Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Many venomous animals can cause injuries to humans. The injuries are induced by substances called toxins that are produced or stored in the body of these animals and inoculated (i.e., injected) into victims by their venom apparatus, as seen in snakes, spiders, and scorpions. Toxins can also cause lesions from contact when the animal is handled or crushed, as happens with some species of beetles. , , In this situation, they are called poisonous animals, as they do not cause active envenomation.
Toxins can interact and cause lesions in the tissues, organs, and systems of other animals. The mixture of toxins in a venomous animal represents its venom, and venomous animals use the toxins or venom as a defense against predators and to obtain food. The effects are variable, but mainly the blood, nervous system, and tissue at the inoculation site are affected (e.g., hemolytic, neurotoxic, and necrotic effects). Some envenomations cause minimal local manifestations because of their mainly neurotoxic and hemolytic actions. However, coagulant/anticoagulant and proteolytic venom fractions can cause severe necrosis, which facilitates significant secondary bacterial infection. Such lesions can be classified into two types according to the depth of action: (1) Surface (or cutaneous) lesions are the result of contact with irritating substances from certain invertebrate species, whereas (2) inoculation lesions occur when venom is injected deep into the dermis and subcutaneous tissue, causing variable degrees of skin necrosis. Some necroses are superficial, as with cnidarians (jellyfish), whereas others are deep and severe, as caused by snakes and some spiders.
Many conditions can lead to human envenomation in the extremities, especially in the lower and upper limbs. One profile for bites by snakes includes farmers working outside without foot or leg protection. Envenomation often occurs in the hands because of their exploratory function, especially in children. Adult hand injuries occur mainly in farmers and fishers as a result of the characteristics of their work. Academically, hand envenomation can also be characterized according to animal groups, but the groups will always possess venom with coagulant and proteolytic actions that cause superficial or deep tissue necrosis.
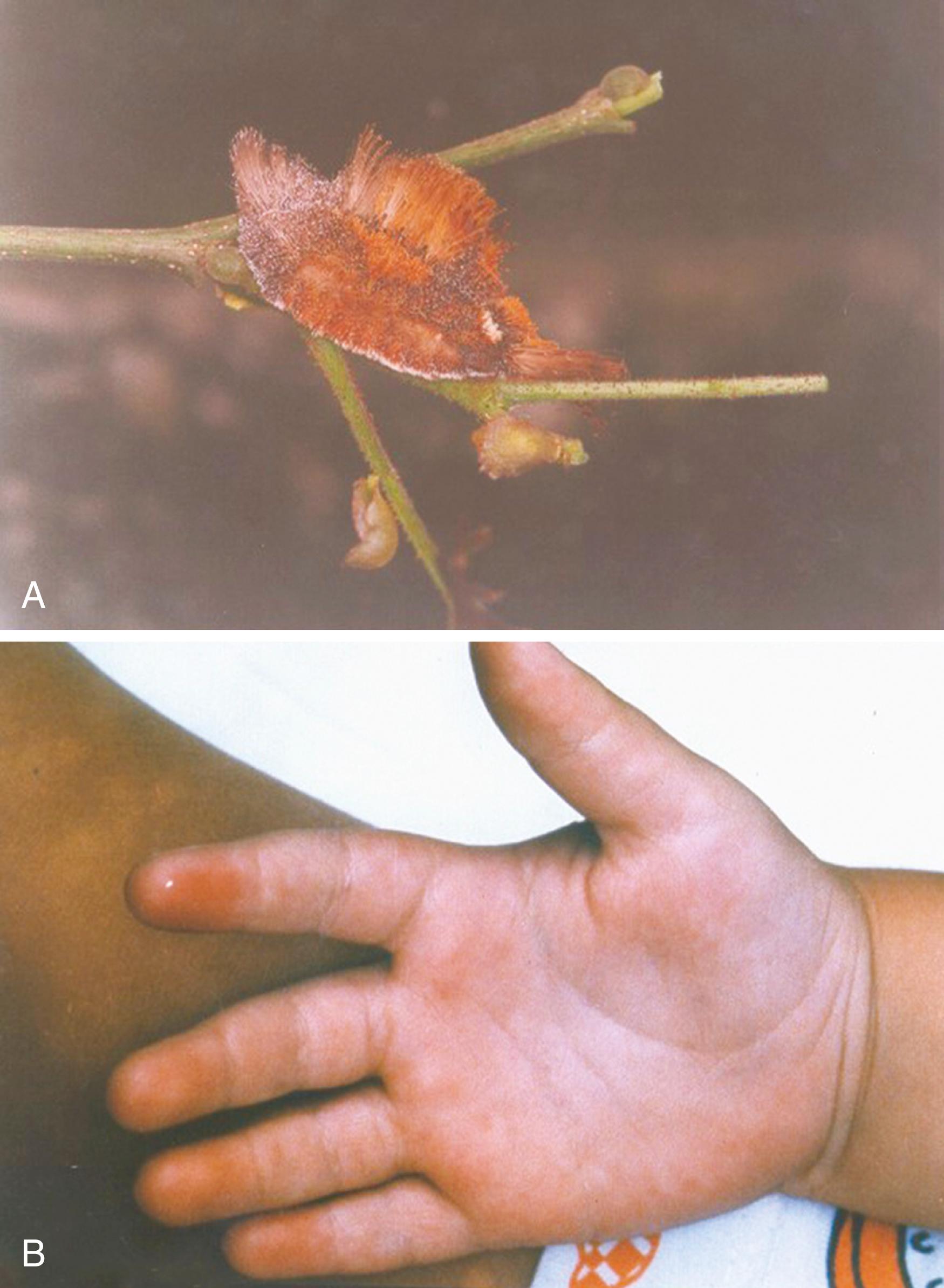
Envenomation by caterpillars is the most common of all injuries by venomous animals around the world. Caterpillars of the Saturniidae and Megalopygidae families cause the majority of injuries, and their hollow bristles contain toxins capable of provoking intense pain and a mild inflammatory reaction at the point of contact ( Fig. 52.1 ). , , , As a rule, the pain is out of proportion to the mild erythema and edema observed. Occasionally, local superficial necrosis occurs. The injury can be treated by a regional anesthetic block to control the pain or serial application of topical anesthesia with 0.25% lidocaine and 0.25% prilocaine in order to greatly decrease or eliminate the pain. There are no later sequelae as a result of this type of envenomation.
