Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The global burden of disease related to trauma is immense, with more than 1.5 million deaths each year due to violence, 1.25 million deaths in road traffic accidents annually, and nearly 1 million children die each year because of injury. These numbers are expected to increase in the next 20 years and trauma is among the top 10 causes of death globally. The numbers of injured survivors have increased, with up to 1 billion patients seeking medical assistance after an injury annually, and depending on the geographical location every eighth hospital admission now is related to injury. The associated global costs are excessive approaching 2% of a country’s gross national product with respect to road accidents ; however, it must be emphasised that there are considerable variations between different countries.
The trimodal death distribution, first described by Trunkey in 1983, may have changed in the past years, but it remains a good model to understand the timing and causes of death following injury. , The first peak relates to patients with non-survivable injuries (e.g. complete aortic rupture). Despite preventive measures (e.g. seat-belts, airbags, helmets, avoiding drunk-driving), which remarkably reduces the first peak and the years of life lost, injuries continue to cause death and morbidity. The majority of patients die within the first 24 hours after an accident, and this second peak comprises patients arriving alive in the emergency department, with head, thoracic and abdominal/pelvic injuries being the predominant lethal injuries. Unrecognised or untreated abdominal injury is one of the most important causes of preventable death. One of the main goals of trauma surgery is to diminish this peak and Advanced Trauma Life Support (ATLS®) with its primary and secondary survey is one way to evaluate and treat severely injured patients in this phase. The third peak comprises patients dying at a later stage due to multiorgan failure and sepsis.
![]() The Advanced Trauma Life Support (ATLS®) guidelines are a crucial part of the early evaluation and management of all trauma patients.
The Advanced Trauma Life Support (ATLS®) guidelines are a crucial part of the early evaluation and management of all trauma patients.
Trauma surgery has evolved tremendously over the past 50 years. The traditional dogma of mandatory exploration of all penetrating wounds has changed to selective non-operative management (NOM) in neck and abdominal trauma. Damage control surgery and damage control resuscitation have been introduced. Abdominal compartment syndrome and intra-abdominal hypertension have been identified and strategies put in place for prevention. Early institution of blood and lower volumes of crystalloids are seemingly beneficial. There is a far better understanding of coagulopathy in the trauma setting and specific transfusions ratios have been shown to improve survival. A more restrictive transfusion regime is also associated with less infection. Imaging is far more frequently available and the introduction of focused assessment with sonography in trauma (FAST) and extended FAST (eFAST) in the resuscitation room is changing surgical algorithms. There is much to be enthusiastic about in our management of the injured patient, but we also need to be aware of the fact that clinical signs are vital in our assessment and that there should not be an over-reliance on special investigations.
The goal of the primary survey is to identify and instantaneously treat life-threatening injuries. This early management phase is called the ‘golden hour’. Pre-hospital and in-hospital time plays an important role in this resuscitation phase as the mortality is highest within the first 24 hours after the incident. Patients are assessed and resuscitated along the ATLS ABCDE algorithm. The following life-threatening injuries must be ruled out:
A irway: airway obstruction (due to foreign bodies, aspiration, facial or laryngeal injuries)
B reathing: tension pneumothorax, open pneumothorax with a sucking wound, massive haemothorax, cardiac tamponade, flail chest
C irculation: shock (mainly caused by haemorrhage)
D isability: severe traumatic brain injury
E xposure: hypothermia
The pathophysiological consequences of these injuries are hypoxia (caused by airway or breathing problems), hypotension/ hypoperfusion (caused by circulation problems) and hypothermia (exposure problem). Hypoxia and hypoperfusion result in anaerobic metabolism with accumulation of acidic metabolites, a deficiency of adenosine triphosphate (ATP) and failure of the Na/K-ATPase pump. This failure causes cell swelling and damage, and finally organ dysfunction. Serum lactate, pH and base excess are good parameters to assess the adequacy of organ perfusion and oxygenation. Higher lactate level and the duration of hyperlactatemia correlate with mortality after trauma. Hypoperfusion also leads to increased excretion of stress hormones, which consecutively increases the contractility of the heart, the heart rate as an early sign of relevant blood loos and local vasoconstriction with hypoperfusion of the skin, muscles, kidneys and the intestine (centralisation). Blood pressure drops later with ongoing blood loss and exhausted compensatory mechanisms. Heat loss while lying exposed, cold intravenous fluids and opened body cavities during surgery cause hypothermia. Hypothermia itself negatively influences the coagulation system and myocardial function. The three ‘hypo’-problems lead to the well-known deadly triad of hypothermia, acidosis and coagulopathy .
