Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The goal of surgical management of any cancer of the head and neck is to remove the cancer in its entirety and preserve form and function. Marginal mandibulectomy (MM) evolved as a surgical technique to obtain the margin around the tumor yet avoiding the cosmetic and functional complications of segmental mandibulectomy (SM). Crile first described the MM in 1923 as an incision that is “carried down to the underlying bone, and thence into the bone by a sharp chisel or saw, so that a slice of bone can be split off in one piece, bearing the undisturbed cancer off as on a bone platter.” The three most common locations of cancer of the oral cavity in which MM plays a role include the floor of the mouth, the gingival ridge, and the retromolar trigone, where carcinoma abuts the mandible.
It was once believed that the oral cancers invade the mandible by draining through the lymphatic channels in the mandibular periosteum on their way to the cervical lymphatics. Hence, segmental mandibulectomies and composite resections were performed for oncologic completeness. Reconstructive surgery was still in rudimentary stages so that resections resulted in suboptimal cosmetic and functional outcomes, including malocclusion, temporomandibular joint dysfunction, Andy Gump deformity, tracheostomy, and gastrostomy tube dependence. Marchetta et al. later demonstrated that mandibular involvement occurs predominantly via direct invasion of the periosteum. This finding eliminated the mandate for SM. Furthermore, Barttelbort et al. proposed a theory of tumor invasion of the mandible. The cancer initially quickly invades the broad plane of the mandible superior to the mylohyoid muscle attachment. Involvement of the inferior lingual cortical plate occurs infrequently and late. Because of this theory, MM became a feasible procedure for removal of the cancer without compromising the mandibular arch.
The local recurrence and survival rates after segmental and MM were shown to be comparable (though one must be aware of the patient selection bias: Patients with gross bone involvement require a more extensive procedure). MM became an oncologically sound procedure in the management of oral cavity cancers and securing the margin around the cancer. The adverse cosmetic and functional outcomes are limited by preservation of the architecture of the mandibular arch and native muscular attachments. In addition, dental rehabilitation is a viable option in the form of a removable dental plate or dental implants. A major and legitimate concern with this procedure is the inability to obtain reliable intraoperative bone margins. Hence, careful preoperative planning must be executed.
The goal of MM is to secure the margin around the cancer.
Proper patient selection is the key: Meticulous preoperative clinical and radiologic evaluation should be performed to rule out bone involvement.
Osteotomies must be planned before the surgery.
Osteotomies should be placed with assurance of preservation of healthy residual teeth and allowing for dental rehabilitation.
Most recurrences occur in the soft tissues, not the bone. Hence, careful intraoperative frozen section analysis should be used to avoid recurrence in the soft tissues.
Most MM defects can be successfully reconstructed with the split-thickness skin graft.
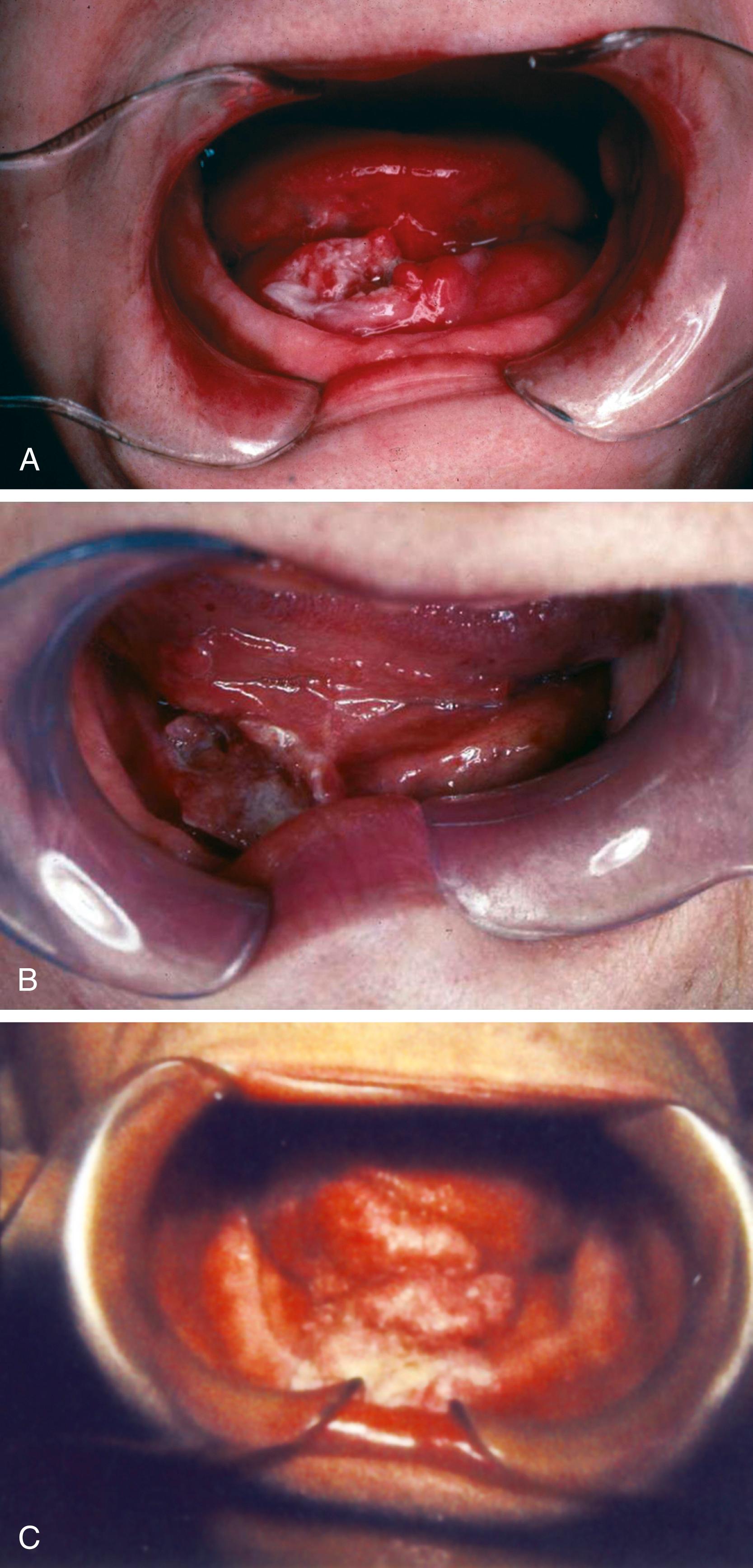
