Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The importance of facial aesthetics was recognized as early as 55 BC when Cicero (106–43 BC) wrote in De Oratore, Volume III, “Everything is in the face ....” The face forms an integral part of one’s life, and each face can be considered “custom made.” All faces have a forehead, two eyes, a nose, a mouth, two ears, and a chin, and yet we manage to look significantly different from each other. Facial beauty, however, can be recognized when there is good balance and harmony among the different parts of the face. Harmonious shape and form of the individual parts of the face (i.e., the nose and the chin) will certainly further enhance facial beauty.
The mandible forms a large part of the lower half of the human face and is, often subconsciously, associated with “character” or “personality.” A deficient chin is generally associated with femininity, whereas a strong square chin is associated with masculinity. The need for a strong biting action gradually became redundant with the discovery of fire—about 700,000 years ago. Cooking and tenderizing food removed the need for a large, strong lower jaw and musculature. Human facial features, particularly the mandible, have responded to environmental changes in different parts of the world over many thousands of years. Today, each of the myriads of faces in the world is an expression of subtle genetic mutations. In the long term, however, globalization will unify global considerations and standards of facial attractiveness and beauty.
Although the chin is a nonfunctional entity, it forms an integral part of the rest of mandibular aesthetics and, ultimately, facial aesthetics. One may therefore consider that surgical correction of the form, size, and shape of the chin is responsible for mandibular aesthetics and that total skeletal mandibular surgery should correct function and the overall position of the chin in the space. Genioplasty is, however, performed to normalize the form, shape, and size of the anterior mandible; it is not a substitute for mandibular surgery.
The purpose of this chapter is to concentrate on the aesthetic considerations, evaluation, and correction of mandibular dentofacial deformities by means of orthognathic surgery. The aesthetic correction of mandibular deformities will be considered with regard to three components: (1) the genial component, which represents anterior aesthetics; (2) the corpus-and-ramus component, which is responsible for the anteroposterior and transverse positions of the mandible; and (3) the dentition, which is responsible for oral function.
Dental compensation: Compensation is the term used to refer to the natural tendency of teeth to tilt to decrease occlusal discrepancies. For instance, in class II malocclusion, dental compensation occurs in relation to the tendency of the maxillary anterior teeth to become retroclined and that of the mandibular teeth to become proclined. The degree of dental compensation is assessed on a lateral cephalometric radiograph, and it is important to take the degree of dental compensation into account when planning surgery. Orthodontists may compensate the dentition to camouflage the skeletal discrepancy. Planning of surgical procedures is based on teeth that are in the uncompensated position. In compensated occlusion, the degree of potential mandibular movement may be underappreciated, given the relationship of the compensated occlusion before surgical correction the teeth need to be decompensated by the orthodontist.
Mastication: It is important to inquire about difficulties with mastication. Patients with dentally uncompensated retrognathia typically have an increased overjet, which compromises the ability of the incisors to cut and shear foods during mastication.
Airway obstruction: In patients with retrognathia, it is important to inquire about any history of snoring or sleep apnea. If sleep apnea has not been diagnosed but there is suspicion based on the patient’s history, a sleep study should be ordered and the results incorporated into the treatment plan. If sleep apnea is present, a two-jaw procedure may be indicated to open the airway while correcting the occlusion.
Aesthetic considerations: Although orthognathic surgery is a reconstructive procedure, it is important to consider the aesthetic consequences of skeletal movement. In particular, when planning treatment for the correction of prognathia, it is important to be aware of soft tissue redundancy and submental fullness, which may result from posterior positioning of the lower jaw. Occasionally, even though the sella–nasion–B-point (SNB) is increased and the sella–nasion–A-point (SNA) is normal, the aesthetic result may be enhanced by correcting the occlusion with upper jaw advancement to optimize the soft tissue drape over the underlying skeletal relationship.
Syndromes: Many syndromes are associated with mandibular deficiency and should be identified before treatment. Although the treatment may not require technical modifications, it is important to be aware of any associated syndromes before treatment is started.
Asymmetry: Lower facial third asymmetry is not an uncommon finding in patients with dentofacial deformities. Most patients with a Class III mandibular anteroposterior excess will present with asymmetry. It is important to note whether the asymmetry is due to mandibular deviation, mandibular asymmetry, or any asymmetry of the chin relative to the mandible. Additionally, there may be maxillary asymmetry associated with mandibular asymmetry, which will require movement of the upper jaw as well.
Relationship to chin: In patients who are concerned about the aesthetic impact of insufficient mandibular projection but demonstrate mild or minimal occlusal abnormality, advancement of the chin is a treatment option that frequently achieves the patient’s aesthetic goals without subjecting the patient to sagittal split osteotomy. It is however important to note that genioplasty is not a substitute to mandibular surgery.
Neoplasm: Infrequently, a neoplasm may be the source of excessive mandibular growth. A neoplastic etiology typically presents as an asymmetrical mandible, with teeth out of occlusion. The rapidity of tumor growth will produce a mandibular shift that exceeds the ability of the maxillary teeth to remain in occlusion. Mandibular asymmetries without crossbite are typically associated with more chronic processes, such as hemifacial microsomia, or an early history of condylar trauma.
Trauma: Injury to a condyle before skeletal maturity may stunt growth, leading to mandibular asymmetry and crossbite and anterior open bite.
Autoimmune: Rheumatoid arthritis can cause condylar resorption resulting in an anterior open bite or mandibular retrognathia. It is important to ensure good medical control of the disease before undertaking surgical correction.
Developmental anomalies: Various developmental anomalies, such as Pierre Robin sequence, hemifacial microsomia, or congenital syndromes, may result in hypoplastic mandibles. By the time these patients are old enough to be considered for surgery, the underlying etiology has typically been elucidated and should be considered when developing the final surgical plan.
Endocrine: Acromegaly and other hormonal abnormalities can lead to anomalies of mandibular size and position.