The treatment in this primary phase is priority-oriented and kept as simple as possible.
All patients are given supplemental oxygen. A definitive airway (intubation or surgical cricothyroidotomy) will clear any airway obstruction. Needle decompression and intercostal drains usually resolve any life-threatening tension or open pneumothoraces. A thoracotomy is required for a massive haemothorax (>1500 mL drainage) or for ongoing bleeding (>200 mL/h for the next 4 hours), patients in profound refractory shock or undergoing cardiopulmonary resuscitation after penetrating trauma. The main goal in circulation problems is to stop the bleeding and restore the volume. Chest (e.g. intercostal arteries), abdomen (mainly spleen, liver, mesentery or kidneys), pelvis or long bones (fractures) and external wounds (with vascular injuries, extensive scalp or torso injuries) are the main sources. Intercostal drains, direct compression, packing, or (partial) resection of bleeding organs, aortic cross-clamping, Pringle manoeuvre, vessel repair or shunting are some basic techniques to stop the bleeding. Unstable pelvic fractures are temporarily stabilised by a pelvic binder, C-clamp or external fixator. Long bone fractures are externally or internally stabilised to reduce bleeding, alleviate pain and enable intensive care. A damage control resuscitation in patients with major haemorrhage can improve outcome: minimised, balanced, volume resuscitation, especially in penetrating injuries, until early successful bleeding control, but an adequate volume substitution and pharmacologic adjuncts (tranexamic acid) have then to be carried out and adequate urine excretion has to be achieved. , Using the Glasgow Coma Scale (GCS), a patient with a score less than 9 must be intubated and evaluated with a computed tomography (CT) scan of the brain. The CT of the brain should be delayed in the case of a patient who is haemodynamically unstable requiring operative intervention. Warm infusions, blankets or warming devices such as a Bair Hugger 3 M© are used to limit and treat hypothermia.
Further relevant injuries can now be sought and treated in the next phase, the ‘secondary survey’, usually carried out from head to toe. Basically, definitive repair of all relevant injuries is the main target. However, the extent of these therapeutic measures as well as the surgical procedures in the primary survey must be considered. Trauma causes a first hit and a consecutive systemic inflammatory response syndrome (SIRS), which can trigger reduced resistance to infection. Early extensive surgical care of all injuries, acting as a second hit, can lead to a further immune response with resultant multiorgan dysfunction, failure or even death. In addition, if certain criteria are met (e.g., hypotension on admission, abdominal vascular and major liver injuries), only abbreviated operative procedures, so-called damage control surgery , should be applied. Damage control surgery is a well-established surgical strategy, mainly in major abdominal trauma, but also in other conditions, and should enable patients not to slip further into an unsalvageable metabolic state of the deadly triad of hypothermia, acidosis and coagulopathy. Damage control surgery aims to quickly stop the bleeding and limit contamination without restoration of the anatomy (e.g. to pack or remove solid organs, staple bowel injuries and to temporarily close the abdomen), and to normalise the pathophysiological parameters in the intensive care unit (ICU). No major surgery is carried out during this ICU stage. Oxygen delivery, blood pressure, heart rate, urinary output, body temperature, pH, lactate and coagulation must be normalised in the ICU. Aggressive volume resuscitation, abdominal packing and the accumulation of intra-abdominal blood increase the risk of an abdominal compartment syndrome in some of these patients and the intra-abdominal pressure should therefore be monitored (IAP > 20 mmHg with new organ dysfunction). Reduction in cardiac output, renal failure, impaired ventilation and raised intracranial pressure are several pathophysiological consequences of raised intra-abdominal pressure (see Chapter 20 ). After normalisation of these parameters, a re-look is performed with definitive surgical care and primary abdominal wall closure without mesh if possible. The timing here is crucial; the possible consequences are re-bleeding if returned too early, and infection and sepsis if returned too late to the theatre to remove abdominal packing. Patients ideally remain intubated, ventilated, under antibiotic cover and return to theatre 24–48 hours after the first operation.
