoms of cough with sputum production, dyspnea, wheezing, and hemoptysis. , Up to 25% of patients are asymptomatic. Radiographically, an endobronchial mass is typically visible only on CT or MRI, as chest x-ray commonly shows only post-obstructive consolidation or atelectasis ( Fig. 18.10 ). The mean interval between the diagnosis of the original tumor and the appearance of an endobronchial metastasis is 4 to 5 years. These patients have a poor survival, with a median of 11 months. Patients with breast cancer may have a better prognosis. , ,
In histologic and cytologic specimens, secondary endobronchial malignancies may be confused with primary malignancies, such as squamous cell carcinomas, neuroendocrine carcinomas, or salivary gland-type tumors. Endobronchial adenocarcinomas other than salivary morphotypes should raise the suspicion of metastatic disease. An exuberant reactive stromal proliferation around endobronchial lesions may mimic a metastatic spindle cell sarcoma.
Clinicians perform the same diagnostic tests in suspected primary or secondary pleuropulmonary malignancies. These include sputum cytology , ; bronchoscopy with brushing, washing and alveolar lavage; transbronchial or transtracheal aspiration and biopsy ; transthoracic fine-needle aspiration (FNA) , ; thoracoscopic biopsy such as video-assisted thoracic surgery ; open thoracotomy and biopsy; and effusion cytology. In some cases, expectant management is undertaken with sequential radiologic studies. A computerized tomography scan (CT) or positron emission tomography scan (PET) may be obtained to delineate further abnormalities and possibly aid in the distinction between primary and secondary malignancies (e.g., mediastinal adenopathy favors a primary lung malignancy).
The diagnostic accuracy of primary and secondary malignancies largely depends on the size and the location of the lesion rather than its specific histologic subtype. For example, the sensitivity of FNA is 93% in lesions larger than 2 cm in diameter and 60% for those smaller than 1 cm. Raab et al. assessed the accuracy of percutaneous FNA in a group of hospitalized patients with known extrapulmonary malignancies and new solitary lung masses. Pathologists correctly classified 87% of the pulmonary lesions as primary or secondary malignancies. More than 90% were metastases, indicating that the probability of a primary lung tumor was low in this clinical setting. Raab et al. found that the use of immunohistochemical studies was needed in only 20% of cases but yielded a definitive diagnosis in 78% of cases in which it was used.
Diagnostic accuracy is higher in peripheral nodules compared to central lesions. Pilotti et al. reported that the sensitivity of FNA in the detection of metastatic pleuropulmonary disease was 89%, whereas it was 92% for primary malignancies. Another interinstitutional study reported 96% specificity for transthoracic FNA. The sensitivity and specificity of bronchoscopy depends on the location of the lesion. , Thoracoscopy is a sensitive means of accessing peripheral lesions and has a high level of accuracy overall. It may be viewed as a treatment option as well as a diagnostic test in patients who have limited metastatic disease, especially if lung function is compromised.
Kern and Schweizer concluded that the sensitivity of sputum cytology for the detection of intrapulmonary metastasis was similar to that associated with primary lung cancers. Similarly, sputum cytology is more likely to be productive if the metastatic lesions are large and centrally located. The diagnostic accuracy of sputum cytology increases if sequential samples are obtained.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here