The clinical evaluation must be the primary diagnostic tool in determining surgical treatment of the patient with dentofacial derformities, and cephalometric evaluation serves as a helpful diagnostic guide. Cephalometric radiography also enables the clinician in quantification and classification, as well as communication with colleagues and helps create a treatment plan via a visual treatment objective, plan for tooth extractions, monitor progress during treatment, evaluate treatment results, and study facial growth.
The face should always be evaluated with teeth in occlusion and the lips in repose.
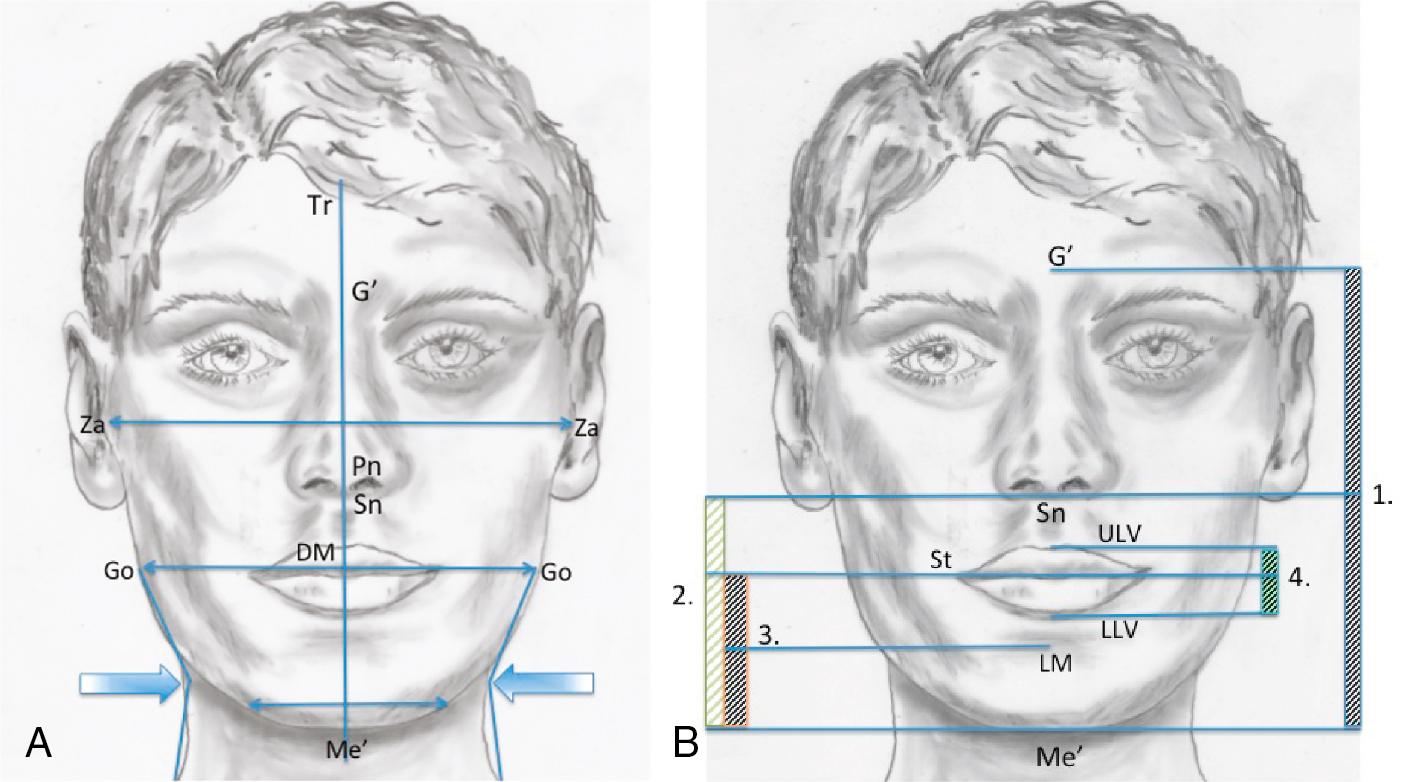
The shape, form, and size of the chin should be in harmony with the particular facial and body type (“corporo–cephalic” relationship) and the gender of the patient. The mandible should have a well-defined, smooth lower border, from the angle to the chin, with a definite separation of the lower third of the face from the neck. The neck relative to the mandibular lower border takes on a subtle hourglass appearance, with its superior aspect being well defined by the concavity immediately below the inferior mandibular borders ( Fig. 21.1 A). The mandibular borders become less defined in the presence of tissue laxity, lipomatosis, chin deficiency, and/or a low hyoid bone.
Transverse dimensions: Individuals with leptoprosopic (narrow and long) facial features also often have a transversely deficient, “pointed” chin that seems separate from the mandible, while dolichoprosopic (broad and wide) faces often have strong broad chins (see Fig. 21.1 A).
Symmetry: The symmetry of the chin is evaluated in relation to the facial midline (Tr-G’-Po-Sn-Me’) as well as the lower dental midline. In cases with mandibular asymmetry, the orthodontist should align the lower dental midline to the midline of the mandible (see Fig. 21.1 A). Mandibular asymmetry would be corrected simultaneously with correction of dental midline asymmetry.
Vertical dimensions: The ratio of the middle and lower facial thirds should be 1:1. The middle third is measured from the glabella (G’) to the subnasale (Sn) and the lower facial third from the Sn to the soft tissue menton (Me’). When an increased lower facial height is present, the clinician should differentiate between vertical maxillary excess and vertical mandibular excess ( Fig. 21.1 B). When the lower facial third is decreased, the clinician should differentiate among vertical maxillary deficiency, deep bite malocclusion, and vertical mandibular deficiency.
Lower facial third: The lower lip and chin should comprise two thirds of the lower facial height (females: 40 ± 2 mm; and males: 44 ± 2 mm) measured from the lower lip stomion (Sti’) to the soft tissue Me’. The height of the lower lip Sti’ to the depth of the labiomental (LM) fold should be equal to the distance from the LM fold to the soft tissue Me’ (see Fig. 21.1 B). The upper lip vermilion (ULV) is usually 25% thinner than the lower lip vermilion (LLV). This relationship (ULV/LLV) will be changed in class II malocclusion, where the lower lip is usually everted, whereas in class III malocclusion, the LLV will be thinner in relation to the ULV (see Fig. 21.1 B). Ethnic differences should also be considered in this assessment.