The following pathophysiological parameters, signs and criteria are indicators to proceed with damage control surgery: ,
Hypothermia < 35°C
Acidosis pH < 7.2
Lactate > 5mmol/L
Coagulopathy INR > 1.5
Systolic blood pressure < 90 mmHg
Mass transfusion (10 and more blood units)
Trauma mechanism (e.g. multiple torso gunshot wounds [GSWs])
Injury Severity Score (ISS) > 36 points
Major vascular (e.g. inferior vena cava injury) and visceral or pelvic injuries
Higher age and comorbidities
Inability to control bleeding by conventional methods
Inability to close the abdomen
Abdominal compartment syndrome during attempted abdominal wall closure
Need to reassess extent of bowel viability
Depending on the hospital facilities, some care cannot be provided locally and the patients must be transferred as soon as possible to a trauma centre or another suitable facility. Typical injuries warranting a transfer are:
Severe or moderate head injury
Major pulmonary contusions
Flail chest
Cardiac or great vessel injury
Acute spinal cord injury
Solid organ injuries
Unstable pelvic ring injury
Severe open fractures or amputations
Several long bone fractures
Polytraumatised patients
Severe burns
Older patients (>55 years) or patients with comorbidities
Patients with these injuries are ideally treated in a level I trauma centre which has been associated with better outcomes and improved survival.
Injury scoring scales
The American Association for the Surgery of Trauma (AAST) publishes the most widely accepted and used injury classification system for neck, chest and abdominal injuries, which is available online at http://www.aast.org/Library/TraumaTools/InjuryScoringScales.aspx . Organ injuries are graded into five increasing severity categories, grade I being minor haematomas or lacerations and grade V completely shattered or devascularised organ injuries.
![]() These injury severity scores are important as they help to guide treatment, have a prognostic value and allow the comparison of results in the literature.
These injury severity scores are important as they help to guide treatment, have a prognostic value and allow the comparison of results in the literature.
Abdominal organs are less protected than those of the chest. General surgeons are consequently often confronted with intra-abdominal trauma. The timing of assessment and treatment depends on the haemodynamic status of the patient and the clinical evaluation. In the primary survey, a clinical evaluation of the haemodynamic status, the abdomen and a FAST is required, particularly in blunt trauma or suspected haemopericardium. Haemodynamic stability is defined as systolic blood pressure > 90 mmHg, pulse rate < 100/min and no more than 1–2 L of crystalloid infusion. Vital signs must be cautiously interpreted, especially in elderly patients, young patients and patients who are under the influence of certain medications and always be correlated with the injuries and metabolic response of the patient. A narrowed pulse pressure in normotensive patients can be a subtle warning sign of haemorrhage.
A thorough clinical evaluation is required in the secondary survey, with inspection, palpation, percussion and auscultation. Repeated examination is the key as physical signs may be delayed or altered in the case of drunk or drugged patients, patients with traumatic brain injuries, acute spinal cord injuries and with distracting injuries. Adjuncts (nasogastric tube, urinary catheter, FAST, CT of the abdomen, diagnostic laparoscopy [DL]) are helpful tools, particularly in these patients to rule in or out a relevant intra-abdominal injury.
The most important method in clinically evaluable patients remains serial clinical examination. In penetrating trauma, the authors do not recommend ultrasound of the abdomen or invasive procedures such as local wound exploration or diagnostic peritoneal lavage.