Most spider bites cause minimal local and systemic effects in humans, with variable pain intensity and healing without sequelae; the only treatment necessary for these injuries is analgesia and hygienic measures at the bite site. Spider bites that cause systemic complications and risk to life, such as in bites by Latrodectus (the black widow), Atrax (the funnel web spider), and Phoneutria (the banana spider), do not cause significant manifestations at the bite site. A spider associated with severe local effects, including marked tissue necrosis, is the cosmopolitan brown “recluse” spider (genus Loxosceles ) that lives in some regions of Africa; the North, Central, and South Americas; Australia; and some places in Asia and Europe. , Loxosceles spiders often live in home environments, mainly in dark places, and can bite when crushed against a victim’s body, usually at night in situations where the spiders feel threatened. The incidence of arm and hand spider bites is about 15% to 30%, and they can cause severe functional problems and long periods of incapacity; these are important injuries that specialists in upper extremity surgery should become familiar with. ,
Brown recluse spider venom is a mix of proteins. The most important fraction is sphingomyelinase D, which causes skin necrosis, vasculitis, and hemolysis. , , , There are two classic manifestations: cutaneous loxoscelism and viscerocutaneous loxoscelism. The initial bite may be minimally painful and go unnoticed. In 2 to 6 hours, a burning pain arises along with local erythema and blanching of the skin with eventual cyanosis and edema. Occasionally, hemorrhagic blisters develop. In 3 to 7 days, necrosis is evident ( Fig. 52.2 ). , , , If skin lesions are absent after 2 to 3 days, soft tissue necrosis is unlikely. , Systemic alterations, if they occur, will be present within 24 to 72 hours after the bite and include fever, arthralgias, vomiting, hemolysis, petechiae, and urticaria, with disseminated intravascular coagulation and renal failure being at the severe end of the spectrum. , , , ,

The gold standard for diagnosis is capture and identification of the spider, a situation that rarely occurs and unfortunately leaves clinical diagnosis, based on the dermatologic aspect of the lesion, as the most important method. , , , The knowledge of the geographic distribution of spiders of the Loxosceles genus and the seasonality of the envenomations contribute to the diagnosis. We must remember that the clinical appearance of the necrotic injury in the skin is not specific to the bite of spiders and may be caused by several medical conditions, such as erysipelas, cellulitis, necrotizing fasciitis, and fungal and bacterial infections, as well as other animal envenomations. , , Serologic diagnosis is currently in the experimental stage. , , ,
There is no standard treatment for spider bites. , , Skin integrity should be maintained to prevent infection and local circulation preserved, specifically with hand lesions, to maintain articular mobility and skin sensitivity. The initial phases of treatment should include rest, cold packs, elevation of the limb, intensive cleaning, tetanus prophylaxis, systemic analgesics, and gentle passive and active articular mobilization. , Moderate or severe bites (with significant necrosis) are treated with antibiotics (e.g., dapsone), corticosteroids, surgical excision, and antivenin. , , , , Dapsone is an antibiotic from the sulfone group with antimicrobial and antiinflammatory properties; it is commonly used for leprosy and many inflammatory skin diseases. , Use of dapsone is based on its capacity to block the diapedesis of neutrophils. Dapsone is