Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Breast ptosis is one of the most common issues seen for evaluation in a plastic surgeon’s office. It can be developmental or more commonly acquired, secondary to weight loss, hormonal changes, pregnancy, and aging. A mastopexy is reserved for a patient for whom the major concern is breast ptosis and not an issue of volume, because the procedure repositions the breast with only limited removal of breast tissue.
There are many types of mastopexy techniques described to address the ptotic breast. The techniques are often described in reference to the final scar placement, such as the circumareolar technique, circumvertical technique, , and inverted-T scar technique. , However, there is much more variation in the techniques, including the vascular pedicle orientation, management of the parenchyma, and additional ancillary procedures to enhance the results.
The inverted-T scar technique has been the most widely used technique for both mastopexy and breast reductions because of its versatility, ease in execution, and predictable results. Excessive unwanted skin often plaguing a ptotic breast is addressed and excised as part of the procedure. The disadvantage is of course the presence of an additional scar along the inframammary fold (IMF) and failure to maintain lower pole stability over time.
In this chapter, we will describe our preferred technique for an inferior pedicle inverted-T mastopexy with or without mesh-reinforcement and the superior pedicle circumvertical mastopexy with inverted-T scar with or without auto-augmentation. Special emphasis will be placed on preoperative decision making and technical details of the operative approach.
The ideal candidate for a mastopexy alone is a patient who is relatively satisfied with her volume and is mainly looking for correction in her breast ptosis and improvement in breast shape. The ideal candidate has adequate breast volume and enough ptosis to warrant a mastopexy and the scars associated with these procedures. In the authors’ opinion, the inverted-T mastopexy is an excellent alternative for anyone who meets the criteria for a mastopexy based on its versatility, allowing for different pedicle designs, parenchymal manipulations, and use of ancillary techniques, such as mesh placement ( Fig. 15.1 )

There are a few patients in whom a mastopexy alone is not an ideal procedure. A patient desiring considerably more volume or significant upper pole volume and cleavage would be better served with an augmentation mastopexy technique ( Fig. 15.2 ). The exception would be the patient desiring those attributes, but the simultaneous procedure is deemed inappropriate or unsafe. In these cases, a mastopexy can be performed at the initial procedure, followed at least 6 months later with a breast augmentation (two stages). Additionally, a patient with mammary hyperplasia desiring significant volume reduction would be better served with a reduction mammoplasty.

The preoperative evaluation is used to determine the mastopexy technique that will achieve an optimal outcome that meets the patient’s desired results ( Box 15.1 ).
Relationship of the NAC to the IMF (Regnault’s degree of ptosis)
Amount of breast tissue overhanging the fold
Location of the NAC on the breast mound
Amount of vertical excess and horizontal excess
Ptosis was described by Regnault based on the relationship of the nipple–areola complex (NAC) to the IMF ( Table 15.1 ).
| Breast Ptosis | ||
|---|---|---|
| True ptosis |
|
|
|
|
|
|
|
|
| Glandular ptosis |
|
|
| Pseudoptosis |
|
|
The inverted-T technique is reserved for patients with significant ptosis and vertical excess that will benefit from skin excision along the fold. For patients with less ptosis and minimal vertical excess, a circumareolar or circumvertical mastopexy can be performed without the need for skin removal along the fold. In our experience, if the distance from the new nipple position to the fold is less than 10 cm, most likely only a vertical or a vertical with small horizontal wedge or J-extension will be adequate for correction, most commonly using a superior pedicle. To avoid the inframammary scar with a circumvertical mastopexy, the tissue at the base of the breast is resected internally causing elevation of the fold with the excess vertical length tucked under the new breast fold, eliminating the need for the horizontal scar. This has been less satisfying in our hands, and we always prefer to excise vertical excess skin through an inverted-T excision to achieve long-term success. Not removing the skin at the fold increases the risk of fold malposition, scar irregularities or dog ears, or elongation of the lower pole with bottoming-out over time.
When an inverted-T scar technique is selected, the decision on whether to use a superior pedicle or inferior pedicle must be determined. That decision is based mostly on the amount of ptosis, the quality of the breast tissue, and the position of the NAC. For patients with good-quality breast tissue and if the amount of NAC elevation is less than 5–6 centimeters, a superior pedicle is used with a circumvertical mastopexy inverted-T scar ( Fig. 15.3 ). An auto-augmentation may be performed with this approach if appropriate.

