Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The medial patellofemoral ligament (MPFL) is the primary soft tissue restraint to lateral patellar translation. The MPFL is often injured with a first-time lateral patellar dislocation. Rehabilitation is the mainstay of treatment for first-time patellar dislocation; however recurrent patellar instability results in substantial morbidity in active individuals. MPFL reconstruction has become the cornerstone of surgical stabilization of the patella for recurrent lateral patellar dislocations. Although techniques for MPFL reconstruction vary, adherence to biomechanical and anatomic principles is necessary for optimal outcome. Compliance with postoperative rehabilitation protocol is important for optimal recovery and return to activity.
Laxity of the medial retinacular patella stabilizing structures due to recurrent lateral patella dislocations, documented by physical exam, stress radiographs, and/or arthrometer testing
Acute patellar dislocation with associated osteochondral fracture, loose body, or other intraarticular injury requiring surgical attention
Documented recurrent patellar instability events after completion of appropriate rehabilitation
Continued lack of knee confidence and fear of patellar dislocation despite adequate rehabilitation efforts
Patellofemoral pain without instability
Patellofemoral arthrosis without instability
Excessive radiographic lateral patellofemoral tilt &/or translation without patellar instability
Patellar instability should be differentiated from patellofemoral pain, with appropriate consultation including history, physical exam, and direct imaging. Pain between dislocation events could be from chondral damage or other soft tissue pain issues and may not be improved with patellar stabilization.
Comprehensive preoperative evaluation, including detailed documentation (imaging) of anatomic risk factors of patellar instability is essential to guide treatment options.
Quantify and document excessive lateral patellar translation under anesthesia at the start of the case. Compare this to the contra-lateral leg.
MPFL patellar attachment should be placed in the proximal half of the patellar cartilage’s longitudinal surface.
The MPFL graft should be tunneled through the soft tissue in an extra-synovial manner, within the second layer of the medial knee structures.
Anatomic femoral insertion is critical. A preferred method is using imaging landmarks (i.e., Schöttle’s point), under fluoroscopic guidance. Anatomic landmarks can serve as a proxy, if needed.
After locating the femoral MPFL placement (e.g., with a Kirschner wire), range the knee to test graft isometry. If the graft shortens through knee range of motion, the starting point may be too proximal. If the graft lengthens, the starting point may be too distal.
Secure the graft in knee flexion with the patella well-located in the groove (typically 30 to 45 degrees).
Avoid violating the posterior patellar articular surface when securing MPFL patellar fixation.
Patellar fixation techniques that utilize an oblique tunnel thru the anterior cortex risk a patellar fracture.
Multiple or large drill holes through the patella create stress risers and increase the risk of a patella fracture.
Malposition of the femoral tunnel can lead to abnormal graft forces and predispose the patient to elevated patellofemoral pressure, pain, and/or graft failure.
Loss of motion is the most common complication following patellar stabilization and can be the result of inadequate postoperative rehabilitation, tunnel malposition, or graft overtensioning at the time of graft fixation.
Primary dislocation of the patella is the cause of 2% to 3% of knee injuries and has an incidence rate of 5.8/100,000 in the general population. , This rate is as high as 29/100,000 in patients 10 to 17 years of age and affects athletes of both sexes. Sex has often been thought to be a predictor of patellar instability risk. , Generally, females are considered to be at higher risk than males, although this is not consistent across studies.
Anatomical abnormalities such as trochlear dysplasia, patella alta, extensor mechanism malalignment, femoral anteversion, tibial torsion, and valgus deformity of the knee may increase predisposition to patellofemoral instability. , First-time dislocations are typically managed conservatively, as the risk of recurrence after a first-time dislocation is 33.6% based on a recent systematic review. Many recent studies have shown that the risk of redislocation increases as the number of risk factors increases ( Table 100.1 ). Even in the absence of recurrence, pain and instability persist in many patients.
| RISK OF RECURRENCE (%) | |||
|---|---|---|---|
| 0 | 1 | 2 | 3 |
| 8.6 | 26.6 | 29.6–60.2 | 70.4 |
| 7.7 | 22.7 | 50.9 | 78.5 |
| 13.8 | 30.1 | 53.6 | 74.8 |
The MPFL is the primary soft tissue restraint to lateral patellar translation in early flexion, the position of the knee when lateral patellar dislocations typically occur. As the knee continues into flexion, the bony patellofemoral anatomy, in particular trochlear depth, provides the primary restraint to lateral patellar translation. Soft tissue procedures that address MPFL deficiency have garnered growing interest in recent years. A surgical approach to MPFL deficiency will be further discussed.