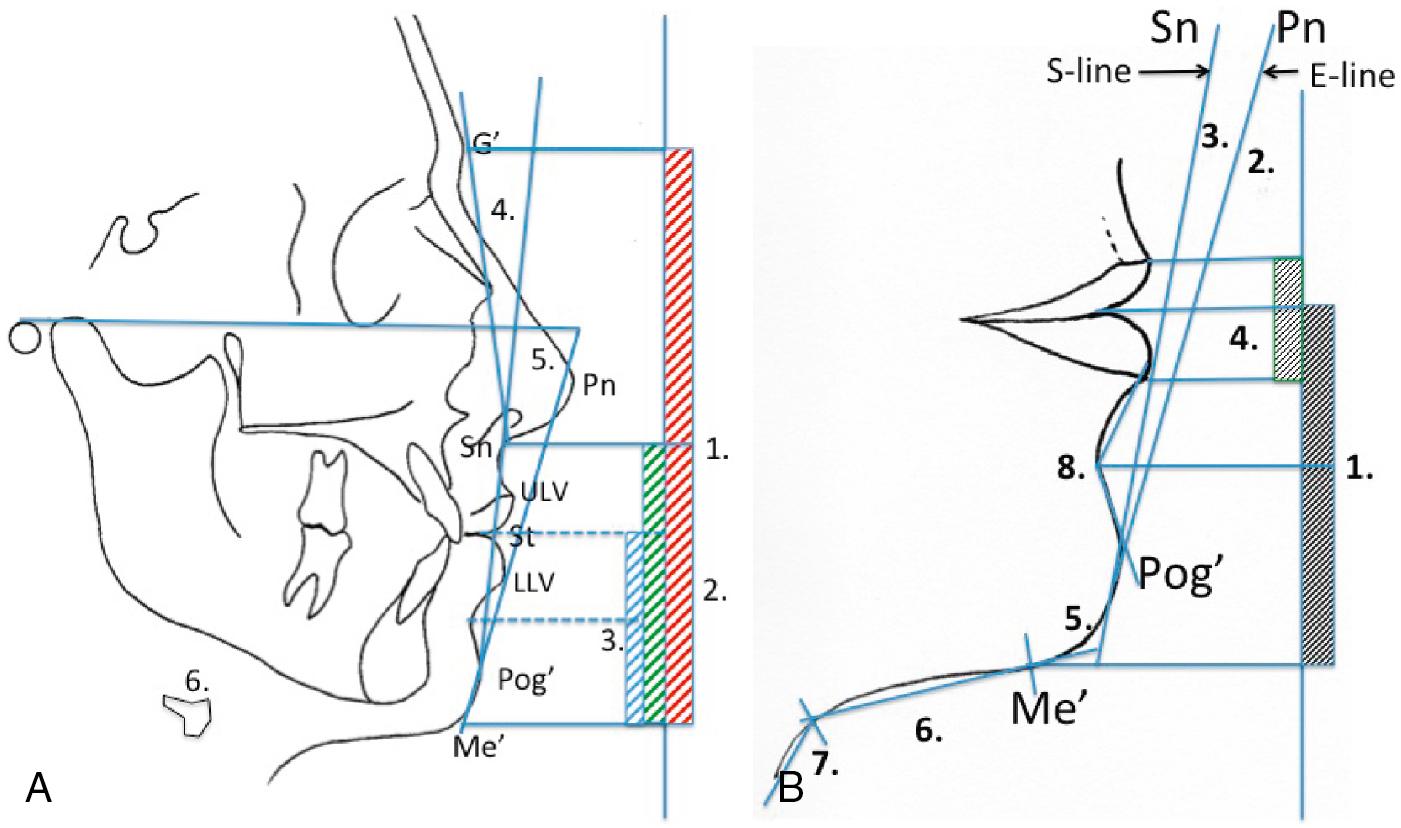
The main contributing factors responsible for the shape and contour of the chin are the anteroposterior position of the lower lip; the depth and height of the LM fold; and the shape of the chin button. Although the following factors should be assessed clinically, angles and linear measurements can be more easily and accurately measured on a lateral cephalometric radiograph ( Fig. 21.2 A, B).
Lower lip position: In class II malocclusion, with an increased overjet, the lower lip is usually everted, and the LM fold is acute. The lower lip will curl forward and downward as it becomes impinged in the increased overjet. Conversely, in class III malocclusion, the lower lip will curl backward and the LM fold will be obtuse as a result of poor lip support by the lingually inclined (compensated) lower incisors.
Labiomental fold: The chin should have a gentle S-curve from the lower lip to the lower border of the mandible. The LM fold is an angle formed by the lower lip and a line tangent to the superior convexity of the chin and should be ±130 degrees. The angle is usually acute in class II mandibular anteroposterior deficiency and obtuse in class III mandibular excess. This angle is often accentuated in class II malocclusion due to an everted lower lip resulting from the influence of the upper incisors. The lower lip will roll back following mandibular advancement. The surgeon considering genioplasty should assess not only the anteroposterior position of the pogonion (Pog’) but also the chin shape and the depth and height of the LM fold (see Fig. 21.2 A).
Chin button: During assessment of the shape of the chin button, the clinician should differentiate between individuals with macrogenia (prominence of the chin button) and mandibular anteroposterior excess (well-shaped chin but total mandibular excess) and individuals with microgenia (deficient chin button) and total mandibular anteroposterior deficiency. These entities may also occur in combination.
