Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Medial ligament injuries are among the most frequently treated problems of the knee joint, with the majority not requiring operative intervention. Whereas isolated superficial medial collateral ligament (SMCL) ruptures are common, concomitant damage to the anterior cruciate ligament (ACL) also occurs in many cases, especially in young and active patients.
Overall, there are four types of SMCL injury patterns: (1) SMCL tears that also almost always involves the meniscofemoral and meniscotibial attachments (deep medial collateral ligament [DMCL]); (2) associated posteromedial capsular (PMC) tears (posterior oblique ligament [POL]); (3) associated ACL or posterior cruciate ligament (PCL) tears with patterns 1 or 2; and (4) multiple ligament injuries or knee dislocations.
The mechanism of injury to the medial ligaments involves a valgus stress with usually a combined external tibial rotation component from either a noncontact (pivoting or cutting) or a contact injury (direct blow to the lateral side of the thigh or knee). The decision process regarding the appropriate treatment of medial ligament injuries involves determining the severity of the injury to the entire knee, including the other knee ligaments, and the specific injury pattern of the medial structures and menisci.
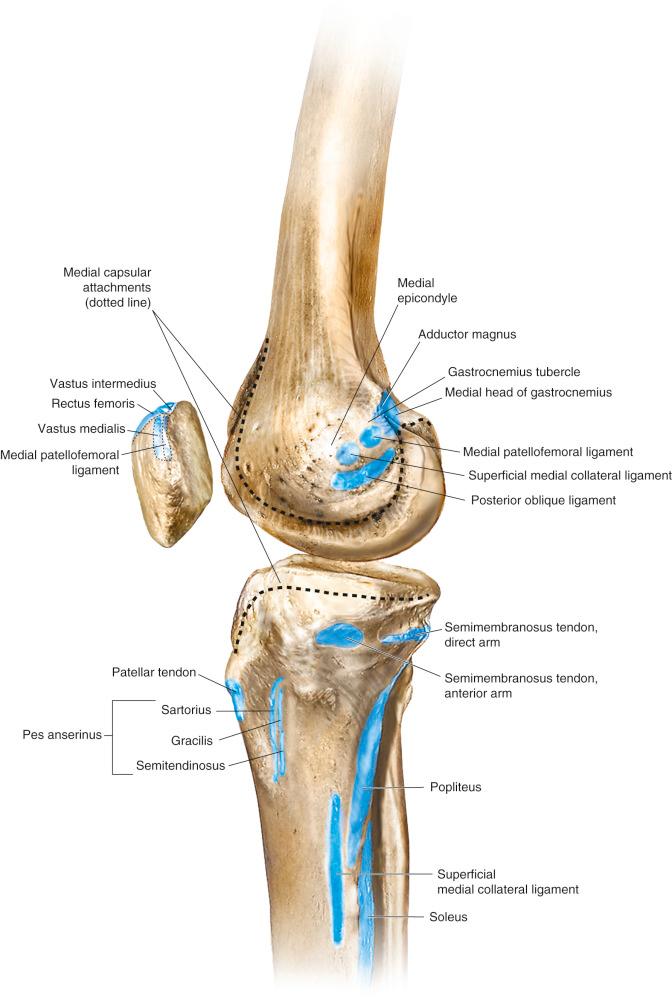
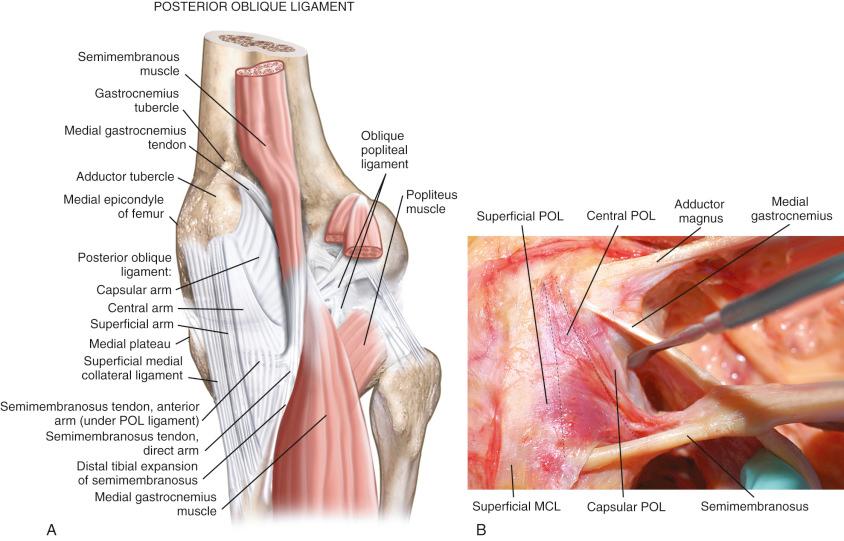
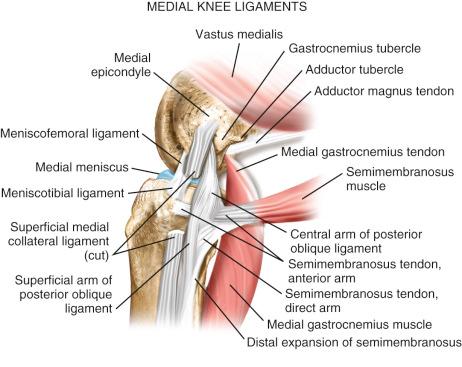
