Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() For videos accompanying this chapter see ExpertConsult.com . See inside cover for access details.
For videos accompanying this chapter see ExpertConsult.com . See inside cover for access details.
The best way to approach esthetic breast surgery is to work with gravity – not against it. Remove tissue where it is in excess and add tissue where it is deficient. Although this sounds simplistic, it forms the basis of the principles of esthetic breast surgery. Although in some cases the skin brassiere can be used to shape the breast, it is better to rely on parenchymal reshaping for a consistent, long-lasting result. The parenchyma can be reshaped most easily by following this “excess/deficiency” principle.
The surgeon needs to understand what various surgical maneuvers can achieve and what our limitations are as surgeons. With that knowledge, we can then manage surgical results (and therefore patient expectations) more appropriately.
Because the upper breast border will not change with either a breast reduction or mastopexy, the result can be predictable (but not always what either the surgeon or the patient desires). Some patients are high-breasted and some are low-breasted. The breast is lifted – not at the upper breast border – but by controlling the glandular ptosis. Once the patient (and the surgeon) understands this concept, it becomes clear what can be “removed” in a breast reduction or “moved” in a mastopexy.
Patients and surgeons often think that the breast can be pushed up the chest wall, but the upper breast border will only be elevated if something is added (an implant raises the upper breast border on average 2 cm and fat grafting far less).
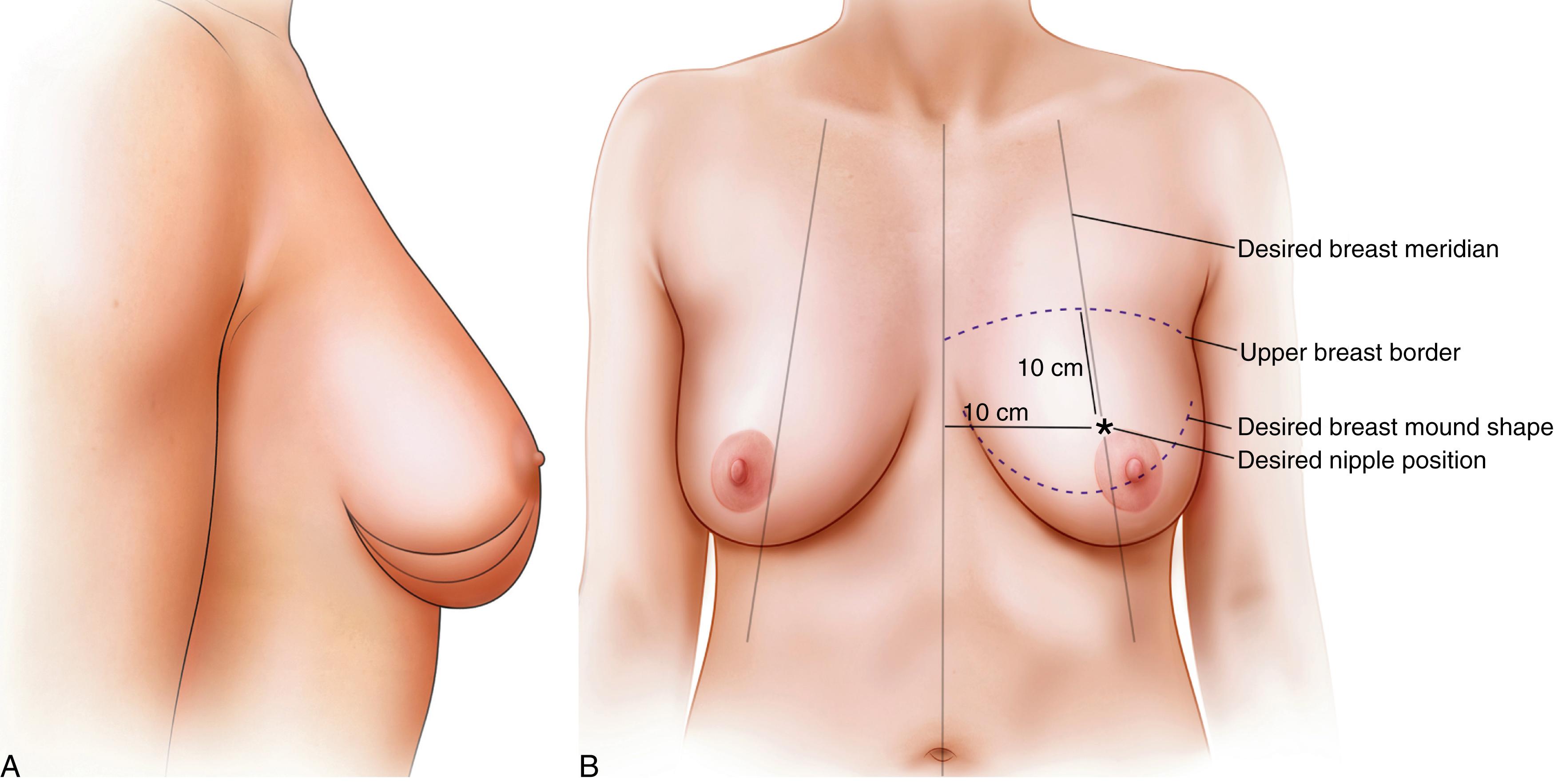
The surgeon can transpose drawings onto the patient’s photographs ( Fig. 38.1 ) and the decision-making process becomes simplified. Remove (or move) any ptotic gland below the ideal breast shape. Determining the ideal nipple position then becomes simple once the shape is outlined.