Lip–chin–submental angle: This angle is formed by the lip–chin line (from the labrale inferius to Pog’) and a submental tangent. Angles of ±126 degrees for males and ±121 degrees for females are considered aesthetically pleasing. The angle will be acute in patients with class III mandibular anteroposterior excess and/or patients with macrogenia, whereas it will be obtuse in patients with class II mandibular anteroposterior deficiency and/or microgenia. An everted lower lip and/or excessive submental fat will increase the submental angle. Submental lipomatosis often exists independently of generalized body fat. The fat usually exists between the skin and the platysma muscle and can easily be assessed with gentle pinching of the skin (see Fig. 21.2 A, B).
Chin–throat length: This measurement is made from the submental neck point to the soft tissue Me’ and should be 42 ± 6 mm. In class II mandibular recession, the chin–throat length is decreased, and in class III mandibular prognathia, it is increased. This measurement is significant in differentiating between mandibular anteroposterior excess and maxillary deficiency. Mandibular setback would obviously reduce this length and may negatively affect aesthetics (see Fig. 21.2 A, B).
Chin–throat angle (cervicomental angle): The angle is formed by a submental tangent and a line tangent to the neck (females: 121 degrees; and males: 126 degrees). Individuals with macrogenia and mandibular anteroposterior excess will have an acute angle, whereas individuals with microgenia and mandibular deficiency will have an obtuse angle (see Fig. 21.2 A, B).
Modern approach in treatment planning and surgical navigation by means of three-dimensional (3D) computer-aided studies has had a significant impact on orthognathic surgery. Cephalometric evaluation, however, remains the gold standard for the assessment and diagnosis of dentofacial deformities. The primary objective of orthognathic treatment is to make the facial appearance more normal, not to make the patient’s cephalometric measurements more “normal.” It is recommended that the cephalometric radiograph be taken with teeth on centric occlusion (CO) and the lips in repose. In cases where there is a significant difference between CO and centric relation (CR), a second radiograph is made to document CR and to study the “true” relationship between the mandible and the maxilla. This may often prove to be difficult.
Although aesthetic and structural considerations demand assessment of all the facial structures, this chapter will concentrate on aesthetic surgery of the mandible. For descriptive purposes, it will be assumed that the maxilla and the upper dentition are in the normal position.
The soft tissue landmarks are shown in Fig. 21.2 A. (Only the landmarks used in the text are shown.)
Glabella (G’): The most anterior point of the forehead
Nasion (N’): The deepest point of the concavity in the midline between the forehead and the nose
Pronasale (Pn): The most anterior tip of the nose
Subnasale (Sn): The point where the upper lip merges with the columella in the midsagittal plane
Labrale superior (Ls): The mucocutaneous border of the upper lip vermilion
Stomion superius (Sts): The lowest point of the upper lip vermilion
Stomion (St): The midsagittal point where the lips touch in repose
Stomion inferius (Sti): The uppermost point of the lower lip vermilion
Labrale inferius (Li): The mucocutaneous border of the lower lip vermilion
Pogonion (Pog’): The most anterior point of the chin in a midsagittal plane
Menton (Me’): The lowest point on the contour of the chin
The facial contour angle is the angle of facial convexity, contained between a line drawn from G’ and Sn (the upper facial plane [UFP]) and a line drawn from Sn to Pog’ (the lower facial plane [LFP]). The mean angle for females is 13 ± 4 degrees and for males 11 ± 4 degrees. Individuals with mandibular deficiency and/or microgenia will have a more convex profile (increased facial contour angle), whereas individuals with prognathism and/or macrogenia will have straighter or even concave profiles (decreased facial contour angle). It is, however, important to keep in mind that vertical maxillary deformities (vertical maxillary excess or deficiency) will influence this assessment due to clockwise or counterclockwise rotation of the mandible around the condyles (see Fig. 21.2 A).
E-line: This line is also called the “aesthetic plane” and is formed by a line drawn from the tip of the nose (Pn) to Pog’. The upper lip should be 4 mm behind the line, and the lower lip should be 2 mm behind it. The soft tissue profile behind the line should form a symmetrical “Cupid’s bow” shape. The anteroposterior position of the chin, the nasal tip projection, and the lip support by the incisors will influence this assessment (see Fig. 21.2 B).
S-line: The upper and lower lips should touch the S-line, which is drawn from Pog’ to the midpoint of the S-shaped curve between Sn and Pn. If the lips are behind this line, it may indicate lack of lip support or a prominent chin. The lips may fall in front of this line because of dental protrusion or a deficient chin ( Fig. 21.2 B).
Z-angle: The Merrifield Z-angle is formed by the intersection of the Frankfurt horizontal (FH) plane and a line connecting Pog’ and the most protrusive lip point (upper or lower). The average Z-angle is 80 ± 9 degrees. An angle greater than the previously mentioned is indicative of mandibular anteroposterior excess, whereas an angle less than the above will indicate mandibular deficiency. The Z-angle also indicates the relationship of the lips to the chin, as well as possible chin prominence or deficiency (see Fig. 21.2 A).
Hyoid bone level: Normally, the hyoid cartilage is situated 20 mm below the lower border of the mandible and just below the lower molar teeth. When the hyoid cartilage is situated more anterior and/or inferior than the norm, isolated soft tissue procedures in the neck will have limited results (see Fig. 21.2 A).
Relationship of the middle third height to the lower third height: The distance from G’ to Sn (middle third height) and from Sn to Me’ (lower third height) is measured, and the ratio should be approximately 1:1.
Lower lip–chin height: This measurement is made from Sti to Me’ and should be 44 ± 2 mm for males and 40 ± 2 mm for females. An increase may indicate an increased anterior mandibular (chin) height. A decrease may however indicate a short mandibular (chin) height or a deep bite and everted lower lip.
Labiomental fold: The lower lip, the depth of the LM fold, and the chin button should form a smooth and harmonious S-shaped curve, with the labiomental fold dividing the lip–chin height (Sti–Me’) into approximately equal halves (see Fig. 21.2 B). The angle is acute in patients with class II dentoskeletal deformities caused by an everted lower lip or in patients with macrogenia. Individuals with class III dentoskeletal deformities and retroclined (compensated) lower incisors or those with microgenia will exhibit an obtuse LM angle.