In breasts with poor-quality tissue with associated laxity and ptosis, if the NAC elevation is greater than 6 cm, an inferior pedicle inverted-T mastopexy is our preferred technique ( Fig. 15.4 ). Often, a mesh reinforcement is secured across the inferior pedicle to limit the lower pole stretch from the extra volume of the pedicle being retained in the lower pole. Whereas the superior pedicle technique may not be suitable for all patients undergoing mastopexy based on the limitations in pedicle length, the inferior pedicle has much greater versatility and can be used for most ptotic breasts based on a variety of factors, including surgeon preference.

The breast is a structure composed of breast lobules enveloped in a superficial fascial system. Many aspects of the breast composition contribute to the shape and stability of the breast. Assessment should include evaluation of the skin thickness and elasticity, the quantity and distribution of subcutaneous fat, the composition and firmness of the breast parenchyma, the integrity of the Cooper’s ligaments, the nature and position of the underlying musculature, and the shape and slope of the underlying chest wall. All of these aspects influence the shape of the breast and ultimately the outcome after the mastopexy. Thin skin with a lax skin envelope, fatty composition and elongated Cooper’s ligaments would predictably be qualities associated with poor outcomes in maintaining upper pole volume and shape postoperatively ( Fig. 15.5 ).
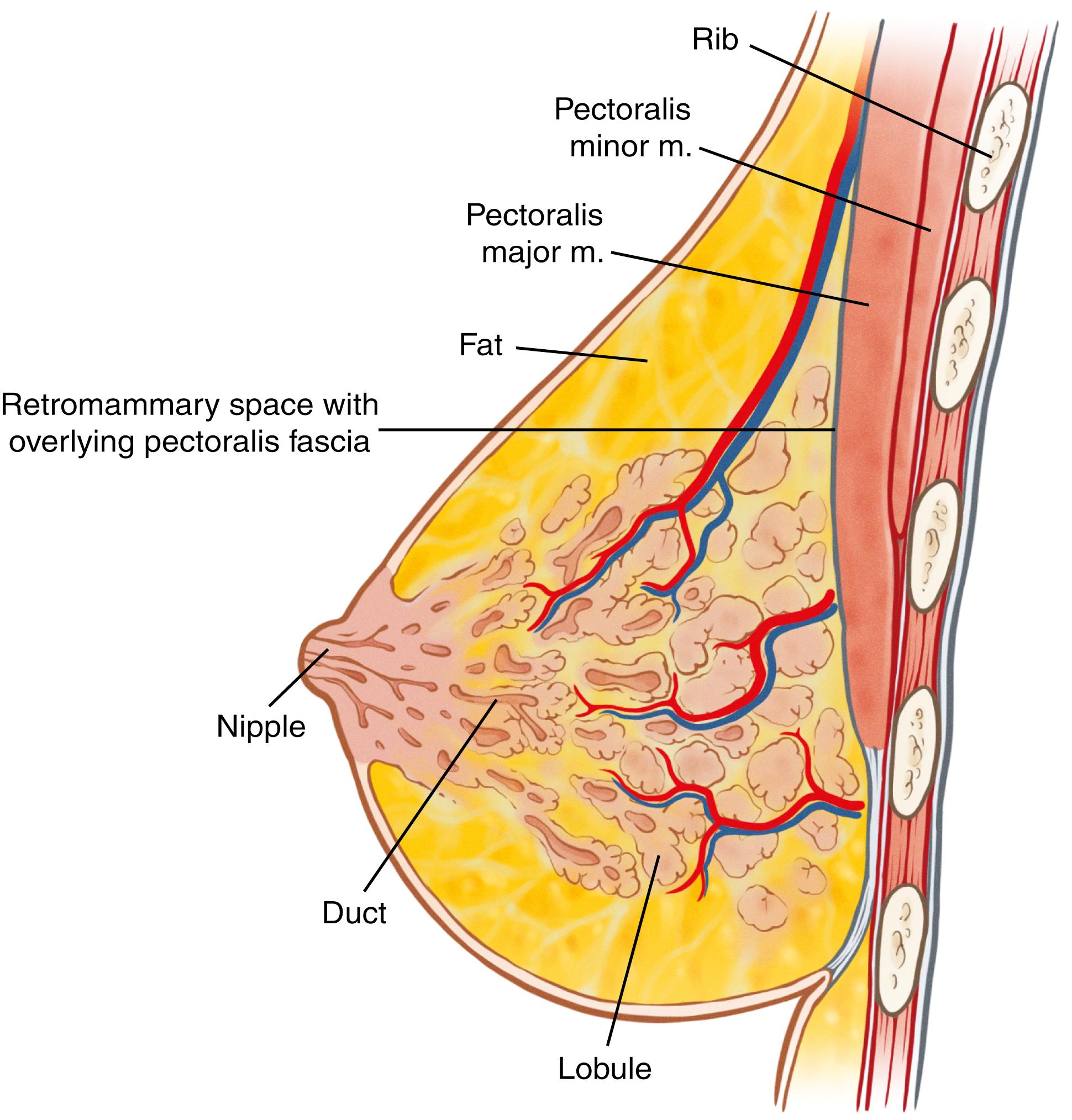
Although this provides some information about the degree of breast ptosis, it is insufficient to describe the true extent of breast ptosis. A more complete assessment of ptosis is summarized in ( Table 15.1 ). When performing a mastopexy, an understanding and assessment of the vascular anatomy is critical to performing the procedure safely. The breast has a rich blood supply from multiple sources, including the internal mammary artery (IMA) perforators, the lateral thoracic arteries, the thoracoacromial, anterolateral, and anteromedial intercostal perforators. The superior pedicle is supplied by the second branch of the IMA that emerges deep from the second interspace and courses superficially