Knowledge of the medial side of the knee is imperative for successful MPFL surgical planning and execution. The MPFL can consistently be identified just distal to the vastus medialis obliquus, within the second of three layers. The MPFL runs transversely from the medial patellar and quadriceps tendon borders to the femur. The femoral origin is within a well-defined saddle between the medial epicondyle and the adductor tubercle. LaPrade et al. noted this location to be 1.9 mm anterior and 3.8 mm distal to the adductor tubercle. The MPFL attaches to the proximal third of the medial patella. The MPFL provides 50% to 60% of soft tissue restraint to the lateral translation of the patella.
In the first 20 to 30 degrees of knee flexion, the quadriceps fires and pulls the patella laterally. This is countered by the MPFL, which centers the patella in the trochlear groove. Nomura et al. found increased lateral subluxation of the patella between 20 and 90 degrees of flexion with progressive sectioning of the MPFL.
Early surgical dissections described femoral-sided injuries as the most common injury site. More recent studies utilizing magnetic resonance imaging (MRI) have found a more uniform distribution of MPFL injury patterns, including patella-based ruptures, femoral-based ruptures, intrasubstance ruptures, and multifocal injuries. Age and skeletal maturity likely affect MPFL injury location, as younger patients more often have patella-based ruptures. ,
Patellar instability is most commonly characterized by excessive lateral patellar translation and includes a spectrum of incidents ranging from dislocations in activities of daily living to traumatic dislocation events. The factors salient to the treatment algorithm include any history of recurrent dislocations, age at time of first dislocation, history of contralateral (bilateral) dislocation, and family history of patellar dislocations. ,
In the acute traumatic setting, the patella may spontaneously reduce or it may require a formal reduction maneuver. Pain and swelling are a result of soft tissue and potential articular surface damage. Hemarthrosis is common in acute injuries, with aspiration recommended for patient comfort as needed.
The physical exam can vary based on the timing of patellofemoral instability as the examination differs for acute and chronic instability patients. Acute dislocations will be discussed in less detail, as they are typically more readily apparent from the patient’s history. These patients present with more obvious physical exam findings, such as swelling, pain, apprehension, and laxity. The knee is observed for intraarticular and extraarticular swelling and deformity. Soft tissues are palpated to identify areas of tenderness, including along the MPFL. A comprehensive ligamentous examination is important to rule out concomitant cruciate or collateral ligament injuries. Medial collateral ligament injuries commonly occur at the time of patellar dislocation. Patients may be able to describe a spontaneous relocation event or may require a formal reduction in the emergency department.
With regard to the evaluation of a patient with recurrent instability, the patient should be evaluated while standing and while walking to assess for tibiofemoral alignment, particularly valgus alignment and rotational abnormalities. Single-leg squats or step-downs should be performed to assess hip strength and core control. An assessment of ligamentous laxity utilizing the Beighton criteria should be conducted.
The rest of the examination can take place with the patient supine or seated on an examination table. A general examination of knee range of motion, ligamentous stability, and meniscal pathology must be performed and compared with that of the contralateral leg. The examiner should evaluate for areas of referred pain, localized tenderness, or neurological compromise.