The hard tissue landmarks shown in Fig. 21.3 include the following (only the landmarks used in the text are shown):
Glabella (G): The most anterior point of the frontal bone
Sella (S): The center of the sella turcica
Nasion (N): The most anterior point on the frontal nasal suture in the midsagittal plane
Orbitale (O): The lowest point on the inferior orbital rim
Anterior nasal spine (ANS): Anterior tip of the anterior nasal spine
B-point (Supramentale) (B): The most posterior midline point in the concavity of the of the mandibular symphysis
A-point (Subspinale) (A): The most posterior point in the concavity where the lower edge of the anterior nasal spine meets the alveolar bone covering the maxillary incisors
Pogonion (Pog): The most anterior point of the chin
Menton (Me): The most inferior point of the symphysis of the mandible in the mid sagittal plane
Porion (Po): The most superior point of the external auditory meatus
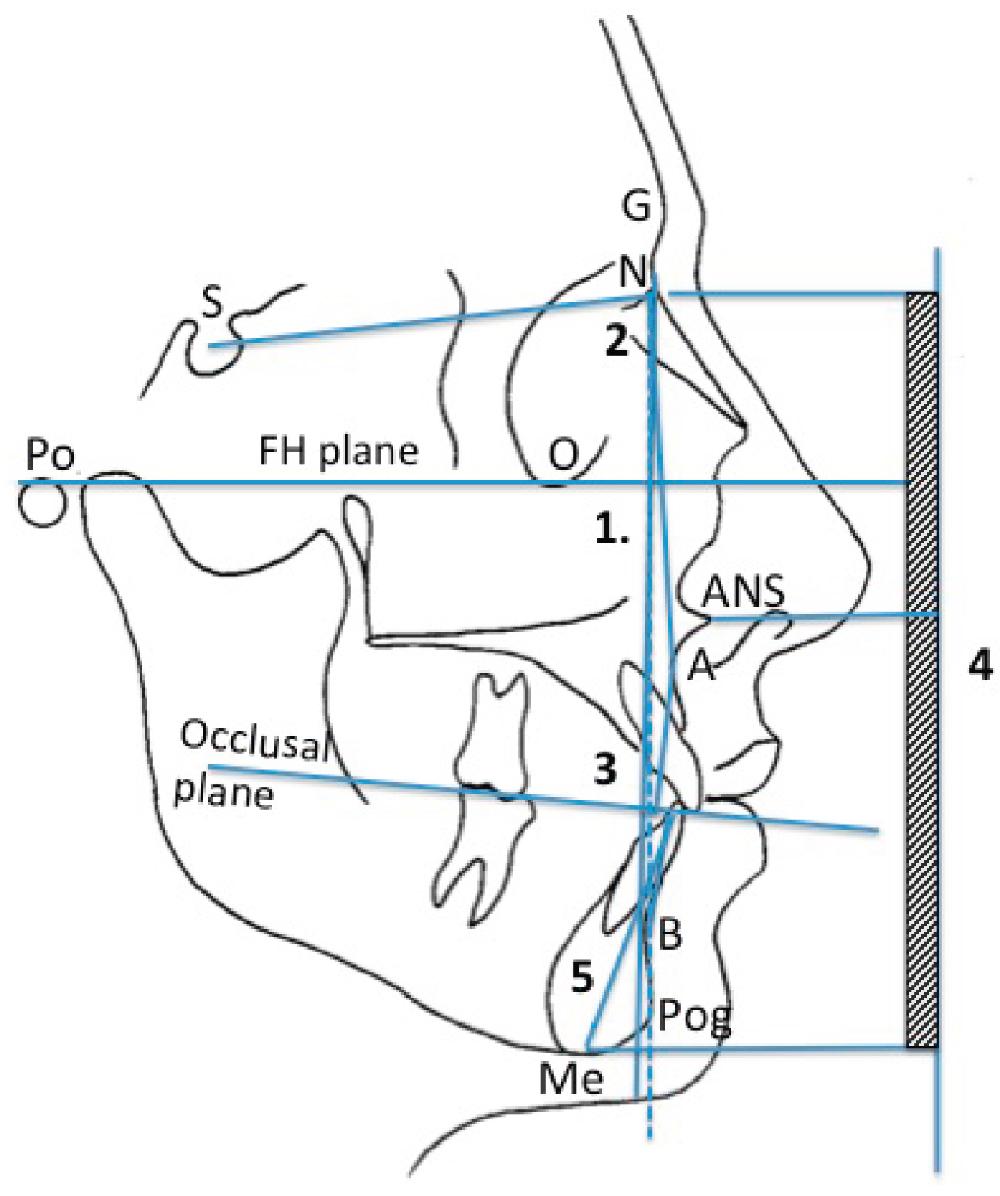
Facial angle: The facial plane is a vertical line and extends from N perpendicular to the FH plane. The FH plane extends from Po to Or. The angle between these two planes should be 82 to 95 degrees. This angle indicates the anteroposterior relationship of the bony chin, to the cranium. Small values indicate a recessive chin, and large values indicate a prominent chin ( Fig. 21.3 ).
SNB angle: The SNB angle is formed between the anterior cranial base (S-N) and a line connecting B-point and N. Its mean is 80 degrees. The angle gives an indication of the anteroposterior position of the mandible relative to the anterior cranial base. Individuals with an angle greater than 80 degrees will tend to have mandibular excess, whereas individuals with mandibular deficiency will have an SNB angle less than 80 degrees. This measurement should, however, always be assessed in relation to the SNA angle, which indicates the maxillary anteroposterior position in relation to the anterior cranial base (see Fig. 21.3 ). The ANB angle (normal + 2 degrees) indicates skeletal discrepancies between the maxilla and the mandible.