This involves an understanding of the inferior wedge principle. , The inferior ptotic gland needs to be “removed” in a breast reduction. It is best “moved” in a mastopexy using Liacyr Ribeiro’s method , where it can be separated and moved up to the center of the breast (not the upper pole). Filling the upper pole usually requires either an implant or the addition of tissue (e.g., fat grafting). The inferior wedge is that tissue below the Wise pattern.
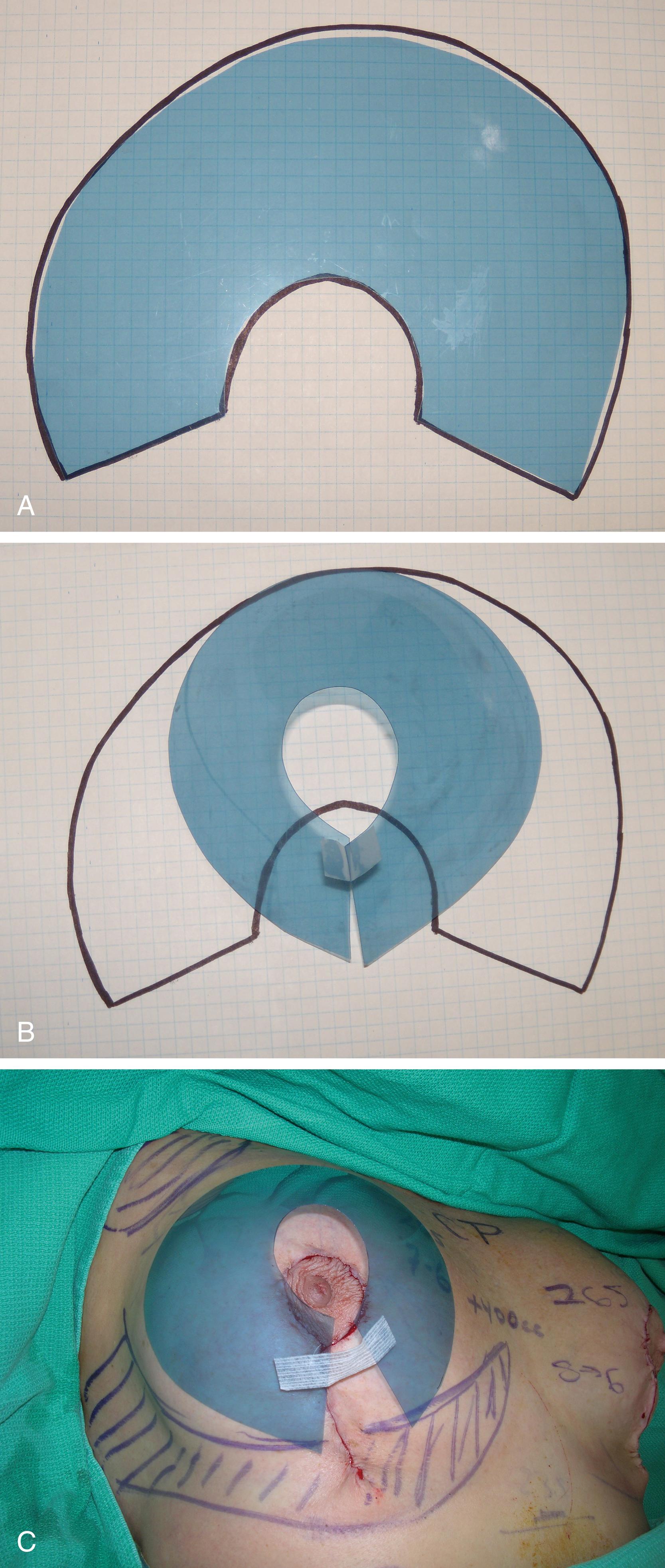
When Robert Wise deconstructed a brassiere and developed the “Wise pattern,” it was designed to be used for the skin to shape and hold up the breast ( Fig. 38.2 ). Unfortunately, skin is often not a good brassiere and it stretches with tension (as it does with skin expansion procedures). If the surgeon, on the other hand, uses the Wise pattern for the parenchyma – and leaves behind a Wise pattern (with no tension on either the parenchyma or the skin), the result will be predictable and long-lasting. The Wise pattern shown below starts flat but then develops a nice conical shape when put together with the inferior wedge removed.