The further priority of assessment and treatment is dictated by the mechanism of injury, sustained injuries, haemodynamic status of the patient and clinical evaluation. Typical indications to proceed with a laparotomy are:
Haemodynamic instability due to an intra-abdominal injury (positive ultrasound or clinical evidence of intraperitoneal bleeding)
Peritonitis (tenderness of the abdomen and abdominal guarding)
Organ evisceration
GSWs with a transabdominal trajectory
Confirmed stomach, rectum or genitourinary system (bladder, ureter, vagina) injuries after penetrating trauma
Free intra-abdominal air
Hollow viscus rupture or perforation
Patient develops peritoneal signs or haemodynamic instability after failed NOM.
A few decades ago, all penetrating wounds mandated a laparotomy. More than 30% of the laparotomies were negative (no intra-abdominal injuries) or non-therapeutic (the intra-abdominal injury does not need any intervention). Short-term morbidity of a trauma laparotomy is high (wound infection, intra-abdominal abscess, pneumonia, urinary tract infection, deep venous thrombosis, pulmonary embolus) and long-term complications (small-bowel obstruction and incisional hernia) are encountered in 15% after trauma laparotomy. , This is independent of whether the laparotomy was therapeutic or unnecessary. To reduce unnecessary laparotomies and their consequences, selective NOM was developed in asymptomatic and haemodynamically normal patients. Lower transfusion requirements, fewer abdominal infections, shorter hospitalisation, lower mortality and lower costs are positive consequences of NOM. , The decision to proceed with NOM is crucial. The fear of re-bleeding, missing a hollow viscus injury and the consequences of a delayed laparotomy are still constant companions. The fear may be exaggerated since delayed laparotomies do not increase the risk of adverse events if carried out within 12–24 hours. Serial examinations are mandatory to detect failure of NOM and to act appropriately in a timely fashion, with risk factors for failed NOM being age older than 55, haemodynamic instability, higher specific organ and total injury severity grade, size of haemoperitoneum, contrast blush on CT and use of anticoagulants. Angioembolisation may play an important role in patients with these risk factors and solid organ injuries.
FAST is a non-invasive, cheap, easily reproducible, focused examination of the chest and abdomen, which can be performed at the bedside by the treating trauma surgeon. The primary goal of FAST is to detect free fluid (presumably blood in a trauma patient) in the abdomen, chest or the pericardium, as an explanation for the haemodynamic instability of a patient. The goal is not to detect distinct organ injuries. FAST can be carried out within 5 minutes, with the specificity to detect free fluid in blunt trauma being 90–100% and sensitivity 60–100%. , FAST, however, is operator-dependent, despite an easy learning curve. False-negative results are misleading and often seen in patients with obesity or surgical emphysema. The ultrasound can be falsely negative if it is performed too early, as it needs more than 500 mL of blood in Morrison’s pouch to be visible. , FAST performed too early is associated with more interventions. Ideal indications are blunt torso trauma, haemopericardium, children and pregnant patients. The goal of eFAST is to diagnose a pneumothorax, which can be done with a higher sensitivity than a chest X-ray.
Contrast-enhanced CT is the gold standard to detect and grade torso injuries in stable patients as well as to rule out significant injuries. Contrast blushes can also represent active bleeding spots, which are amenable to angiographic embolisation. It is non-invasive, but it usually requires transport to radiology, time and is expensive. Contrast material can cause allergic reactions and induce nephropathy. The overall accuracy and sensitivity is high except for diaphragmatic, bowel and some pancreatic injuries. A special algorithm is needed for diaphragmatic injuries (see later in this chapter). The index of suspicion of bowel injuries is high in the presence of:
free fluid and no solid-organ injury,
free extraluminal gas,
thickened bowel wall,
mesenteric stranding and
haematoma surrounding a hollow viscus.