Wits appraisal: The Wits appraisal is a linear measurement of the distance between the maxilla and the mandible and is not influenced by the cranium. Points BO and AO are established by dropping perpendicular lines from A-point and B-point, respectively, onto the occlusal plane. The mean in males is for BO to be 1 mm in front of AO in males, and BO and AO to coincide in females. A small discrepancy may indicate that the malocclusion can be treated orthodontically, whereas a large discrepancy may indicate that surgical correction is indicated (see Fig. 21.3 ).
Midface and lower face skeletal vertical heights: Perpendicular lines are drawn from N, ANS, and Me to a vertical line perpendicular to the FH plane. The vertical skeletal relationships are measured from N to ANS and from ANS to Me. The normal skeletal midface height is 53 mm and that of the lower face is 65 mm (ratio 5:6). The ratio is more important than the actual measurement. In most individuals with vertical dentofacial deformities, the lower measurement (ANS–Me) will be affected. The ANS–Me distance will be increased in individuals with vertical maxillary excess, vertical mandibular excess, and, in most individuals, open bites. The lower measurement will be decreased in individuals with vertical maxillary deficiency, vertical mandibular deficiency, and closed or deep bites (see Fig. 21.4 ).
Anterior mandibular height (mandibular dental height): This height is measured from the lower incisor tip to Me and should be 44 ± 2 mm for males and 40 ± 2 mm for females. The clinician should differentiate between incisor extrusion and an accentuated curve of Spee and skeletal vertical excess of the chin (see Fig. 21.4 ).
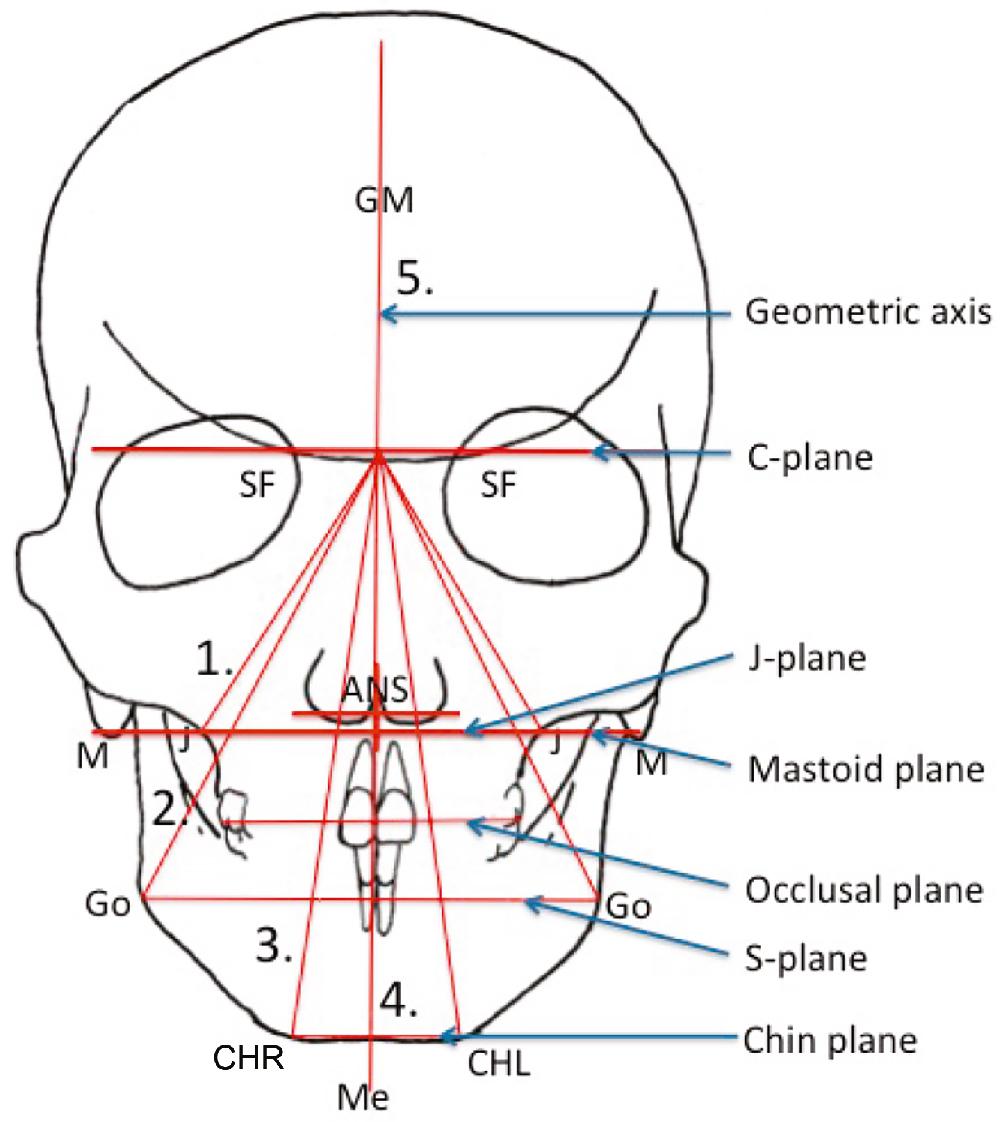
Patients with facial asymmetry will need, in addition to lateral cephalometric analysis, a posteroanterior radiographic analysis. Most asymmetrical dentofacial deformities have 3D components, and a 3D digital computerized study is extremely helpful in analysis and treatment planning in these cases.