Because the upper breast border is the more stable (and predictable) landmark, the inframammary fold (IMF) becomes less important. In the past, I marked the new nipple position at the level of the IMF until I realized how variable the fold can be. Some patients not only have a variable footprint location on the chest wall, the distance between the upper breast border and the lower breast border (inframammary fold) can vary from a few centimeters to well over 15 cm.
Because of the variability of the IMF, the Regnault classification of ptosis can be misleading. Paule Regnault classified breast ptosis based on the relationship of the nipple to the IMF. If the nipple was well below the level of the fold, then a mastopexy would be required. Unfortunately, sometimes the nipple is in a good position on the breast mound, but the fold is abnormally high (especially in tuberous breasts) and the approach should instead be to fill the lower pole of the breast and give a better breast shape by centralizing an implant behind the existing nipple position. If the breast is large and the nipple is high then the best approach would be to remove some of the ptotic gland. The nipple should be moved only if it is too low on what will be the final breast mound.
We should instead look at the amount of glandular ptosis or nipple ptosis in relation to the upper breast border and upper pole of the breast. Once the inferior wedge of glandular ptosis is removed, the new nipple position can be easily determined. The ideal nipple position on an average “C” cup breast is about 10 cm down from the upper breast border and about 10 cm from the chest midline (drawn straight – not around the breast).
The upper breast border remains at the preoperative level with a breast reduction or mastopexy but it can be elevated on average 2 cm with an augmentation or mastopexy-augmentation.
It is easier to plan surgery if the surgeon first assesses glandular ptosis and then nipple ptosis. The level of the IMF is the least important landmark. Sometimes it is better to fill the lower pole of the breast (and lower the IMF) with an implant to centralize the breast mound behind the existing nipple position than it is to move the nipple.
It is important for the surgeon to first assess patient desires in terms of size. Any previous biopsies, mammogram results, and personal and family breast history should be outlined. The patient should be asked about past experience and wishes related to pregnancy and breastfeeding.
Then details of other patient requests, such as shape and upper pole fullness, should be determined.
The consultation is far easier if photographs are taken and used for the discussion. The surgeon can then mark on the photos to illustrate what kind of result can be achieved ( Fig. 38.3 ). The upper breast border is marked (here with a dotted line). The distance of “flat” chest wall is marked with the vertical arrow on both the frontal and the lateral views. Note that the drawing shows removal of the glandular ptosis – removal of both inferior and lateral breast tissue where it is in excess. Once the desired inferior border of the breast is determined, the new nipple is placed about one-third up the breast mound. Note that the IMF is not marked – and not needed.