Ideal indications for CT are stable patients with blunt trauma, penetrating back or flank trauma, penetrating trauma with questionable extraperitoneal tract, right upper quadrant/right-sided thoraco-abdominal trajectory (i.e. to exclude liver injury) and haematuria (i.e. to exclude upper urinary tract injury). In transpelvic penetrating wounds with haematuria, a CT cystogram is helpful to guide further treatment. , It is currently not clear if routine or selective scanning is recommended in polytraumatised patients, where there is a clear trend to a whole-body CT. ,
Laparoscopy is a minimally invasive procedure; however, it requires special expensive equipment, surgical skills and usually general anaesthesia. There is as yet no role for DL in the haemodynamically unstable patient, as pneumoperitoneum further compromises the haemodynamic, pulmonary and renal status. In elective trauma situations, it has been successfully used in diagnosis and repair of peritoneal breach, stomach, minor liver, suspected extraperitoneal rectal and, specifically, diaphragmatic injuries. It can help to avoid a laparotomy in a highly selected patient group. ,
The spleen (40–55%), liver (35–45%) and small bowel (5–10%) are the most frequently injured organs in blunt abdominal trauma. Major pelvic or chest injuries are commonly associated with relevant intra-abdominal injuries, and serial clinical examination usually detects these injuries. A seat belt sign or a buckle-handle injury raises the suspicion of a mesenteric, duodenal or pancreatic injury and such patients need admission and further investigations. NOM has become the standard of care in most patients with solid organ injuries with no indications to proceed with laparotomy (predominantly haemodynamic instability due to major haemorrhage). FAST or CT are most often used as adjuncts in NOM. Hollow viscus rupture and/or peritonitis are still clear indications to proceed with operative treatment. Free air or free intra-abdominal fluid without parenchymatous organ injuries must raise the suspicion of a hollow viscus or mesenteric injury and mandates a laparotomy, especially in patients with a severe head injury or complete spinal cord injury due to unreliable physical examination.
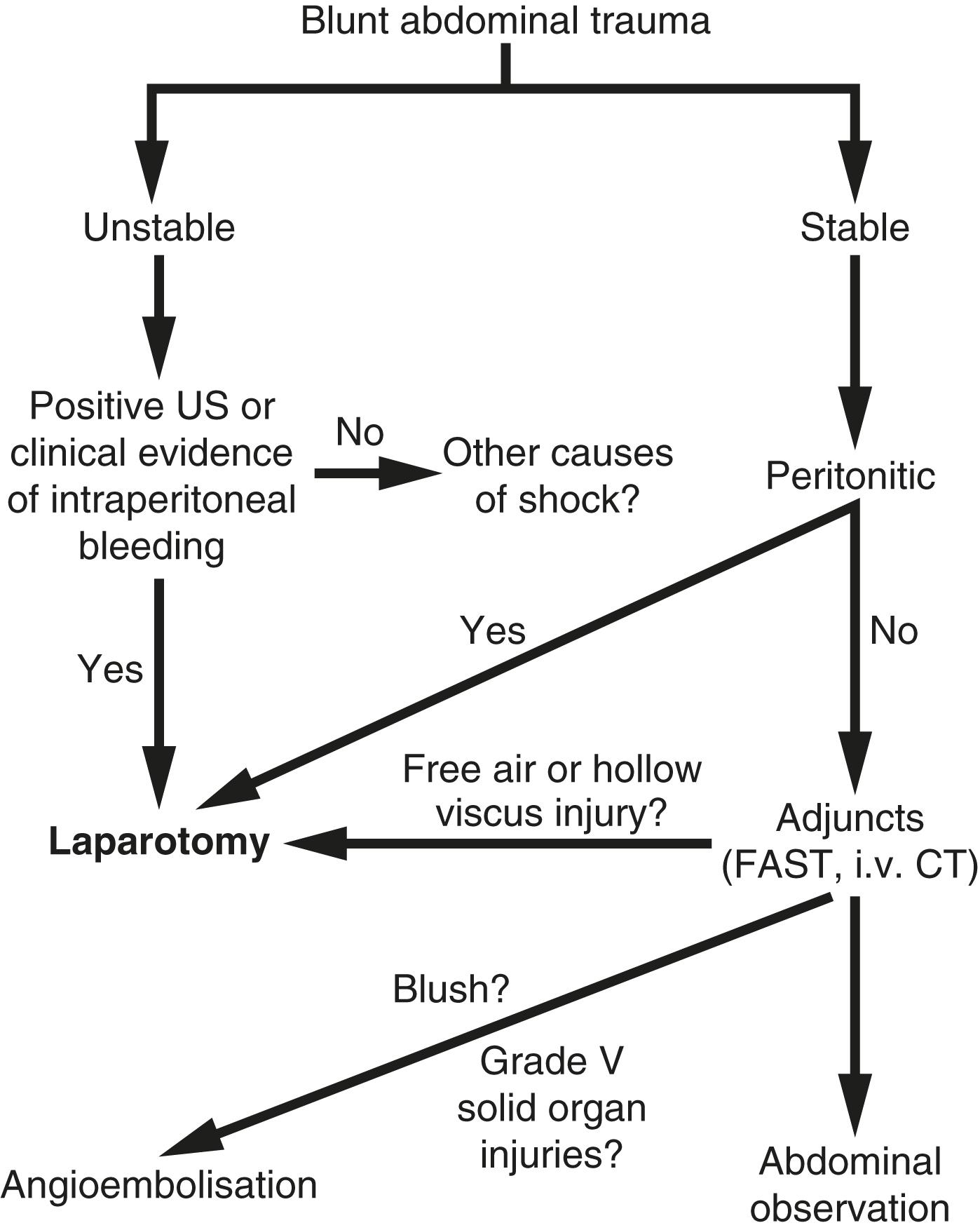
Fig. 19.1 presents an algorithm for the management of blunt abdominal trauma.