Only the hard tissue cephalometric landmarks used in the text are shown in Fig. 21.4 and include the following:
SF: The point where the small wing of the sphenoid bone crosses the medial orbital ridge
Anterior nasal spine (ANS): The center point at the base of the nose
Jugulare (J): The most superior, medial point on the zygomatic buttress
A: The maxillary dental midline
B: The mandibular dental midline
Y: The most lateral point on the buccal surface of the first upper molar (YL for left and YR for right)
Z: The most lateral point on the buccal surface of the first lower molar (ZL for left and ZR for right)
Gonion (Go): The most inferior posterior point at the angle of the mandible
Menton (Me): The most inferior point of the chin in the midline
CH: The most inferior lateral point of the chin (CHL for left and CHR for right)
Mastoid (M): The most inferior point on the mastoid bone
The posteroanterior cephalometric planes are shown in Fig. 21.4 and include the following:
Cranial base plane (C-plane): A horizontal line connecting the SF points
J-plane: A line connecting the left and the right J-points
Occlusal plane: A line connecting the occluding points of the upper and lower molar cusps (Y-left and Y-right)
S-plane: A line connecting the left and right Go points of the mandible
Chin-plane: A line on the inferior border of the chin connecting the left and right CH-points
Mastoid plane (D-plane): A line connecting the left and right M-points
Geometrically constructed vertical axis (GM): This axis is constructed by dividing the C-plane and D-plane, connecting these two points and extending it to the chin
Maxillary triangle: The triangle is constructed by connecting the midpoint on the C-plane (C-point) to the left and right J-points.
Mandibular triangle: The triangle is constructed by connecting C-point with Go bilaterally.
Chin triangle: Connecting C-point with the left and right CH points forms this triangle.
The triangular analysis (see Fig. 21.4 ) is helpful to assess the cants in the maxilla, mandible, and chin in relation to the cranial base as well as to each other. Also, by measuring and comparing the left and right sides of the bases of the triangles, transverse discrepancies and rotations can be assessed. Midline symmetry of ANS, Me, and the dental midlines can be evaluated. Asymmetrical discrepancies between the lower dental midline and the midpoint of the chin should be noted. With the dental and chin midlines coinciding, however, both are asymmetrical to facial and upper dental midlines, and symmetry should be corrected with mandibular surgery. With upper and lower dental midlines centralized, however, the chin is asymmetrical, and correction will require genioplasty. It is important that the orthodontist position the lower dental midline in the middle of the chin.
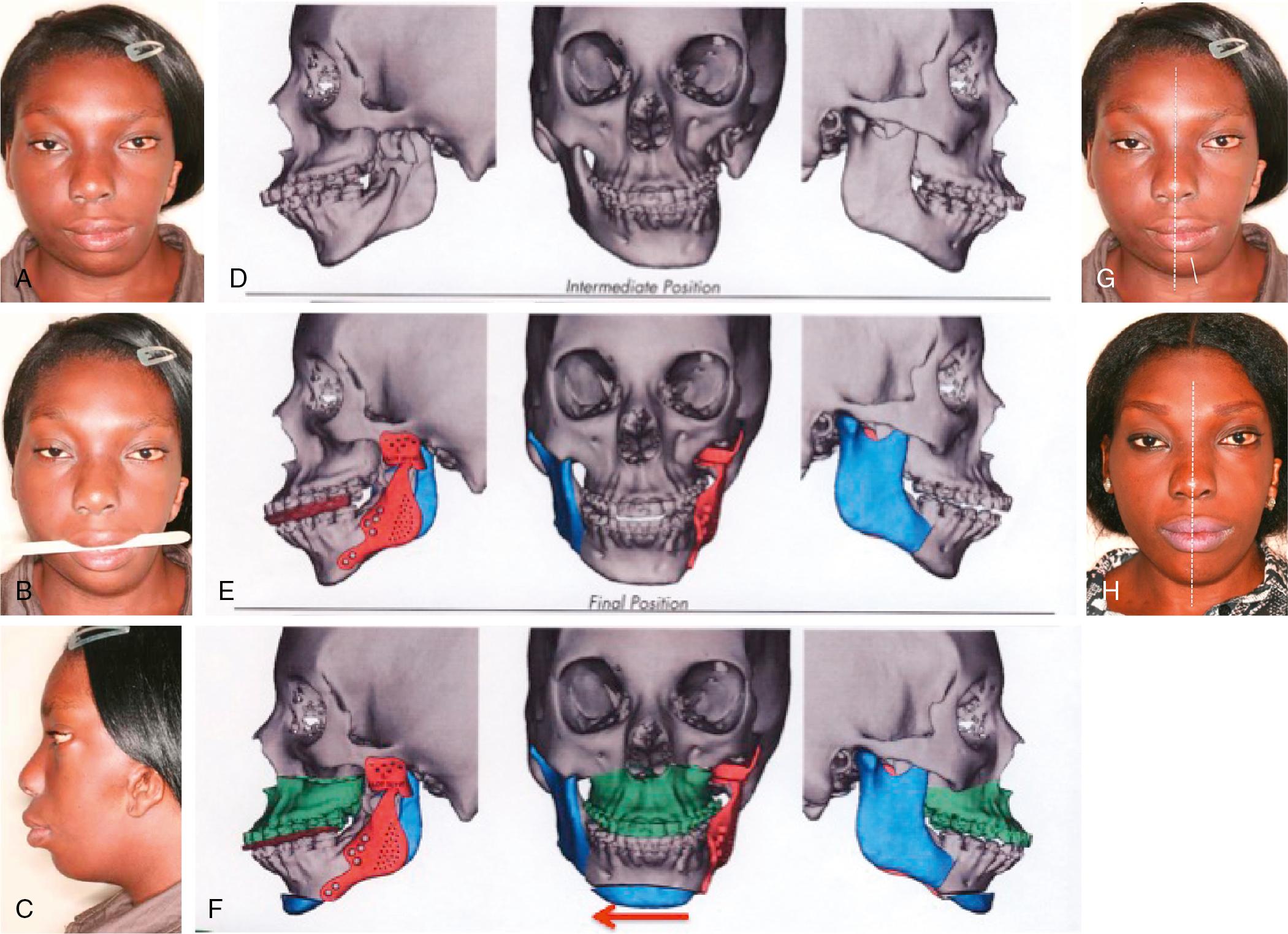
The posteroanterior cephalometric analysis is, however, limited to the evaluation of only two dimensions of the face. The value of 3D digital computerized studies in the assessment and treatment planning of facial asymmetry is demonstrated in case 1 ( Fig. 21.5 ).