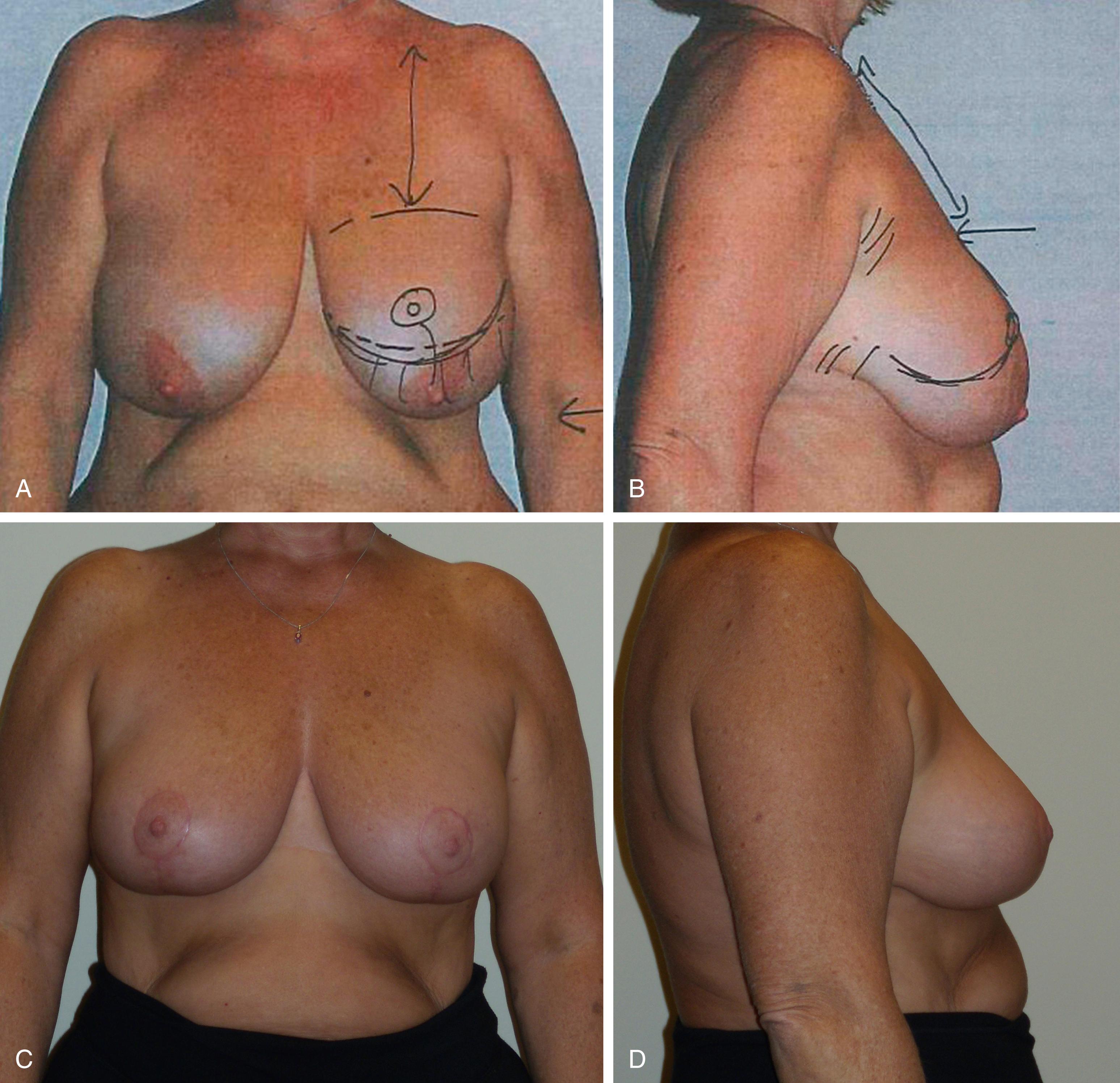
There is still a bit of overhang in the final result because it is difficult to lift the breast completely up onto the footprint without some overhang. Having the breast shape completely confined to the breast footprint is difficult unless the footprint is long vertically or without lowering the IMF (as often happens with an inverted T inferior pedicle breast reduction).
Patients need to be warned that they will not achieve the “double push up brassiere effect” without clothes. There is normally a vertical distance of flat chest wall (this can vary from about 9 cm to 16 cm in an average height patient) between the clavicles and the upper breast border. The breasts do not normally come up close to the clavicle and the upper breast border should never be higher than the preaxillary crease. This has become an important part of managing patient expectations over the past few years with the new fashions in brassieres.
If a patient has very poor upper pole fullness, some of the inferior wedge can be moved up , (separated from all surrounding breast tissue but left attached as a chest wall-based flap) to provide better projection, but any attempt to try to fill the upper pole is usually doomed to failure. The tissue that is mistakenly pushed up will inevitably fall down resulting in unattractive glandular ptosis.
Patients often see more in the photographs than they do in the mirror and by showing patients their photographs, they can better understand the limitations of the procedure. Patients need to understand that they cannot achieve either a higher footprint or more upper pole fullness. They can, however, achieve better projection.
Reduction/Mastopexy
There are numerous designs and labels for various breast reduction and mastopexy techniques. The design should be divided into two categories:
pedicle design, and
skin resection pattern.
The breast is a superficial structure attached to the skin at the nipple. Most of the blood supply to the breast is superficial. It starts out in a deep location around the periphery of the breast and then both the arteries and veins travel around the breast in the subcutaneous tissue.