The medial structures identified for purposes of surgical treatment consist of the SMCL, DMCL (including meniscus attachments), and the PMC, which includes the structures referred to as the POL and semimembranosus attachments. The key to the diagnosis and treatment of medial ligament injuries relies on a comprehensive understanding of the intricate anatomy on the medial side of the knee. This is presented in detail in Chapter 1 . In Figure 19-1 , the osseous attachments of the medial structures are shown. Figure 19-2 shows the medial and posteromedial ligament structures, which are discussed in detail. Figure 19-3 shows the relationship of the semimembranosus muscle attachments to the posteromedial structures and POL. These include the bifurcation of the semimembranosus tendon into a direct and anterior arm just distal to the joint line and a minor attachment of the direct arm to the medial coronary ligament along the posterior horn of the medial meniscus. The semimembranosus tendon sheath makes up a distal tibial expansion that includes a medial and lateral division. A major attachment of the semimembranosus forms the oblique popliteal ligament, which is a broad fascial band that courses laterally attaching to the fabella, posterolateral capsule, and plantaris (see Chapter 1 , Fig. 1-6 ).
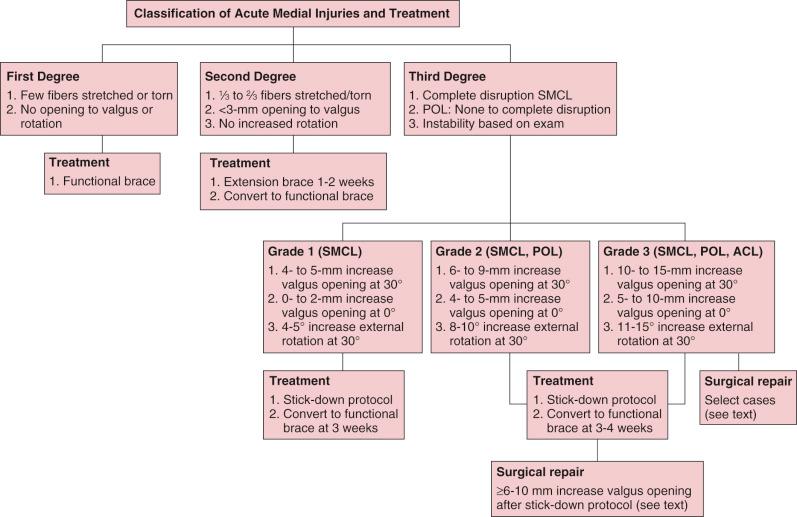
It is important to understand and classify the soft tissue injury of all the medial structures. The majority of acute medial ligament injuries that involve damage to the SMCL alone, or SMCL and PMC, are treated conservatively. The nonoperative treatment algorithm is shown in Figure 19-4 and discussed later in more detail. Gross major disruption of all of the medial structures alone or in addition to the ACL or PCL tears involve a group of select knees. The treatment of these gross ligament disruptions is discussed in a later section of this chapter.