Clinical examination and analysis of the dental models provide the most information regarding occlusion and other dental factors required for diagnosis and treatment planning. Several basic clinical and dental model evaluations, in combination with the cephalometric assessment, are helpful to develop an orthodontic and surgical treatment plan. Only the essential dental evaluations for mandibular skeletal surgery will be discussed here.
Arch length and tooth sizes: The mesiodistal widths of teeth, relative to the amount of alveolar bone length available, can be correlated and the presence of crowding or spacing assessed. This will assist in determining whether teeth need to be extracted or spaces need to be created or closed. Generally, in class II malocclusion, crowding will be present in the lower arch and less in the upper arch, and the lower incisors will often be proclined. In class III malocclusion, the lower incisors will often be lingually inclined, compensating for the class III skeletal relationship between the maxilla and the mandible.
Tooth size analysis: The Bolton analysis is a method used to correlate the mesiodistal widths of the six upper and lower anterior teeth. The formula is: Total width of the lower anterior six teeth × 1.3. The total mesiodistal width of the upper six incisors divided by the combined width of the six lower incisors yields a value called the intermaxillary (Bolton) index. This number should equal the total width of the six anterior teeth in the upper arch. The difference between the calculated and the actual upper arch widths determines the tooth size discrepancy (TSD). TSD causes incompatibility of dental alignment and may occur in the anterior teeth and in the premolar and molar regions.
Incisor angulation: This refers to the axial inclination of the incisors in relation to their respective basal bones. The key is to remove dental compensations by repositioning the incisors in the central trough of bone. In class II mandibular deficiency, the incisors would tend to be protrusive and will often need to be decompensated by retraction. The incisors in class III mandibular prognathia will mostly be retroclined and often need to be decompensated by proclination.
Curve of Spee: This relates the vertical position of the lower incisor teeth to that of the posterior teeth. The lower incisors should be 1 mm above a flat mandibular occlusal plane. An accentuated curve of Spee in the mandible is often associated with a deep bite and a reverse curve with an anterior open bite. If an accentuated curve of Spee in the mandible is present, the clinician needs to consider whether the curve should be corrected orthodontically before or after surgery. Orthodontic leveling will increase the arch length and may require tooth extractions. A severe curve of Spee can also be corrected surgically and may eliminate the need for extractions.
Intercuspid relations: This refers to the Angle classification of dental relationship. A class I canine intercuspid relationship is essential. A class I molar relationship is preferable, but a class II or III is acceptable and will occur due to premolar extraction in one dental arch and not the other.
Dental arch symmetry: There may be significant asymmetry within the arch, and this may often occur with a unilateral missing tooth. Vertical asymmetry may occur in sections or even an entire dental arch, causing a cant in the transverse occlusal plane. These vertical dental asymmetries and occlusal cants will have consequences with skeletal correction and will need consideration.
General dental problems: Problems such as missing teeth, caries, crowns, bridges, implants, impacted teeth, ankylosed teeth, and large dental restorations may influence the treatment design and should be identified before treatment. Root resorption of teeth should be noted because it will influence the planned orthodontic treatment. The salvageability of teeth and the decision to extract or restore a tooth forms an integral component in planning and treatment of patients. If a tooth extraction is planned, it should be decided either to maintain the space and replace the tooth with an implant later or to close the space orthodontically or surgically.
Periodontal status: Lack of sufficient keratinized epithelium, especially in the lower incisor region, and preexisting periodontal pathologies could be worsened by orthodontic and surgical treatment. This should be addressed before commencement of treatment because if left untreated, severe gingival recession and loss of supporting bone will result. It is especially important when the lower incisors are proclined (i.e., dental decompensation) in class III cases. Gingival grafting must be considered to provide attached keratinized epithelium attachment before the start of orthodontic treatment.
Macroglossia: True macroglossia may be caused by congenital conditions, such as Down syndrome, Beckwith-Weidemann syndrome, lymphangioma, glandular hyperplasia, and hemangioma. Acquired causes of macroglossia may include acromegaly, cysts or tumors of the tongue, myxedema, and amyloidosis. It is important to differentiate between true and pseudomacroglossia. With pseudomacroglossia, the tongue size may be normal; however, the tongue will appear relatively large. Habitual posturing, hypertrophied tonsils or adenoid tissues, small dental arches, and tumors displacing the tongue may create the impression of pseudomacroglossia. An enlarged tongue may cause several dentoskeletal problems and certainly cause skeletal and dental instability following surgical orthodontic treatment. However, not all open bite dentofacial deformities are caused by macroglossia; surgical orthodontic correction of an open bite without addressing a large tongue would certainly lead to poor stability. In the presence of macroglossia, a tongue reduction procedure should be considered before commencement of treatment. Orthognathic correction of an open bite malocclusion will allow a normal tongue to adapt to the altered volume of the oral cavity and will also eliminate the cause of a tongue thrust.
Temporomandibular joint (TMJ) assessment: The TMJ is an important component of the orthognathic mechanism and should be carefully examined. A basic TMJ evaluation should be done in two areas: (1) mandibular movements (limited or asymmetrical mouth opening); and (2) TMJ signs and symptoms (pain, clicking, locking). The pretreatment status should be carefully documented as pathologic conditions of the joint may be present at the outset, develop during treatment, or even develop long after treatment.
The genioplasty procedure can be performed as a single surgical procedure; however, to optimize aesthetic results, the procedure is often performed in conjunction with other orthognathic surgical procedures.
The required soft tissue result can be predicted either with the aid of digital 3D computer programs or by using the lateral cephalometric radiograph. The advantage of the computer-aided prediction is that a 3D image can be visualized. The visual treatment objective is developed with all the data obtained from systematic patient evaluation to make the visual objective as accurate and realistic as possible. The ratio of soft tissue changes to hard tissue changes associated with surgical advancement of the chin is 0.9 to 1.0 and for chin reduction is 0.6 to 1.0. The surgical cephalometric visual treatment objective is well demonstrated in the clinical cases presented. The soft tissue response is influenced by the surgical technique and design.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here