Most of the blood supply to the breast comes from the internal mammary system ( Fig. 38.4 ). The inferior or central pedicle is supplied by the deep artery and vein that penetrates through the intercostal muscles and the pectoralis muscle from the fourth interspace. That this artery (and venae comitantes) comes from the fourth interspace makes sense because the breast is a fourth interspace structure.
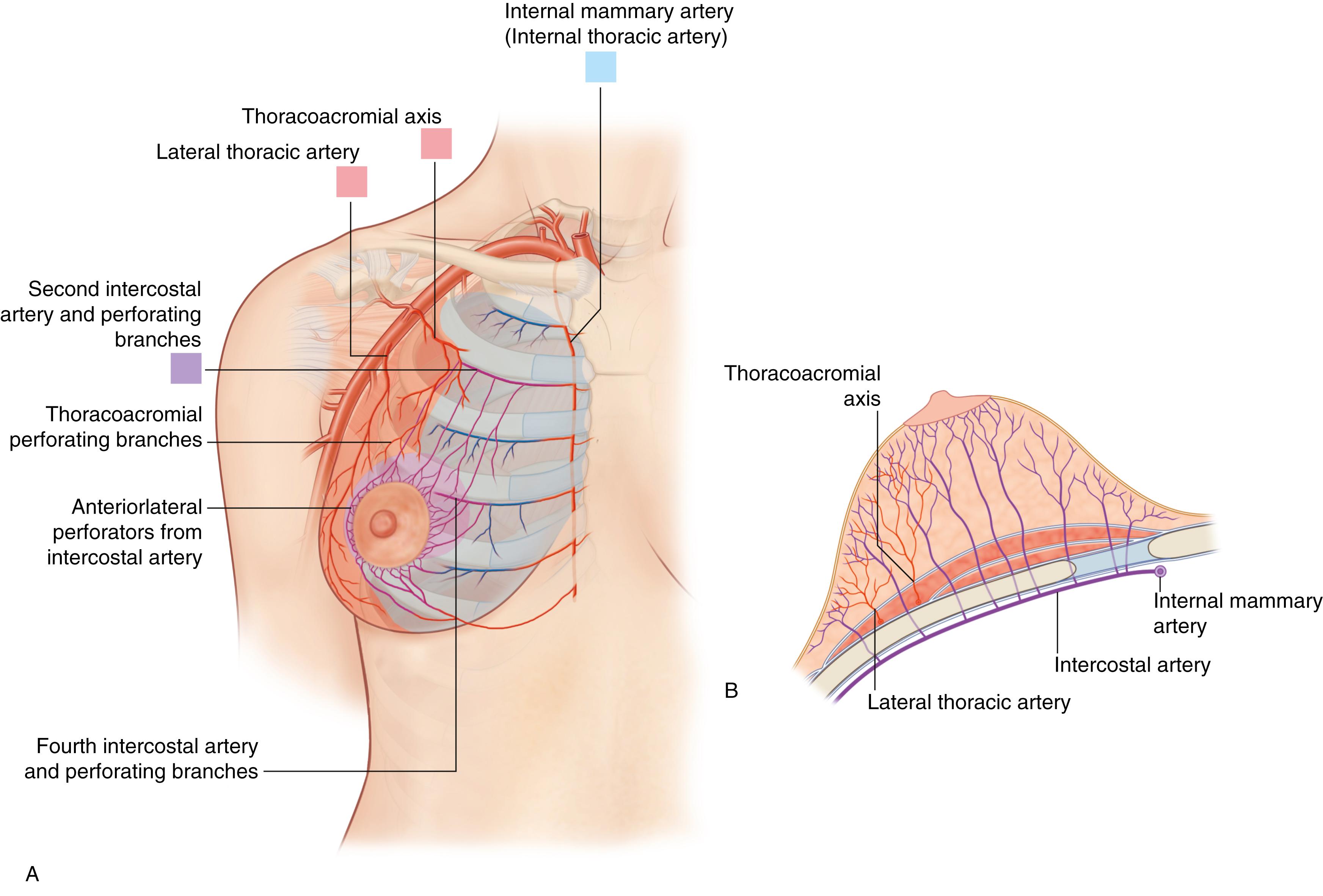
There is also some blood supply from the superficial branch of the lateral thoracic system and this artery supplies a lateral pedicle.
Most of the arteries are within the first centimeter deep to the skin surface at the level of the areola. The veins travel separately from the arteries and they are more superficial – just under the dermis. They can often be seen through the skin when examining the patient and they can be seen to drain mainly superomedially.