In cases of chronic injury to the medial ligaments, it is important to obtain a complete history and objective and functional rating. We use the Cincinnati Knee Rating System (CKRS) for this analysis (see Chapter 41 ) to determine patient complaints of giving-way and the levels of activity at which this symptom occurs as an indication for surgical stabilization procedures. In this chapter, instability refers to an increase in abnormal motion limits as detected on the physical examination and is not used to indicate giving-way events.
Patients who have medial ligament tears classified as first, second-, or third degree that demonstrate either no increase or a mild to moderate increase in medial joint opening at 0 and 30 degrees of flexion do not require acute medial ligament repair or reconstruction.
A valgus malalignment and valgus thrust on walking contraindicates a medial ligament reconstruction in chronic cases without first performing an osteotomy to correct the lower limb malalignment. Alternatively, a genu varus provides a theoretical benefit of decreased tensile loads on the medial ligament structures.
In chronic cases of disruption of the medial ligaments, particularly associated with ACL or PCL tears, joint arthritis and associated pain and swelling may exist that contraindicate a soft tissue reconstruction. The patient goals and anticipated symptoms from the preexisting arthrosis are carefully considered.
Sedentary, nonathletic patients who do not experience pain, swelling, or giving-way with daily activities do not require surgery. These patients are advised to maintain their ideal body weight and obtain yearly consultations to monitor the knee joint.
In chronic cases, patients with marked lower extremity muscle atrophy are not candidates for surgery until adequate muscle strength is regained. The high potential for postoperative complications exceeds the potential benefits in these patients, especially in regard to developmental patella infera, quadriceps shutdown, and arthrofibrosis. A formal program of physical therapy should be pursued, which may be required for many months to improve overall lower limb muscle strength and function, particularly in multiligament injuries.
Associated medical problems may exist that either require treatment or contraindicate surgery, including complex regional pain syndrome, diabetics, vascular insufficiency, skin lesions, infectious conditions, obesity, or other medical diseases.
A considerable amount of discrepancy exists in the literature regarding the use of terminology to describe and classify the medial ligament injuries from an anatomic standpoint and the abnormal motion limits that exist (see Chapter 3 ). We agree with Hughston and coworkers that the clinician must clearly separate and classify medial ligament tears as either first degree (tear involving a few fibers), second degree (partial tear, no instability, 3 mm or less of medial joint opening), or third-degree (complete rupture, see Table 19-1 and Fig. 19-4 ). This is one of the earliest systems devised and is based on a classification proposed by the American Medical Association. The problem has arisen, as amply demonstrated in Table 19-1 , that this classification system has been modified extensively by different authors and it is often not possible to categorize the injury severity of the knees under treatment. A grade 1 instability (0 to 5-mm increased joint opening) may represent a second-degree injury (0 to 3-mm increased joint opening) or a third-degree injury (5-mm increased joint opening), requiring protection to allow healing as discussed. This also applies to a grade 2 instability where a 6- to 9-mm increased joint opening is treated conservatively with immobilization, whereas other studies include these as operative cases. Thus it is necessary in the review of the literature to perform a subset analysis, which has been done in this chapter, to try to obtain the category or type of injury under treatment and our treatment recommendations.
