Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Structural and functional development of gut motility in human infants is a process in continuum and varies with birth gestation, postnatal age, nutritional methods, acute illnesses and/or their treatments, comorbidities, and genetic factors. The entire process is complex and is dependent on maturation of the central and enteric nervous systems and gut musculature.
Gastrointestinal motility reflexes develop in utero , and several are functional at full-term birth while some have limited functions after preterm birth. Postnatal maturation advances the frequency, magnitude, sensitivity thresholds, coordination, cross-system interactions, and adaptation of these reflexes.
The developmental aspects of pharyngo-esophageal, gastrointestinal, and colonic motility in human neonates are highlighted. Postnatal maturation of gastrointestinal motility reflexes is dependent on sensory and motor regulation of the intrinsic enteric nervous system integrated and modulated by the central nervous system and autonomic nervous system.
In infants with oral and/or enteric feeding difficulties, mechanisms of motility dysfunction can be due to maldevelopment (absence of reflexes), immaturity (lack of progression with postmenstrual age), malfunction (poor transit and clearance reflexes), or maladaptation (abnormal consequences related to contiguous and cross-system reflexes).
The neonatal period is a time of rapid growth and development that is critical for the evolution of gastrointestinal motility reflexes. Development is grossly dependent on the infant’s maturation both in utero and ex utero . By 14 weeks gestation the cellular components necessary for coordinated neural and muscular activities exist in the fetal gut. However, maturation of neuromuscular functions occurs during mid- and late gestation. This translates to fully functional coordinated gut motility patterns in the full-term healthy neonate capable of independent feeding, aerodigestive protection, and small and large intestinal peristalsis. After birth, this process continues to evolve ex utero and is influenced by the postnatal maturational changes in the central nervous system and enteric nervous system (CNS and ENS), gut muscles, and interstitial cells of Cajal (ICC), as well as by the diet and rapidly changing anatomy and physiology during infancy. In vulnerable high-risk preterm infants, the influences of immaturity, along with other comorbid conditions including neurologic injury, chronic lung disease, hypoxia, inflammation, and sepsis, among others, can complicate and alter the postnatal development of gastrointestinal motility. Coordinated movements of the gut are crucial for the primary function of the neonatal foregut (to facilitate a safe feeding process to steer the feedings away from the airway), midgut (gastrointestinal transit of luminal contents to modulate absorption and propulsion), and hindgut (evacuation of excreta to maintain intestinal milieu homeostasis). In this chapter we will review and summarize the developmental aspects of gut motility (pharyngo-esophageal, gastrointestinal, and colonic) to further explain its potential clinical implications and controversies in neonates.
By the third week of conception, the human gut initially arises as a primitive tube from the endoderm of the trilaminar embryo and later receives contributions from all the germ cell layers. The endoderm gives rise to the epithelial lining and glands, the ectoderm gives rise to the oral cavity and the anus, and the mesoderm-derived splanchnic mesenchyme gives rise to the smooth muscle and connective tissue. During week 4, the differentiation of the foregut, midgut, and hindgut occurs. The foregut later develops into the airway and lung buds, pharynx, esophagus, stomach, and proximal portion of the duodenum; the midgut gives rise to the remainder of the duodenum, small intestine, and portions of the large intestine up to the distal transverse colon; and the hindgut develops into the distal part of the transverse colon, descending colon, rectum, and proximal part of the anal canal.