Because the blood supply to an inferior or central pedicle comes up through the chest wall, the pedicle must be full thickness. Because the blood supply to the superior, lateral, and medial pedicles is in the subcutaneous tissue the pedicles can be created as dermal-subcutaneous pedicles. The pedicle should be thick where the vessels are deep at the breast periphery and then can be thinned out closer to the areola where the vessels are found usually within the first centimeter of tissue depth beneath the skin.
Pedicle design is based on blood supply. If the surgeon does not believe that there is a safe pedicle available, then a free nipple graft may be an option. Usually, however, there are good pedicle designs that can be used. The main choices are inferior (and central), superior, medial, lateral, or a combination ( Fig. 38.5 ). ,
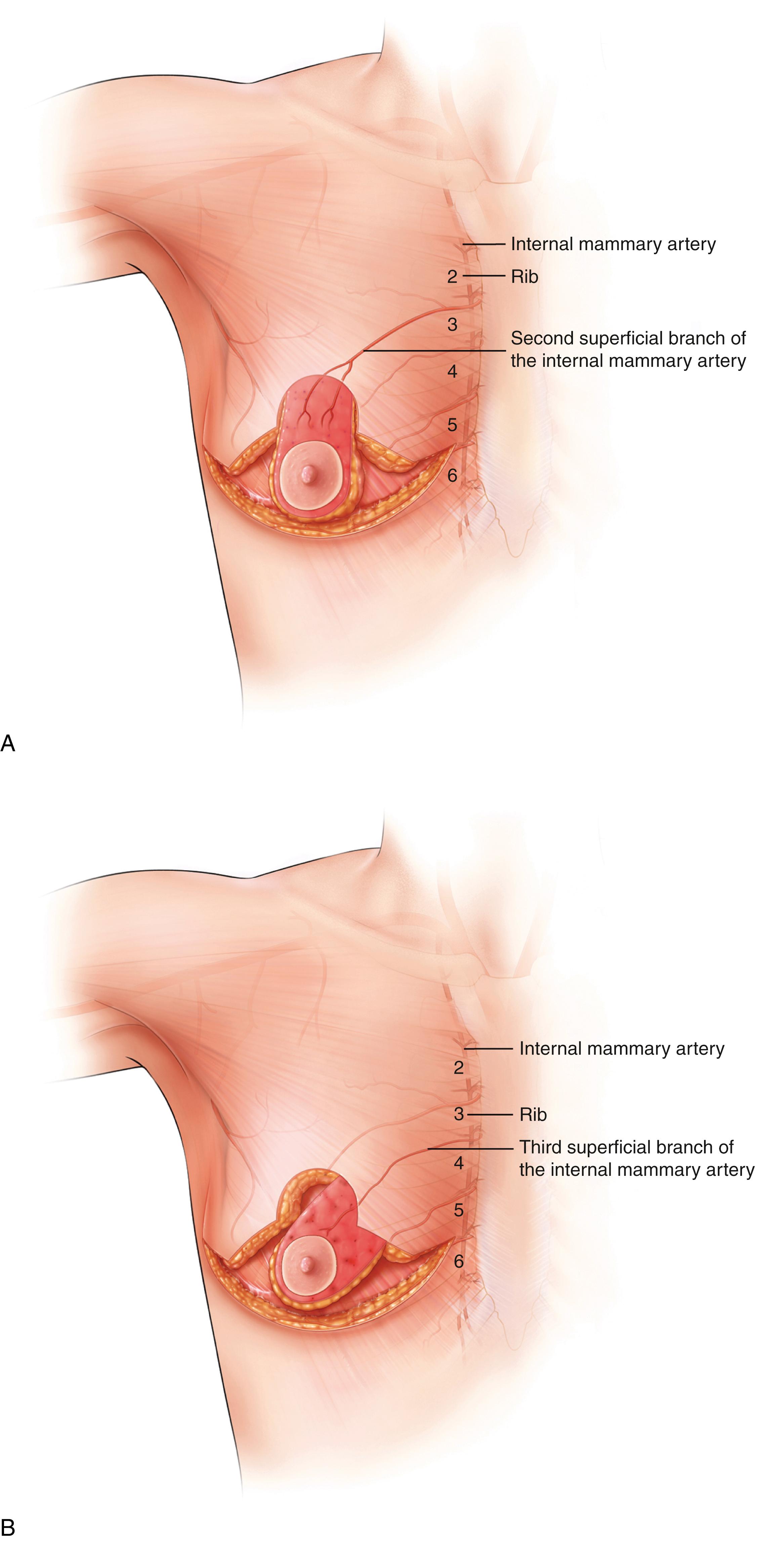
The superior pedicle is supplied by the internal mammary system by the descending branch of the artery from the second interspace and the medial pedicle is supplied by the third interspace. There is clearly some variability but a true superomedial pedicle can be designed to include these two axial arteries.