across the medial upper breast to enter the NAC slightly medial to the midline and approximately 1 cm deep. The medial pedicle is supplied by the third branch of the IMA that emerges from the third interspace and similarly courses superficially across the breast parenchyma to the medial aspect of the NAC. The inferior pedicle and central pedicle are supplied by the fourth branch of the IMA that courses deeply across the medial breast to enter through the Wuringer’s septum approximately 1–2 cm above the IMF and just medial to the breast meridian. The inferior pedicle also has additional blood supply through contribution from intercostal perforators along the IMF ( Fig. 15.6 ).

The markings guide the surgeon in providing symmetric NAC placement and mastopexy design. The patient is sitting upright during the markings. A line is initially drawn along the midline of the breasts and bilaterally down the meridians. The meridian lines bisect the breast equally and may not intersect though the nipple if there is NAC malposition. The IMFs are then drawn, noting any asymmetries to be addressed at surgery.
The position of the IMF is then drawn on the anterior breast through the meridian incision. The breasts are rotated medially and laterally to mark the location of the vertical incisions. Placement of the areola is then marked, starting approximately 2 cm above the nipple position and extending the curved drawing down to meet the medial and lateral vertical markings ( Fig. 15.7 ). This areolar opening marking should produce an areolar opening of approximately 42 mm. Approximately 7 cm below the bottom of the keyhole opening, a line is drawn marking the inferior extent of the vertical incision. Curved transverse lines are then drawn from these medial and lateral points extending down to the IMF.

When performing a superior pedicle technique, approximately 2–3 cm above the fold a U-shaped line connects the medial and lateral vertical markings to define the extent of skin resection ( Fig. 15.8 ). With inferior pedicles, the entire lower segment between the two medial and lateral vertical lines is de-epithelialized, making this line unnecessary ( Fig. 15.9 ).


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here