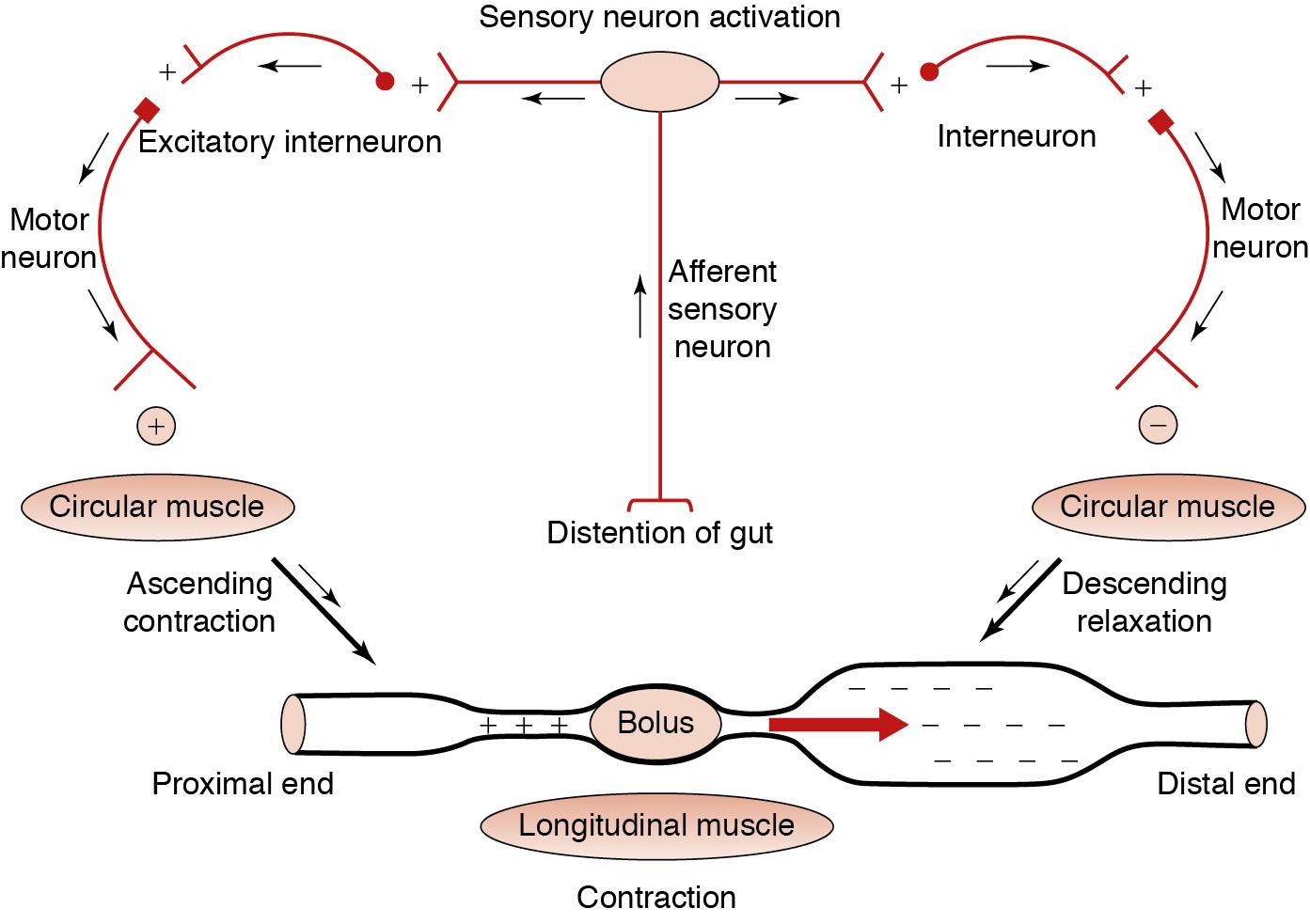
Smooth muscle is innervated by the intrinsic neurons of the ENS, which consists of interconnected ganglia containing neurons and glial cells. The ENS arises from precursor cells derived from the vagal (hindbrain) neural crest that enter the foregut and advances in a rostral-caudal direction. The cells colonize the gut through a complex process of migration, proliferation, and differentiation along defined pathways, and they reach the midgut by week 5 of development and the entire length of the gut by week 7. , A second, more caudal region of the neural crest, that is, the sacral neural crest, also contributes a smaller number of cells that are restricted to the hindgut ENS. The ganglia of the ENS are organized in two plexus layers that span the length of the gut—an outer myenteric plexus situated between the longitudinal and circular muscle layers, and an inner submucosal plexus lying between the circular muscle and the muscularis mucosae. , Neurons within the myenteric plexus are primarily involved in the control of gut motility, whereas neurons within the submucosal plexus are mainly involved in controlling mucosal functions, such as electrolyte and hormone secretion. , The ENS neurons may be classified according to their function as afferent sensory neurons, interneurons, and motor neurons. , , Activation of afferent neurons is the first step in the triggering of motor reflexes as they translate stimuli from the intestinal lumen into nerve impulses that are transmitted to interneurons and motor neurons. Interneurons form circuitry chains running both orally and aborally within the myenteric plexus. The orally running interneurons activate excitatory motor neurons, resulting in smooth muscle contraction, and the aborally running interneurons activate inhibitory motor neurons, resulting in smooth muscle relaxation. The excitatory motor neurons release acetylcholine and the inhibitory motor neurons release nitric oxide or vasoactive intestinal polypeptide. This sequential enteric reflex pattern of ascending contraction and descending relaxation, called peristalsis , forms the basis for Starling’s Law of the Intestine ( Fig. 1.1 ), which facilitates bolus propulsion in the peristaltic direction. The initiation and regulation of peristalsis is a complex process that involves pacemaker cells (ICCs) in addition to the smooth muscle cells and enteric nerves. ICCs generate spontaneous electrical slow waves, which constitute the basic electrical rhythm in the gut. ICCs develop independent of neural crest–derived enteric neurons or glia and originate mainly from Kit-positive mesenchymal mesodermal precursors.