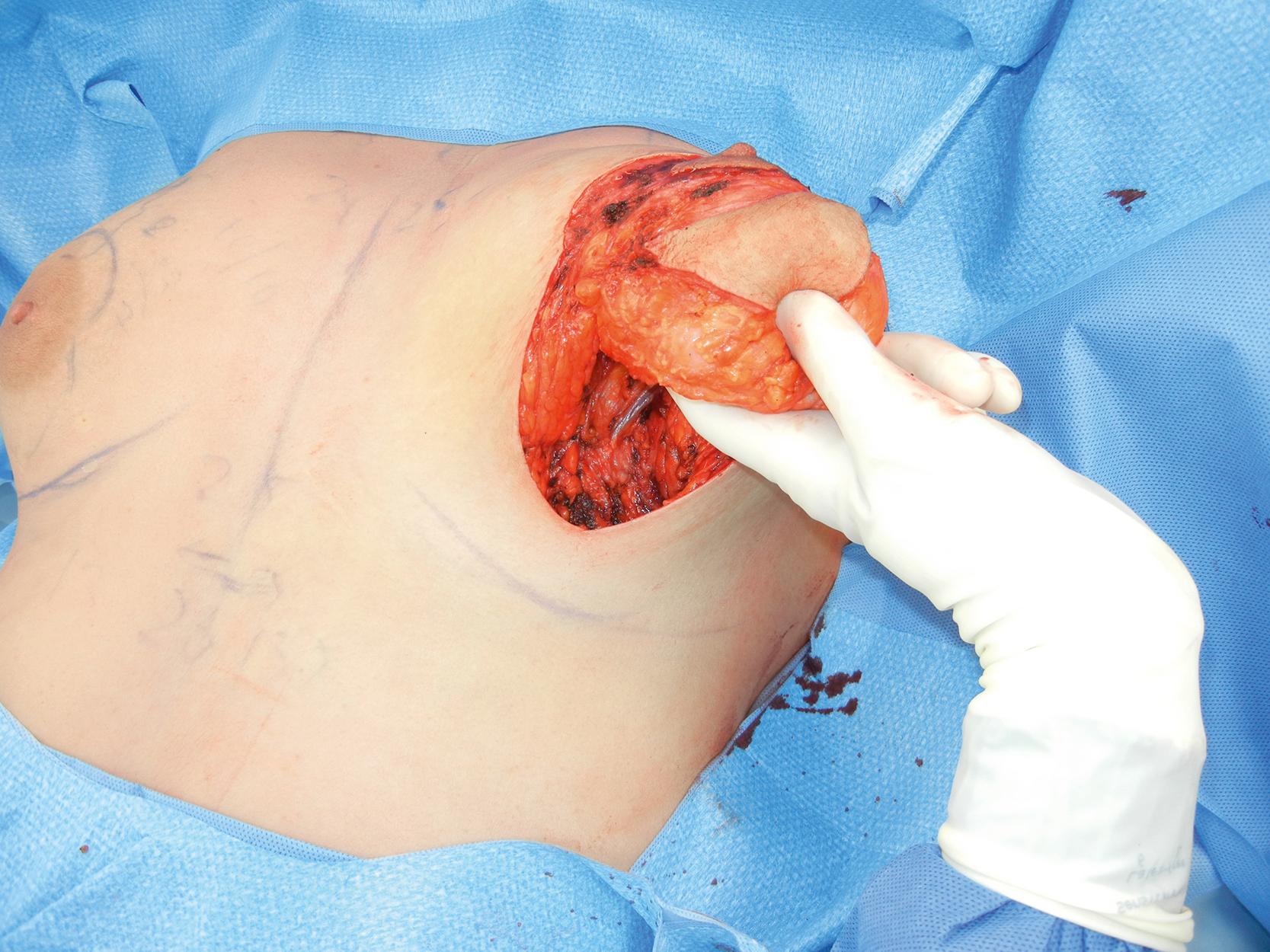
Fig. 38.6 shows the artery and vein to the inferior wedge that is about to be removed in a vertical breast reduction using a true superomedial pedicle.