used in later phases (48 hours after envenomation) and the recommended dose is 100 to 300 mg/day. The greatest concern with the use of dapsone is the advancing effect of hemolysis, which can be severe and cause methemoglobinemia in patients with glucose-6-phosphatate-dehydrogenase deficiency, requiring strict biochemical and hematologic control before and after the use of dapsone. There are no conclusive studies of the efficacy of dapsone or corticosteroids for spider bites, however. , , , , Antibiotics are only used in the presence of secondary infection of necrotic lesions.
Antivenin is routinely used in Brazil, and studies have shown that it can prevent necrosis when used in the first 12 hours after envenomation. , , Unfortunately, this medication is not presently available in the United States. Surgical treatment includes debridement and excision of necrotic tissue and coverage with grafts or flaps once viable tissue is reached. The question involves the time to initiate intervention because necrosis can be active for up to 2 to 8 weeks after the bite. Rees and coauthors reported that late surgery gave better results in their study series. Clinical experience indicates that management consisting of debridement, hygiene measures, and waiting for stabilization of the tissue necrosis is prudent initial treatment. , , , , ,
The most important envenomations by snakes are from the Elapidae and Viperidae families. Bites by the Elapidae family cause discrete skin manifestations, mainly as a result of their neurotoxic and myolytic effects. The snakes include the African and Asian cobras, the African green and black mambas, the American coral snake and the Australian Elapidae snakes, the taipans, and brown snakes. Envenomation can be very severe, and patients sustaining significant envenomation should be identified early. The typical facial symptom is called “drunken face” because of eyelid ptosis, and this should not be confused with other situations such as myasthenia gravis or alcoholic intoxication. Muscular paralysis is the main clinical effect of the bites.
Envenomation by the Viperidae induces necrosis of the skin and deep structures. Snakes in this family are found around the world; the most common associated with human bites are the European and Asiatic vipers and the African vipers such as the Gaboon viper (Bitis gabonica) , the puff adder (Bitis arietans) , and the saw-scaled viper (Echis carinatus) . In the New World, necrotic and inflammatory lesions can be associated with Lachesis (bushmasters) and Agkistrodon (the North American cottonmouth and copperhead), but mainly with snakes of the Crotalus (rattlesnakes) and Bothrops genera, which are very common in North, Central, and South America ( Fig. 52.3 ). The venom of all these snakes can induce intense inflammation, edema, and necrosis at the bite site ( Fig. 52.4 ). , , ,


The intensity of the necrosis caused by envenomation is variable and modulated by the capacity of the venom fractions to destroy tissue. Bites inoculate venom into subcutaneous tissue or muscle, and bite marks may be invisible. Edema at the site of injury occurs very early and can be extremely intense; pain is proportional to the edema. When present, the coagulant and anticoagulant factors in venom cause local and systemic effects, and they can affect systemic coagulation and induce hemorrhage. Skin blisters are common ( Fig. 52.5 ).