The ENS is remarkably independent, but its neuronal activity can be modified or modulated by the CNS via the autonomic nervous system (ANS; parasympathetic and sympathetic nervous systems). , Much of the parasympathetic innervation to the gut travels via the Vagus nerve and the sacral nerves and is primarily excitatory to gut function by promoting secretion and peristalsis. In contrast, sympathetic innervation travels along the mesenteric blood vessels from the prevertebral ganglia and is primarily inhibitory to gut function by decreasing peristalsis and reducing perfusion of the gut.
The human fetal gut, by week 14, has the longitudinal, circular, and muscularis mucosal layers of smooth muscle, submucosal and myenteric plexuses, and ICC networks that are associated with the ENS. However, the first coordinated gut motility patterns do not occur until birth or about that time. By 11 weeks swallowing ability develops, by 18 to 20 weeks sucking movements appear, and by full-term gestation the fetus can swallow and circulate nearly 500 mL of amniotic fluid. ENS-mediated contractile activity is prominent in function by full-term birth and is essential for propulsive activity. Variations in gut motility and peristaltic patterns occur in prematurely born neonates and are discussed in the latter part of this chapter.
In neonates, deglutition refers to bolus propulsion from the mouth into the stomach, and it involves complex coordination of rhythmic sequences including sucking, swallowing, and breathing for safe bolus transit. Effective swallowing rhythms require pharyngeal contractions along with well-timed relaxations of the upper and lower esophageal sphincters (UES and LES, respectively) and sequential esophageal contractions. Using micromanometry methods, pharyngeal, UES, esophageal body, and LES functions have been characterized in neonates. During basal state, UES and LES maintain a resting tone irrespective of age or activity states, thus providing protective physical barriers against refluxate. With growth and maturation, the muscle mass and therefore the tone and activity of the UES increase. The average resting UES pressure (mean ± standard deviation) in preterm born neonates at 33 weeks postmenstrual age (PMA) was 17 ± 7 mm Hg and in full-term born neonates was 26 ± 14 mm Hg, whereas in adults it was 53 ± 23 mm Hg. Similarly, changes in LES length and tone have been observed with growth. , , Additionally, esophageal lengthening occurs in a linear fashion during postnatal growth in both premature and full-term infants.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here