| Reference | System |
|---|---|
| Hughston et al (1976, 1983) |
|
| Fetto & Marshall (1978) |
|
| Garrick (2004) |
|
| Bergfeld (1979) |
|
| Shelbourne & Patel (1995) |
|
| Petersen & Laprell (1999) |
|
| Fanelli & Harris (2007) |
|
For purposes of this chapter, the injury classification in acute cases of medial ligament injuries is based on the clinical examination shown in Figure 19-4 . Note that the medial ligament injuries are based on the first-, second-, and third-degree original classification system. The approximate increases in medial joint opening and external tibial rotation are shown for the different categories of injury. Some classification schemes use a system in which each grade represents a further 5-mm increase in joint opening (grades 1, 2, and 3) over the contralateral normal knee, whereas Hughston and colleagues use a grade to classify the degree of injury and then represent the absolute amount of joint opening in the injured knee (1+, 2+, and 3+ in 5-mm increments; see Table 19-1 ). This chapter uses the increase in millimeters of medial joint opening between the injured and contralateral normal knee because this is the system used in published biomechanical and kinematic studies to be discussed.
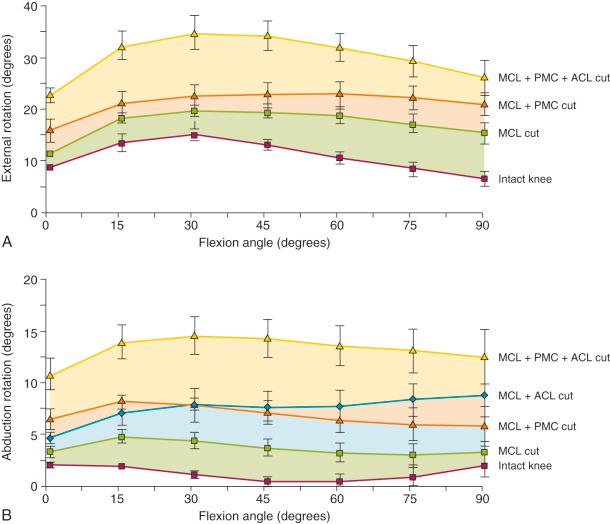
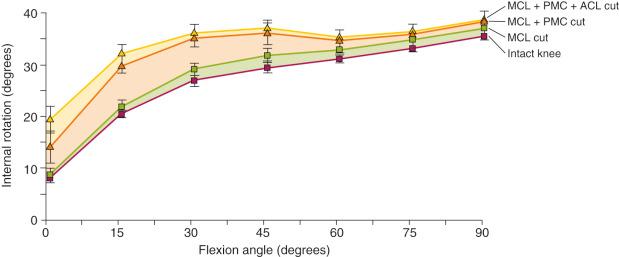
A review of the in vitro cadaveric biomechanical function of the medial ligaments and ACL in resisting medial joint opening, external tibial rotation, and internal tibial rotation is provided in Figure 19-5 , summarized in Table 19-2 , and discussed in more detail in Chapter 3 . A finding of increased medial joint space at 30 degrees of flexion (third-degree sprain, parallel fibers of the SMCL), but not at 0 degrees of flexion indicates the PMC (including the POL) is still functional. Any further increase in medial joint opening at 0 degrees indicates concurrent damage to the PMC. With complete disruption of the SMCL and PMC, the ACL and PCL become a restraint to further medial joint opening. The increase in abduction for a combined MCL/POL injury and MCL/ACL injury at 15 to 45 degrees of flexion is nearly the same (see Fig. 19-5, B ). The major difference between these injuries is in increased abduction at full extension in the MCL/POL-ruptured knee. In summary, knees with rupture to both the medial collateral ligament (MCL) and POL will demonstrate approximate increases in external tibial rotation (average of 9 degrees at 30 degrees of flexion), internal tibial rotation (average of 9 degrees at 30 degrees of flexion), and abduction testing at 0 and 30 degrees of flexion (averages of 5 degrees and 7 degrees, respectively).