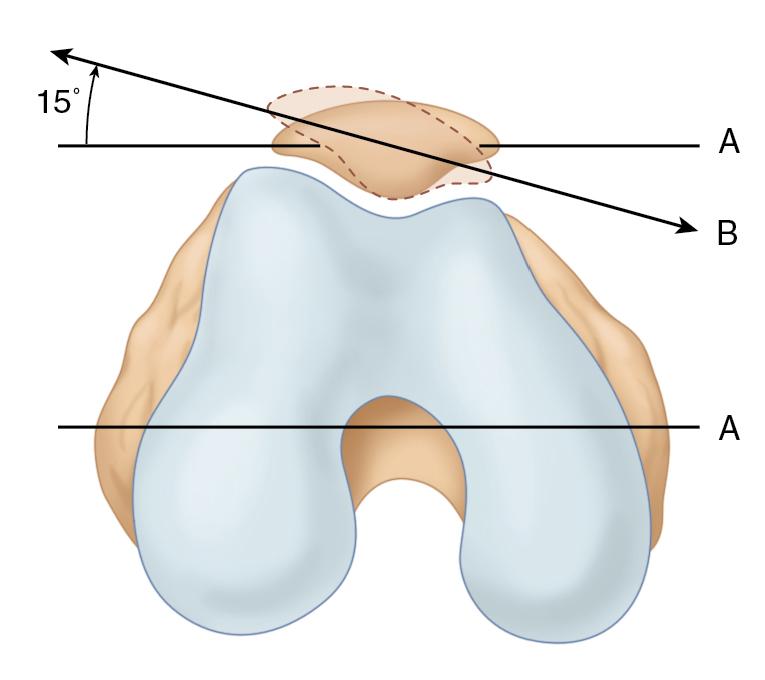
During active knee extension, patellar tracking is observed and the patella is evaluated for a tendency to slip laterally as the knee approaches the last 20 degrees of extension, when the patella is no longer constrained by the lateral trochlear ridge. The patella clearly moving laterally near terminal extension or medially in early flexion is termed a J sign.
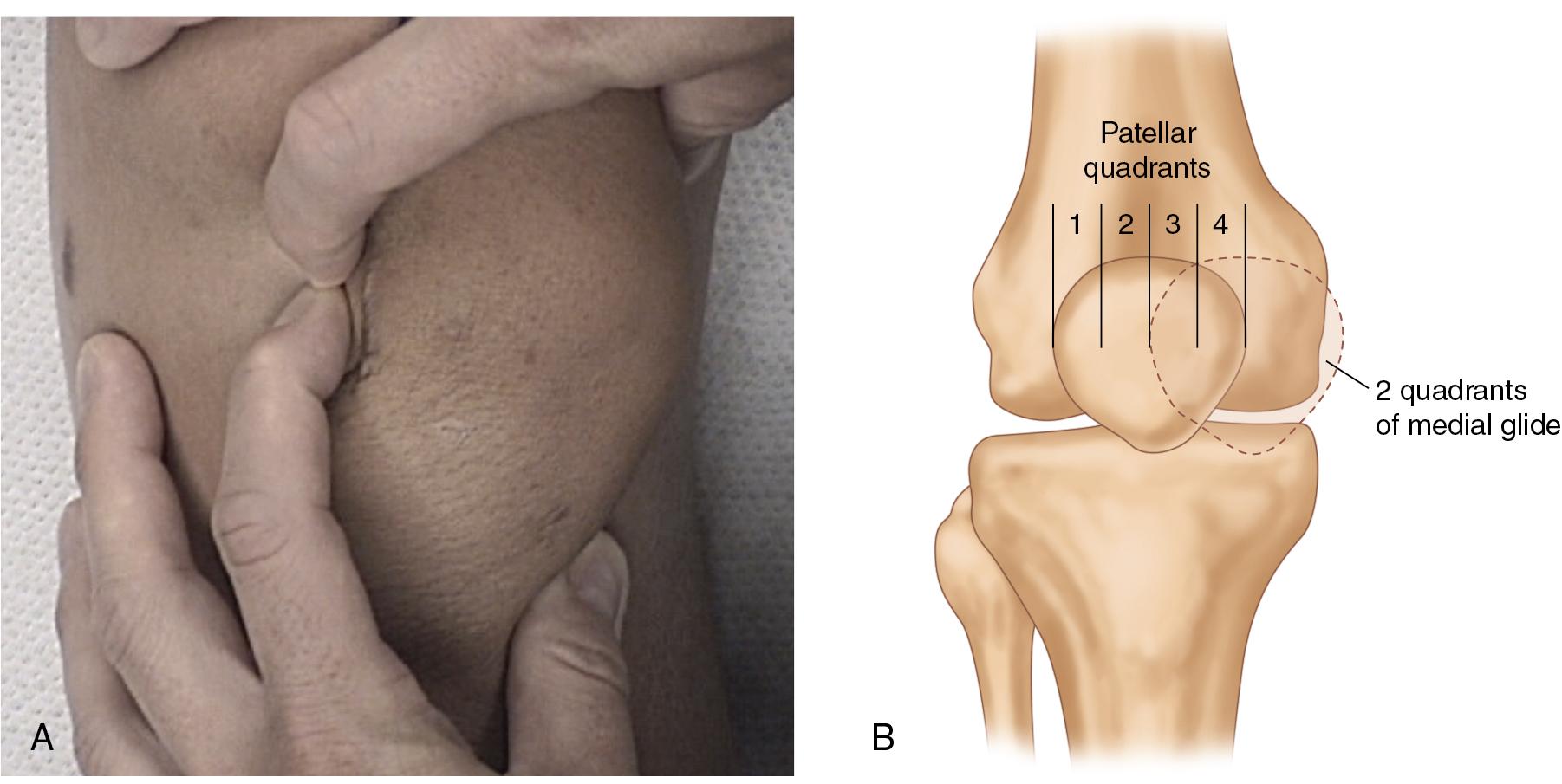
Patellar translation is measured by applying a laterally directed force to the medial side of the patella with the knee in extension. Patellar laxity can be evaluated by quantifying the amount of translation (in quadrants) as well as the consistency of the endpoint ( Fig. 100.1 ). Translation of less than two quadrants is considered normal, while two or more quadrants indicates laxity of the medial restraints. When this is unilateral and associated with an acute injury, it suggests an MPFL injury. More important than the absolute translation is the comparison to the uninjured knee and whether it has a firm or soft endpoint or the presence of an apprehension sign when submitted to the same test. Lateral retinacular tightness is assessed by attempting to lift the lateral edge of the patella, known as the tilt test ( Fig. 100.2 ). The retinaculum is considered tight if the patella will not correct to a neutral or horizontal position.
Routine radiographs, along with what each of these evaluate, are listed in Table 100.2 . Radiographic images of weight-bearing anteroposterior, lateral (30 degrees of flexion), tunnel, and Merchant or Laurin (20 to 30 degrees of flexion) views should be taken to evaluate lower extremity alignment and osseous morphology. The tunnel view is useful for showing