Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Barrett’s esophagus (BE) occurs in the setting of chronic gastroesophageal reflux disease (GERD). It is characterized by conversion of the normal esophageal squamous epithelium into metaplastic columnar epithelium . Since its original description by Tileston et al. there have been several alterations of this definition. It is now widely accepted that BE is an alteration of the esophageal mucosa that is visible endoscopically and has a corresponding histologic abnormality. The endoscopic aspects about recognizing BE are reviewed in greater detail in Chapter 5 : “Diagnosis of Barrett’s Esophagus.” The discussion here focuses on a brief review of the definition of BE, intestinal metaplasia at gastroesophageal junction (GEJ), and the gross and microscopic aspects of BE and BE-related dysplasia.
GEJ, as defined in North America, is the junction between the tubular esophagus and proximal stomach. The location of GEJ is approximated by the most proximal extent of the gastric folds . In Asia, this is determined by locating the distal extent of palisade of longitudinal veins . The squamocolumnar junction (SCJ), also known as the Z-line, is the junction of the squamous mucosa and columnar mucosa. It is normally somewhat irregular in appearance. The location of SCJ and GEJ may not coincide endoscopically. Furthermore, the precise anatomic localization remains difficult in many cases, particularly in the setting of a hiatal hernia . Thus, the precise location of the biopsy is crucial in determining the presence of BE.
Traditionally, the narrow segment of mucus-secreting columnar mucosa distal to the squamous esophageal mucosa, but proximal to acid-secreting gastric oxyntic mucosa has been termed the gastric cardia. In recent years, the existence of the gastric cardia as a native structure has been called into question by some authors who believe that cardiac-type mucosa is always metaplastic, likely in response to gastroesophageal reflux . While metaplastic cardiac-type mucosa undoubtedly is frequently identified in the distal esophagus, evidence from detailed studies of the anatomy and histology of the GEJ, including pediatric autopsy series, supports the notion that the gastric cardia is a native structure . Thus, there is sufficient evidence to support the presence of a small zone of native cardiac mucosa in the most proximal stomach, and in many individuals, metaplastic cardiac-type mucosa of variable length in the distal esophagus.
Although Tileston described the presence of reflux-induced esophageal ulcers in an autopsy series, it was not until nearly 50 years later that Dr Norman Barrett confirmed that this was indeed the lower esophagus that was lined by columnar epithelium . However, it was not until later in 1976 that Paull et al. reported that columnar metaplasia of esophagus (or columnar-lined esophagus (CLE)) in fact is a mosaic of three different types of epithelia: (a) fundic type (with oxyntic glands), (b) junctional type (with cardiac-type glands), and (3) specialized type (with goblet cells) . Multiple studies have documented that the risk of dysplasia and adenocarcinoma is significantly increased when the metaplastic epithelium harbors intestinal metaplasia. For this reason, in the United States, we currently diagnose BE based on the 2008 American College of Gastroenterology Practice Parameters Committee Guidelines and the recent Position Statement issued by the American Gastroenterological Association . Per these guidelines, BE is defined as “change in the distal esophageal epithelium of any length that can be recognized as columnar-type mucosa at endoscopy and is confirmed to have intestinal metaplasia by biopsy of the tubular esophagus” . Thus, the definition consists of a two-pronged approach—an endoscopically visible mucosal change/abnormality and a histologic correlate characterized by the identification of goblet cells. This definition, however, is not universally accepted. In fact, the British Society of Gastroenterology does not require the presence of intestinal metaplasia to diagnose BE . Similarly, the Japanese require the documentation of CLE with or without goblet cells . Additional details regarding evolving definition of Barrett’s esophagus can be found in Chapter 5 : “Diagnosis of Barrett’s Esophagus.” An international agreement on a definition of Barrett’s was achieved in 2015 by the BOB CAT (Benign Barrett’s and CAncer Taskforce) consensus group for the first time as “Barrett’s is defined by the presence of columnar mucosa in the esophagus and it should be stated whether intestinal metaplasia is present above the gastroesophageal junction” .
BE is characterized by irregular tongues of salmon-colored mucosa within the esophagus with or without areas of erosion and ulceration. BE-related dysplasia can be subtle and difficult to recognize endoscopically. It may appear as erosions, ulcers, and slightly elevated mucosa to areas of nodularity, stricture, or polypoid growth. The current guidelines recommend the use of advanced imaging techniques that should be superimposed on high-resolution white light endoscopy using high-definition systems . These techniques have the advantage of improving the detection rate of flat dysplastic lesions that are not readily visualized using standard endoscopic tools. Additional information regarding endoscopic techniques can be found in Chapter 6 : “Screening and Surveillance of Barrett’s Esophagus,” Chapter 7 : “In Vivo Optical Detection of Dysplasia in Barrett’s Esophagus With Endoscopic Light Scattering Spectroscopy,” Chapter 8 : “Enhanced Imaging of the Esophagus: Optical Coherence Tomography,” and Chapter 9 : “Enhanced Imaging of the Esophagus: Confocal Laser Endomicroscopy.”