Innervation to the nipple comes from various sources. There are nerves that come from all directions but they are mainly medial and lateral. There are several medial branches but also a major nerve from the lateral fourth intercostal nerve. This nerve splits with a superficial branch that courses up in the subcutaneous tissue and a deep branch that travels along the pectoralis fascia. The deep nerve branch then turns upward at the breast meridian and can be included in a full-thickness pedicle. Evaluation of my patients has shown that the medial pedicle actually has better return of sensation than either the lateral or superior pedicles. Other studies have shown that there is not much difference in sensation recovery among the various pedicles.
The pedicle design determines the design of the parenchymal resection pattern, but the skin pattern can vary. The classic inverted T (Wise pattern) skin resection pattern , was designed to use the skin brassiere to hold up the remaining breast parenchyma. In those cases where the skin has good elasticity, it can be used to shape the breast.
Unfortunately, skin tends to stretch under tension and many surgeons are now using the inferior wedge resection principle to remove the heavy inferior breast tissue, then closing the pillars together following the Wise pattern for the parenchymal resection and closure instead of using the Wise pattern for the skin resection pattern. The skin resection pattern will then depend on how much skin redundancy there is because it is used to redrape around the breast parenchyma instead of being used as a handle or support.
Not all “vertical” (or “inverted T”) breast reductions are the same. They can be designed with various pedicles. Usually, however, the term “vertical” is associated with the superiorly (superior, medial or lateral)-based pedicles and the term “inverted T” is associated with inferior or central pedicles. The excess breast tissue is removed inferiorly (and laterally) with the superiorly-based pedicles and the excess breast tissue is removed superiorly (and laterally and medially) with the inferiorly-based pedicles.
It makes more sense to work with gravity rather than against it. The inferior pedicle tends to bottom out with time, pushing the IMF down. Over time, the IMF can end up several centimeters below the horizontal scar.
Periareolar skin resection patterns (where the outer doughnut skin edge is sutured to the inner doughnut hole skin edge) are used only rarely because not much skin can be resected. If the patient has a significant amount of redundant skin, then more skin needs to be resected, using either a vertical or inverted T pattern. The breast is not well reshaped when the skin alone is tightened – surgeons need to be aware that Benelli’s description of a periareolar mastopexy did not just tighten the skin; he reshaped the underlying breast parenchyma as well. Failure to follow this advice has resulted in unsatisfactory results.
Some surgeons believe that the inferior pedicle is a safer pedicle for the very large breast reduction. I believe that the true superomedial pedicle has the best blood supply because it includes two axial arteries. I have pencil-Dopplered more than 85 patients and the descending artery from the second interspace is usually just medial and occasionally just lateral to the breast meridian.
When the breast enlarges, the blood vessels also enlarge and travel down with the nipple. The risk in a longer pedicle is not that the blood vessels do not travel to the nipple but that creation of the pedicle might not actually include those particular vessels.
An inferior pedicle (using the inverted T skin resection technique) is the easiest to inset but the weight of the breast is left inferiorly. The medial and lateral pedicles are easy to inset because they rotate into position. The superior pedicle can be harder to inset because it needs to be folded or forced up. Superior pedicles often need to be thinned in order to allow an easier inset without compression and this leaves an empty concave lower pole.
The true superomedial pedicle (with the main base medial but extending upward and across just lateral to the breast meridian) can be harder to inset than a true medial pedicle. But if the surgeon understands that the blood supply is superficial, debulking deep tissue which is causing the restriction can be performed safely. This not only provides a good reliable blood supply but it also gives a nice elegant curve to the lower pole of the breast on the table because the inferior border of the medial pedicle becomes the medial pillar.
The lateral pedicle can be used, but it is often difficult to remove some of the lateral bulk in a breast reduction because the tissue that is in excess (laterally) forms the base of the lateral pedicle. Although there are some veins that drain superolaterally, the majority of the venous drainage is superomedial.
With a mastopexy, breast tissue needs to be rearranged because tightening the skin brassiere alone is not very effective. Patients who have developed ptosis have already demonstrated that their skin envelope cannot hold up the breast parenchyma. A small breast reduction is the easiest mastopexy, especially when an inferior wedge of breast tissue is removed. When the patient wants to maintain their volume, then an inferior flap (described by Liacyr Ribeiro) can be created, moved up, and the pillars closed around caudal to the flap. , When this method of a mastopexy is used, the pedicle is therefore based superiorly (superior, superomedial or superolateral). This method of “moving” breast tissue (that is “removed” in a breast reduction) is a good way of reshaping the breast when the skin brassiere has lost elasticity.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here