osteochondral lesions or loose bodies present in the notch. The lateral view gives information about patellar height and trochlear morphologic features. The Merchant or Laurin view helps determine the degree of patellar subluxation and tilt, the presence of osteochondral lesions, or the extent of arthritis in the patellofemoral joint. Long leg standing radiographs help to assess for valgus alignment.
| Radiographic View | Evaluation |
|---|---|
| Axial views: Low flexion view (20–30 degrees) |
Sulcus angle, patella position in the groove (excessive lateral tilt and/ or translation), patellofemoral joint space narrowing (in older group) |
| True lateral view | Trochlear dysplasia, patella height, patellofemoral joint space narrowing (in older population) |
| Standing AP | Joint space narrowing, limb alignment |
| Standing PA flexion | Joint space narrowing, especially lateral compartment |
Computed tomography (CT) scans and MRI scans are growing in popularity because of improved visualization of patellar tracking, osseous abnormalities, chondral lesions, and MPFL lesions, as compared with standard radiographs. Although CT scans are ideal for showing the bony anatomy, MRI scans show the soft tissue injuries, including MPFL tears, meniscus tears, and chondral lesions. In acute injuries, underlying anatomic patellar instability risk factors, as defined by MRI, did not predict injury patterns as defined by the location and severity of MPFL injury, chondral damage, and/or bone bruising.
Slice axial imaging can also be used to assess for axial plane limb alignment. Historically, CT scans were the imaging modality of choice, but MRI and gait studies are gaining popularity.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here