The surface and the crypt epithelium of Barrett’s mucosa are composed of mucinous epithelium interspersed with goblet cells, enterocytes, and cells with features that are intermediate between intestinal and gastric foveolar cells. The surface epithelium usually shows neutrophilic inflammation, ulceration, or a villiform appearance in some cases. In addition to goblet cells, gastric foveolar-type cells (incomplete intestinal metaplasia), and intestinal absorptive-type cells (complete intestinal metaplasia), the metaplastic glands may also contain Paneth cells, neuroendocrine cells, and even pancreatic acinar cells. The lamina propria surrounding the glands contains variable numbers of inflammatory cells and fibroblasts.
Studies have shown that CLE is a heterogeneous mucosa that demonstrates considerable variability in the distribution of goblet cells, including a distinct gradient with the proximal segment containing a higher density of goblet cells compared to the distal segment . The distal segment of BE has a higher density of oxyntic-type glands compared to the proximal segment . Thus, the proportion of goblet cells is higher at the neo-squamocolumar junction and proximal esophagus. They may range from focal and few goblet cells per crypt to diffuse and numerous in other biopsy fragments. A retrospective study has shown that at least eight biopsy specimens are required to adequately assess intestinal metaplasia. In addition, the yield of intestinal metaplasia is lower in the presence of short-segment BE .
Barrett’s epithelium is typically composed of cells that resemble incomplete intestinal (type II or type III) metaplasia of stomach with chronic gastritis. Complete intestinal metaplasia (type I) is less common. Regardless, subtyping intestinal metaplasia has no clinical implication on the management of BE. Goblet cells are best identified by virtue of their shape and the chemical composition of intracytoplasmic mucin ( Fig. 3.1 ). Because they are rich in acidic mucins (predominantly sialomucins admixed with lesser quantities of sulfated mucins), they acquire a basophilic cytoplasmic blush that is readily recognized on a routine hematoxylin and eosin-stained tissue section . Histochemical stains for acidic mucins, such as Alcian blue at pH 2.5, show intense dark-blue/magenta staining for this combination of sialomucins and sulfated mucins, which contrasts with the predominantly periodic acid–Schiff (PAS)-positive neutral mucins found within the adjacent gastric foveolar-type cells ( Fig. 3.2 ). Routine Alcian blue staining is costly and time-consuming. Since goblet cells can be quite readily recognized on routine hematoxylin and eosin-stained slide, routine use of Alcian blue is not recommended for the diagnosis of BE.
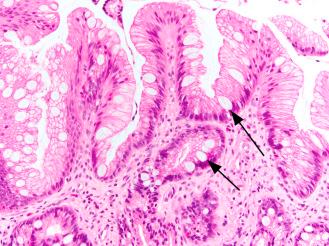
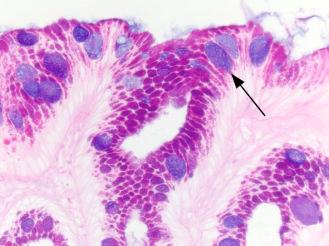
On occasion, markedly distended foveolar epithelial cells may mimic goblet cells (“pseudogoblet cells”) and cause diagnostic confusion. They are usually distributed in a continuous fashion compared to true goblet cells, which tend to be dispersed sporadically throughout the metaplastic epithelium ( Fig. 3.3 ). Additionally, they stain pale eosinophilic on hematoxylin-eosin stain and contain neutral mucin that does not react with Alcian blue at pH 2.5. Caution must be exercised when interpreting histochemical stains for detecting goblet cells. The columnar cells located between the goblet cells contain small quantities of acidic mucin and may show some Alcian blue positivity (so-called columnar blues). In the absence of goblet cell metaplasia, the identification of these cells does not fulfill the criteria for a definitive diagnosis of BE.

The finding of intestinal metaplasia in biopsies obtained from the esophagogastric junction (EGJ) raises two diagnostic possibilities: ultrashort-segment BE or chronic carditis with intestinal metaplasia (CIM). Unfortunately, clinical, endoscopic, or pathologic findings do not allow one to accurately distinguish between these two entities. There is clear evidence that CIM carries a lower risk of neoplastic progression than either short- or long-segment BE In a recent study, Srivastava et al. showed that in a mucosal biopsy from EGJ, the presence of the following features were significantly associated with a diagnosis of BE over CIM: (1) crypt disarray and atrophy, (2) incomplete and diffuse IM, (3) multilayered epithelium, (4) squamous epithelium overlying columnar crypts with IM, (5) hybrid glands, and (6) esophageal glands/ducts .
The expression of CDX2 , a caudal homeobox gene expressed during development, is specific evidence of intestinal differentiation . Several studies have shown that CDX2 is expressed in BE-related intestinal metaplasia . To date, no direct comparisons have been published with regard to potential expression differences between CIM and short-segment BE. Several other markers evaluated for this purpose include Das1, MUC1, MUC2, MUC5AC, MUC6, CK7/CK20 pattern, and CD10. These studies are hampered by differences in endoscopic biopsy protocols and study populations that contribute to apparent discrepancies in their results and lack of reproducibility. Thus, the clinical utility of evaluating intestinal metaplasia of the EGJ using these various biomarkers has not yet been established.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here