The spleen provides important immunological function by clearing intravascular antigens, hence infectious complications are feared after splenectomy. Demetriades et al. analysed 269 patients with blunt splenic trauma, one-third of whom underwent splenectomy. Wound infection, intra-abdominal abscess, urinary tract infection, pneumonia and septicaemia were complications encountered in 32% of the splenectomy group versus 5.2% in the splenic preservation group, with splenectomy raising the infection risk 10 times. Other relevant risk factors for infections were hypotension on admission, an ISS > 16 and hollow viscus injury. The recommendation is therefore to preserve the spleen if possible.
Splenic preservation, however, is not always feasible. Haemodynamic instability and a severely blunt injured spleen remain a clear indication to proceed with laparotomy and probable splenectomy. In a large retrospective case series of the most severe splenic injuries (AAST grade IV and V), 58% of all patients were initially managed non-operatively. NOM failed in 38%, mostly within 48 hours. Risk factors were grade V splenic injuries, concomitant brain injury and contrast extravasation on CT . Age (>55 years), anticoagulation drugs, cirrhosis and the need for blood transfusion must also be taken into account. Either surgery should be undertaken in these patients, or angioembolisation if patients are stable but have contrast extravasation. Prophylactic splenic arterial embolisation in patients at high risk for splenectomy (splenic pseudoaneurysm, splenic arteriovenous fistulas, AIS 3 and higher) was not superior to surveillance and embolisation as required in a randomised study. Interestingly, the use of anticoagulation (e.g. warfarin) did not affect the outcome of spleen (and liver) injuries. Patients after angioembolisation of the splenic artery also had higher rates of deep venous thrombosis. Angioembolisation may cause a reactive thrombocytosis and hence a higher risk of deep venous thrombosis. Early prophylaxis should be considered in these patients.
![]() Grade V splenic injuries, especially in combination with a head injury, predict failure of non-operative management.
Grade V splenic injuries, especially in combination with a head injury, predict failure of non-operative management.
Delayed haemorrhage, splenic artery pseudoaneurysm, splenic abscess or pseudocyst are complications after NOM. However, a 6-hourly serial physical examination and haemoglobin (Hb) estimation in a high-dependency unit (HDU) or ICU with bed rest for 1–2 days seems to be safe to avoid and detect these complications. Mechanical deep venous prophylaxis can be started immediately. Medical prophylaxis can be started after 48 hours without a higher risk of bleeding or NOM failure in isolated blunt splenic injury. Length of in-hospital observation remains unclear; however, 5–7 days or even less in isolated minor splenic injuries with unproblematic observation seems acceptable. Activities should be restricted for 6 weeks.