Large areas of necrosis and inflammation can simulate erysipelas and cellulitis. These findings can also occur in the presence of a secondary bacterial infection, a common complication in envenomations that leads to extension of necrosis and ulcers at the bite site ( Fig. 52.6 ). Abscess formation can be seen at the bite site as well, and it is usually caused by gram-negative and anaerobic bacilli. Occasionally, amputation of the compromised extremity is necessary because of necrosis and infection. This is common in fingers and is due to the compromise of their circulation, and the necrosis can extend proximally to muscles, tendons, and bones ( Fig. 52.7 ). ,


A rare but very severe complication is compartment syndrome, which is an increase in pressure in a closed compartment that results in abnormal neuromuscular function because of compression of muscles, nerves, and vessels. This syndrome is a result of necrosis and inflammation and is most commonly found in the volar and dorsal forearm, legs, and fingers. The most valuable signs and symptoms to help in the diagnosis of compartment syndrome is pain that is not proportional to the edema and limitations in neuromuscular action. The gold standard in the United States for evaluation of this syndrome is measurement of compartment pressure. Systemic hypotension may be present in patients with normal peripheral pulses. Treatment of compartment syndrome consists of fasciotomy, which is more effective when performed early.
Antivenin (specific for various genera) is the only worthwhile treatment, but it has little effect on local complications. Ince and Gundeslioglu reported the use of peripheral vasodilator drugs (pentoxifylline and dextran), associated with antivenom serum in finger injuries, with only 4% of cases developing some tissue necrosis. Due to possible adverse effects of treatment with the antivenom, mainly allergic reactions, patients treated with antivenin should be admitted to the hospital for strict clinical monitoring.
The primary antivenin used in the United States today is CroFab®, a sheep-derived antivenin that was approved for use by the U.S. Food and Drug Administration in October 2000 and is marketed by Savage Laboratories. It consists of purified Fab immunoglobulin fragments obtained from sheep immunized with the venom of the western diamondback, eastern diamondback, and Mojave rattlesnakes and the cottonmouth or water moccasin. CroFab is given in the case of severe envenomations, with significant local tissue swelling, systemic signs of envenomation, and abnormalities in clotting functions. The initial dose is four to six vials of the antivenin mixed in 250 cc of saline and given slowly (25 to 50 cc/hour) over the first 10 minutes with monitoring for signs of allergic reaction. If none occurs, the remainder of the solution is given over the next hour. Depending on the response, redosing may be necessary.
Pit viper bites differ from other compartment syndromes in that the venom is injected directly into the skin and subcutaneous tissue with immediate resultant tissue edema, ecchymosis, and rapid swelling. The venom may or may not be injected into a closed compartment, but it usually is. The severe swelling of the skin and soft tissues outside a compartment can be of such a degree that the circulation will be impaired, particularly with bites on the digits of the hand. When a snakebite victim in whom the tissues of the envenomated extremity have the appearance of an impaired blood supply or compartment syndrome, or both, is first seen, the patient is prepared for surgery. This is regardless of whether antivenin was or is being administered; however, surgery is started only after blood coagulation studies have been completed.
The skin and subcutaneous swelling can be so great that the blood supply is impaired, which may result in subsequent tissue loss. If such swelling is noted, fasciotomy of the underlying compartment as described earlier is done at the same time, without measuring compartment pressures. If the swelling is severe enough to necessitate a dermotomy, the fascia has been penetrated and intracompartmental swelling is present. Failure to release skin that is too tight and is compromising local blood flow can lead to significant tissue loss in the hand, which may necessitate later reconstruction. Local tissue necrosis at the site of the fang marks is debrided, but no other debridement is done at this time.
If after a snakebite no clinical evidence of impending tissue loss secondary to severe swelling exists and there is no clinical evidence of a compartment syndrome, no surgery is performed. As emphasized previously, the pain and degree of swelling after a pit viper bite can make the clinical diagnosis of compartment syndrome a difficult one and may necessitate continuous intracompartmental pressure monitoring. The guidelines for decompression of the soft tissues outside a compartment are nebulous and based on past experience; however, the question of whether a closed compartment needs to be opened should be settled by measuring compartment pressure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here