Despite invention and advancement of many sophisticated diagnostic imaging techniques, physical examination remains the mainstay in decision making. Invasion of the mandible should be suspected and assessed in any patient with an ulcerative lesion within the vicinity of oral or lingual cortices, as up to one-third of cases of histologically proven mandible invasion do not show clinical signs of bone invasion preoperatively. Tsue et al. and Werning et al. independently observed that the location of the primary cancer was predictive of mandibular invasion: Bone invasion was more likely to be present in cancers of the floor of the mouth, retromolar trigone, and inferior alveolar ridge. The presence of dentition was shown to influence perineural invasion. The inferior alveolar nerve was four times more likely to be involved by the cancer in the edentulous mandible than in the partially dentate mandible. The resorption of the alveolar ridge appears to be greater in the edentulous mandible, which places the nerve in a more superficial position, making it more susceptible to invasion of the cancer. Bimanual palpation allows the surgeon to determine whether the tumor is fixed to the bone, signifying bone invasion. The examination may be limited by pain and might require topical or even a general anesthetic ( Fig. 181.1 ).
Werning et al. demonstrated that clinical evaluation of mandibular bone invasion was more sensitive than radiologic assessment (a mixture of Panorex, occlusal views, routine radiographs, and computed tomography [CT]) (sensitivity of 73%), while radiologic evaluation was more specific (specificity of 82%) and had a higher reliability index (0.29 vs. 0.19). They concluded that the combination of clinical and radiologic evaluations is more accurate than either one alone. A newer tomographic modality, single positron emission CT (SPECT), was shown to have 87% overall accuracy in predicting bone invasion, as compared to 71% for clinical examination, CT scanning, and Panorex. SPECT sensitivity approached 95%, as compared to 55% for conventional CT and 50% for Panorex. Another tomographic evaluation named Dentascan was found useful in evaluation of the buccal and lingual mandibular cortices. The Dentascan images consist of panelliptical and parasaggital views derived from the reformatting of the regular axial CT images. Brockenbrough et al. demonstrated sensitivity of 95%, specificity of 79%, positive predictive value of 87%, and negative predictive value of 92% for Dentascan. One of the immediately obvious limitations of CT scanning in the oral cavity is dental artifact. Magnetic resonance imaging (MRI) does not have this shortcoming and may be more useful in the evaluation of medullary bone. It also produced promising results: Sensitivity of MRI in detecting mandibular invasion was 93% with 93% accuracy.
Tumor so close to the mandible that it is not feasible to obtain an adequate margin of resection without removing the alveolar process of the mandible
Abutment of the lesion to the lingual aspect of the periosteum of the mandible
Tumor that crosses the alveolus and into the gingivobuccal sulcus
Absolute
Gross destruction of the bone
Invasion by cancer of the mandibular canal
Relative
Edentulous mandible with reduced vertical height
The concern in question is sacrifice of the endostial blood supply, placing the remaining bone at risk of avascular necrosis and a pathologic fracture.
Previously radiated mandible
While there is usually a single port of cancer entry into the bone in radiation-naïve mandible, histologic analysis of previously radiated bone demonstrates multiple tumor loci. This finding suggests that the radiation alters bone resistance to tumor spread, likely by impairing the periosteal blood supply and weakening it, making the pattern of spread less predictable and posing a real risk of leaving cancer behind by performing subtotal resection.
While clinical assessment in combination with radiographic evaluation is of paramount importance, direct examination of the bone under the periosteum remains the gold standard for identifying mandibular invasion.
In addition to the informed consent, preoperative patient counseling must also encompass discussions of postoperative airway and nutrition management, which may include temporary tracheostomy and placement of a nasogastric tube. In addition, various reconstructive options should be reviewed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here