All patients after splenectomy should receive active pneumococcal and meningococcal vaccination within 2–3 weeks after the operation as well as seasonal flu vaccination. ,
Patient selection is crucial for NOM of blunt liver trauma. A large study at our institution analysed 134 patients with blunt liver injuries. One in four patients required urgent surgery due to haemodynamic instability (31%), peritonitis (46%) or CT findings mandating surgery other than the liver injury (23%). Systolic blood pressure < 90 mmHg at admission was present in more patients. However, hypotension on arrival was successfully treated in 70% with a fluid bolus of no more than 1–2 L of crystalloid transfusion. These patients did not need surgery for the liver injury. The remaining patients were non-responders and required surgery. Operative management comprising evacuation of haematoma and drainage only was needed in 37% of patients. Liver-related complications were encountered in 20% after surgery: necrosis, haemobilia and biliary fistula. NOM was initiated in three quarters of patients consisting of serial clinical examinations and Hb estimations in HDU or ICU, with no routine follow-up CTs. NOM was successful in 95%. Increasing abdominal pain and tenderness, spiking temperature, drop in blood pressure or a fall in Hb level were typical indicators of NOM failure. Liver-related complications were encountered in 7%: biloma, biliary peritonitis, liver haematoma and abdominal compartment syndrome. We concluded that NOM is safe, feasible and successful in selected patients. Patients for NOM must be stable, not peritonitic, and amenable for clinical evaluation . A CT scan with intravenous contrast should always be performed for patients managed by NOM.
Similar results were presented by Van der Wilden et al., who analysed 393 patients with AAST grade IV and V blunt liver injuries. One-third of the patients proceeded to surgery due to haemodynamic instability. The remaining two-thirds of patients were managed non-operatively, which was successful in 91%. Failure of NOM occurred due to recurrent liver bleeding or biliary peritonitis. We concluded that even high-grade liver injuries with haemoperitoneum and contrast extravasation can safely be treated non-operatively, which contrasts with high-grade splenic injuries. Importantly, nearly 70% of all NOM patients had a diffuse haemoperitoneum, 27% demonstrated contrast extravasation on CT and one quarter of all patients in their NOM group had angioembolisation of the liver.
Mechanical thromboprophylaxis, feeding and mobilisation should be started as early as possible in stable patients with NOM and no contraindications. , Medical thromboprophylaxis can be started after 48(–72) hours in grade 3–5 liver injuries. ,
![]() Most blunt liver injuries can be managed non-operatively in the stable patient.
Most blunt liver injuries can be managed non-operatively in the stable patient.
Low-grade blunt kidney injuries, such as kidney contusions, are successfully treated non-operatively. The evidence for higher-grade injuries is unclear. Haemodynamic instability and/or urine extravasation are indications to proceed with surgery, which generally means nephrectomy. A study that analysed 206 patients with AAST grade IV and V blunt kidney injuries demonstrated that one in four patients needed an urgent laparotomy due to haemodynamic instability. Nearly 60% of these patients underwent a nephrectomy. In three quarters of patients, NOM was started and successfully accomplished in 92%. Angioembolisation was undertaken in every sixth patient. Haemodynamic instability, peritonitis or abdominal compartment syndrome were the reasons for NOM failure. The authors concluded that even higher-grade blunt kidney injuries with urine extravasation in haemodynamically stable patients can safely be treated non-operatively.
In patients with gross haematuria and possible bladder injury, a CT cystography is recommended to rule out bladder injuries. Intraperitoneal bladder injuries must be repaired, while simple extraperitoneal injuries can be treated non-operatively with a urinary catheter in place for 10 days. However, if the anterior pelvic ring is approached, also an extraperitoneal injury should be repaired. Simple repairs in asymptomatic patients can be followed up clinically, all other injuries need a follow-up cystogram.
Penetrating wounds between the nipple line and the knees can potentially cause intra-abdominal injuries. The difficult questions to answer are: (1) has the peritoneum has been penetrated; and (2) an intra-abdominal injury requiring surgery has occurred. Penetrating wounds with solid organ injuries can still be managed non-operatively in many selected cases.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here