| Motion Limit | 0 Degrees of Flexion | 15 Degrees of Flexion | 30 Degrees of Flexion | 60 Degrees of Flexion | 90 Degrees of Flexion |
|---|---|---|---|---|---|
| Anterior (mm) | |||||
| ACL | 5.8 ± 0.9 * | 9.4 ± 1.0 † | 8.4 ± 1.9 * | 4.7 ± 2.1 ‡ | 3.5 ± 1.6 ‡ |
| ACL & MCL | 6.1 ± 2.0 * | 10.0 ± 2.4 * | 11.0 ± 2.9 * | 10.6 ± 3.5 * | 10.1 ± 4.2 ‡ |
| MCL & POL/PMC | –0.5 ± 1.1 | –0.3 ± 1.1 | –0.5 ± 0.9 | –0.1 ± 0.7 | 0.4 ± 1.1 |
| ACL & MCL & POL/PMC | 8.7 ± 3.2 † | 12.8 ± 4.3 † | 14.4 ± 4.9 † | 14.6 ± 5.7 † | 12.5 ± 5.6 * |
| External Rotation (Degrees) | |||||
| ACL | 1.2 ± 1.4 | 0.7 ± 0.8 | 0.7 ± 0.6 | 0.7 ± 0.4 | 0.5 ± 0.5 |
| MCL | 2.5 ± 1.1 ‡ | 3.3 ± 1.5 ‡ | 4.6 ± 1.3 * | 8.0 ± 2.2 * | 8.7 ± 3.2 ‡ |
| POL/PMC | 1.6 ± 0.9 | 1.2 ± 1.2 | 0.9 ± 1.7 | 0.8 ± 2.5 | 0.8 ± 2.4 |
| ACL & MCL | 2.3 ± 0.4 † | 3.2 ± 1.1 * | 4.6 ± 1.6 * | 7.3 ± 2.3 * | 7.5 ± 2.0 * |
| MCL & POL/PMC | 6.8 ± 2.5 ‡ | 7.2 ± 1.9 * | 9.0 ± 2.0 * | 13.6 ± 3.0 * | 15.0 ± 3.6 * |
| ACL & MCL & POL/PMC | 10.9 ± 5.8 * | 12.7 ± 6.2 * | 14.7 ± 6.5 * | 16.7 ± 5.9 † | 15.3 ± 5.1 † |
| Internal Rotation (Degrees) | |||||
| ACL | 2.9 ± 1.0 * | 2.2 ± 0.9 ‡ | 0.8 ± 0.9 | 0.5 ± 0.8 | 2.0 ± 2.6 |
| MCL | 0.5 ± 0.5 | 1.4 ± 0.7 | 2.1 ± 1.2 | 1.8 ± 0.3 † | 1.5 ± 0.4 * |
| POL/PMC | 3.4 ± 2.4 | 4.0 ± 2.3 | 2.7 ± 1.7 | 1.3 ± 0.7 | 1.4 ± 1.4 |
| ACL & MCL | 3.6 ± 1.5 ‡ | 3.5 ± 1.4 ‡ | 2.3 ± 1.3 | 2.4 ± 0.8 * | 2.1 ± 1.4 |
| MCL & POL/PMC | 6.3 ± 5.8 | 11.6 ± 3.4 * | 9.3 ± 2.2 * | 3.9 ± 2.4 | 2.9 ± 1.5 |
| ACL & MCL & POL/PMC | 12.7 ± 6.5 * | 13.2 ± 3.3 § | 10.4 ± 2.1 § | 4.5 ± 1.1 § | 3.3 ± 1.2 † |
| Abduction (Degrees) | |||||
| ACL | 0.4 ± 0.2 ‡ | 0.8 ± 0.5 | 0.6 ± 0.6 | 0.1 ± 0.3 | 0.0 ± 0.3 |
| MCL | 1.5 ± 0.9 | 3.3 ± 0.8 * | 4.1 ± 0.8 † | 4.5 ± 0.8 † | 3.8 ± 1.0 * |
| POL/PMC | 0.4 ± 0.3 | 0.2 ± 0.6 | 0.4 ± 0.3 | 0.0 ± 0.9 | 0.4 ± 0.5 |
| ACL & MCL | 2.5 ± 1.1 ‡ | 5.4 ± 2.6 ‡ ; | 7.1 ± 3.6 ‡ | 8.1 ± 4.0 ‡ | 7.1 ± 2.8 ‡ |
| MCL & POL/PMC | 4.6 ± 1.9 ‡ | 6.0 ± 1.4 * | 6.6 ± 0.9 § | 5.8 ± 1.2 † | 4.8 ± 1.1 * |
| ACL & MCL & POL/PMC | 9.1 ± 4.6 * | 12.7 ± 4.8 † | 14.4 ± 5.0 † | 14.2 ± 4.5 † | 12.1 ± 4.0 † |
The increase in medial joint opening and external tibial rotation shown in Figure 19-5 provides an indication of an associated ACL tear when these motion limits are distinctly abnormal. In these knees, there is a large increase in anterior tibial translation and the pivot shift test is in the grade III category.
The results show the importance of performing the dial tibial rotation test (see Chapter 17 ) to determine the anterior subluxation of the medial tibial plateau with medial ligament injuries. With a combined MCL/POL injury, there will be a noticeable increase in internal and external tibial rotation (see Fig. 19-5 and Fig. 19-6 ).
The medial structures resisting external rotation in the dial test show the SMCL is the primary restraint; however, the increase in external rotation is small (4.6-8.7 degrees at 30 and 90 degrees of flexion) and may not be clinically detectable. The increase in external tibial rotation approximately doubles when the SMCL and PMC are injured (9-15 degrees at 30 and 90 degrees of flexion), resulting in a qualitative detectable positive dial test. An even greater increase occurs with ACL rupture. It should be noted that Griffith and associates reported even larger increases in the dial test with SMCL sectioning, suggesting that some knees may have a positive dial test with this injury.
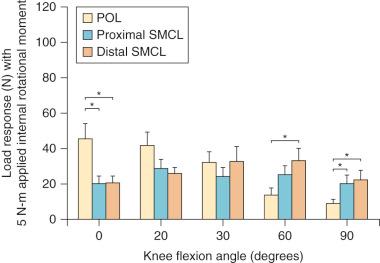
The medial structures resisting internal tibial rotation involve two primary restraints: the PMC/POL and SMCL, with the SMCL having a higher resistance in force measurements at 90 degrees and the PMC/POL having a higher resistance at 0 degrees of flexion ( Fig. 19-7 ). In the dial test for internal rotation, there are discrepancies in ligament sectioning studies regarding the magnitude of internal tibial rotation that occurs. In addition, there are no studies on the amount of anterior or posterior tibiofemoral compartment translation that occurs with medial ligament injuries. In general, sectioning the SMCL or PMC/POL individually produces only small increases in internal rotation whereas sectioning both structures results in an approximate 10 degrees increase in internal rotation at 30 degrees of flexion, with a lesser increase at 90 degrees of flexion. One study showed a similar amount of increased internal tibial rotation at both 30 and 90 degrees of flexion.
Sims and Jacobson reviewed 93 knees that underwent operative treatment for acute MCL injuries. These authors reported that 93% had associated injury to the POL following the description of Hughston and Eilers. The authors emphasized the importance of identification and repair of the POL and tears of the semimembranosus capsular attachment (present in 70% of knees) and associated peripheral detachment of the medial meniscus (present in 30% of knees, Fig. 19-8 ). The authors postulated that a dynamic function of the semimembranosus attachments exists for knee stability, but this is unproven experimentally. Although some authors describe rupture and surgical repair of the POL alone (anteromedial rotatory instability), the biomechanic data show that the POL is not a primary restraint for medial joint opening or external tibial rotation.
![FIG 19-8, Three major acute injury patterns (injury to the posterior oblique ligament [POL] are common to all): (1) injury to the POL with semimembranosus disruption, (2) injury to the POL with complete peripheral meniscocapsular detachment, and (3) POL injury with semimembranosus injury and peripheral meniscocapsular detachment. Disruption at any level is capable of disabling the dynamic function of the semimembranosus. 68 FIG 19-8, Three major acute injury patterns (injury to the posterior oblique ligament [POL] are common to all): (1) injury to the POL with semimembranosus disruption, (2) injury to the POL with complete peripheral meniscocapsular detachment, and (3) POL injury with semimembranosus injury and peripheral meniscocapsular detachment. Disruption at any level is capable of disabling the dynamic function of the semimembranosus. 68](https://storage.googleapis.com/dl.dentistrykey.com/clinical/MedialandPosteromedialLigamentInjuriesDiagnosisOperativeTechniquesandClinicalOutcomes/7_3s20B9780323329033000196.jpg)
A detailed history is taken that includes any previous knee injury and the mechanism of the current injury. The CKRS is used to evaluate the subjective, objective, and functional categories. In acute knee injuries, there may be a swollen knee, with a tense joint effusion and skin ecchymosis that is difficult to examine. Still, it is possible to rule out a multiligament injury with gross instability and complete a neurovascular examination, which includes assessment of signs of a deep venous thrombosis (DVT). The limb is immobilized and the acute injury appropriately treated (ice, compression, elevation, gentle range of motion [ROM], and early muscle activation) and the examination repeated after other diagnostic tests (radiographs, magnetic resonance imaging [MRI]) in 3 to 5 days.
The comprehensive examination of the knee joint required to detect all abnormalities includes (among other items) assessment of (1) range of knee flexion and extension, (2) knee joint effusion and swelling, (3) the knee motion limits and subluxations compared with the contralateral knee, (4) alignment of the patellofemoral joint, (5) patellofemoral and tibiofemoral crepitus, (6) tenderness along the medial joint line and along the entire course of the SMCL from proximal to distal, (7) overall lower limb alignment, (8) neurovascular status, and (9) gait.
The palpation of the medial joint is particularly important to determine if the SMCL tear is more proximal at the femoral attachment, diffuse, or more distal at the tibial attachment. These findings are correlated with MRI. In a young athlete with open physes, palpation at the femoral physis is usually painful and careful radiographic stress views are always obtained to rule out a physeal fracture. A MRI is always helpful to confirm the diagnosis.
The clinical tests for the assessment of ligament injuries are shown in Figure 19-9 . SMCL disruption is determined by manual valgus stress testing at 0 and 30 degrees of knee flexion. The surgeon estimates the amount of joint opening (in millimeters) between the initial closed contact position and open position of each tibiofemoral compartment (avoiding internal or external tibial rotation). The result is recorded according to the approximate increase in the tibiofemoral compartment of the injured knee compared with that of the opposite normal knee. This estimated increase in medial joint opening is easily confirmed at a later time by the gap test if arthroscopy is indicated, as in cases of associated ACL injury.

The integrity of the ACL is determined by Lachman and pivot shift testing. The result of the pivot shift test is recorded on a qualitative scale of 0 to III, with a grade of 0 indicating no pivot shift; grade I, a slip or glide; grade II, a jerk or clunk with the subluxation-reduction; and grade III, gross subluxation with impingement of the posterior aspect of the lateral side of the tibial plateau against the femoral condyle. A KT-2000 (MEDmetric) arthrometer test may be done at 20 degrees of flexion (134-N force) to quantify total anteroposterior (AP) displacement. The medial posterior tibiofemoral step-off on the posterior drawer test is done at 90 degrees of flexion.
The tibiofemoral rotation dial test is done at 30 and 90 degrees of knee flexion with the patient in the supine position to determine whether increases in external tibial rotation occur with anterior subluxation of the medial tibial plateau (and not posterior subluxation of the lateral tibial plateau, indicating a posterolateral ligament injury). An increase in internal rotation may occur with MCL/POL disruptions (maximum 15 to 45 degrees of flexion). Associated lateral and posterolateral disruptions are determined by varus stress testing at 0 and 30 degrees of knee flexion.
A careful observation of the patient's standing alignment and gait is performed to determine whether there is a lower limb valgus alignment and valgus thrust during ambulation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here