Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thoracic outlet syndrome (TOS) refers to a group of complex symptoms in the upper extremity caused by compression of the brachial plexus, the subclavian artery, and the subclavian vein between the interscalene triangle and the inferior border of the axilla. Although a treatable disorder, TOS often remains undiagnosed in patients complaining of diffuse numbness, chronic pain of the head and neck, and pain and weakness of the upper extremities. These patients live with discomfort, uncertainty, and disability, carrying the reputation of “malingerers.” Persistent symptoms may lead to devastating functional, emotional, and financial impairment. Loss of job and lifelong disability are potential outcomes of this syndrome if not treated successfully. Sixty-three percent of these patients are usually observed by general practitioners, and 37% are observed by consultants in other specialties. The first description of symptoms related to a supplementary cervical rib was reported by Willshire in 1860. In 1906, Murphy suggested that the anterior scalene muscle could produce these symptoms and, in 1956, Peet was the first to describe the term “thoracic outlet syndrome.”
Predisposing factors for TOS include (1) exaggerated and repetitive motion, (2) preexisting bone, muscle or tendinous anomaly, and (3) direct impact. The compression may be due to abnormal structures , such as a cervical rib or clavicular malunion or by otherwise normal structures , such as the first rib, the seventh cervical transverse processes, the anterior or middle scalene muscle, or the pectoralis minor tendon. A traumatic event is described as a precipitating factor in 21% of TOS patients. This condition is observed in baseball players such as pitchers, catchers, and first-basemen, and other athletes such as kayakers, weight lifters, and golfers, as well as volleyball, karate, lacrosse, and tennis players, who require exaggerated shoulder motion in their athletic activities. Other patients have a more insidious onset of symptoms caused by particular job-related routine tasks. A teacher may indicate that symptoms are brought on by writing on a blackboard. A cellist may attribute symptoms to holding the left arm in an abducted position. A painter may ascribe symptoms to working on a ceiling. Repetitive exertion of the shoulders, arms, and hands is required by auto mechanics, construction workers, and many other professionals who may be at risk to develop TOS given the nature of their work. Studies have linked upper extremity musculoskeletal disorders to high-performance musicians who play bowed string instruments. While reports about the prevalence of thoracic outlet syndrome in musicians varies, clinicians should be aware of TOS as a differential diagnosis when treating string instrumentalists with upper extremity musculoskeletal disorders. Exaggerated and repetitive motions can cause muscle hypertrophy and, as a result, subject the adjacent artery, vein, and brachial plexus to compression. Experienced clinicians have noted that individuals with long necks and sloping shoulders are prone to the development of TOS symptoms.
The reported incidence of TOS varies widely. The median age of patients suffering from TOS is 29 years. This syndrome has been described also in adolescence and in children , although this is rare. In people aged over 50 years, the syndrome is occasionally precipitated by an injury or lifting a heavy weight. TOS is more common in women. , Neurogenic TOS is reported as the most common form of TOS, comprising over 90% of all cases in adults. Venous TOS is more frequently reported in adolescents and children than in adults. ,
The complexity of multiple symptoms in the upper extremity is caused by (1) painful brachial plexus compression, (2) vascular compression, (3) denervation of hand intrinsic muscles, and/or (4) venous obstruction. Symptoms are more frequent in the dominant hand, although most of the cervical ribs are bilateral and slightly predominant on the left. ,
TOS is divided into the neurogenic type and the vascular type. Neurogenic TOS presents a complex of brachial plexus syndromes. Most patients exhibit symptoms of brachial plexus compression. The dominant symptoms are pain and paresthesias (88% and 83%, respectively) of the hand and forearm (especially ulnar nerve distribution). Most of these patients have bone anomalies at the base of the neck, such as a prominent C7 transverse process or rudimentary cervical rib and associated fibrous bands extending to the first thoracic rib that provoke compression of the lower brachial plexus (nerve roots C8–T1, lower trunk). Neurogenic TOS, with and without bone anomalies, can evoke pain in the distribution of the shoulder, neck, and radial aspect of the arm in the uncommon upper brachial plexus distribution (nerve roots C5 and C6), as well as chronic pain that does not follow a confined dermatomal pattern. Other symptoms include fatigability (23%) and brachial plexus tenderness (32%).
Nonspecific-type thoracic outlet syndrome, also referred to as a Disputed TOS is a category that embraces a multiplicity of vague organic and functional disorders of the upper limb, for which no other diagnosis has been reached. Symptomatology can be quite variable but often involves chronic pain that may or may not follow a confined dermatomal pattern. The diagnosis relies on positive clinical signs and symptoms with or without radiologic or electrophysiologic signs. Exclusion of alternative diagnoses and proper patient selection is the key to diagnosis of disputed TOS.
Vascular TOS is characterized by subclavian artery and vein complications, accounting for 1% to 10% of all patients with TOS, , and may result in significant long-term disability. The majority of arterial cases of TOS are associated with the presence of a cervical rib, which may be incomplete or rudimentary, or an abnormal first rib. , The arterial type of TOS may present symptoms of thromboembolism, lead to symptoms such as arm claudication or threaten arm viability. Occlusion of the subclavian artery also may be asymptomatic due to the rich collateral network. Subclavian artery pathology due to compression at the thoracic outlet is sometimes found to be the cause of an incidentally discovered, asymptomatic subclavicular bruit.
Subclavian vein compression occurs in the costoclavicular space and may be caused also by an exostosis or hypertrophic callus that develops after fracture of the first rib or clavicle. Patients with subclavian vein compression usually present with edema and pain of the hand and arm resulting from subclavian vein thrombosis.
Concerning the issue of treatment, questions arise as to whether surgery is indicated and, if indicated, what surgical technique and approach should be used. Most surgeons routinely attempt conservative treatment for patients with TOS before considering surgical decompression. Patients who have bone or soft tissue anomalies that compress arteries but are free of arterial damage may be managed conservatively by avoiding strenuous or repetitive arm movement. However, surgical decompression should be considered before arterial injury occurs. Generally, at the time of surgical intervention, median duration of symptoms is 24 months (range 1 to 180). Surgical decompression is more successful when TOS is traumatic or subacute, , suggesting that previous physical hard work has an influence on surgical results. Laborers with TOS are less likely to show successful results from surgical intervention, and they are unlikely to return to their original occupation and therefore may be required to pursue retraining for a non–labor-intensive occupation. A study that compared the outcomes of the nonoperative and operative workers, the majority of whom were diagnosed with disputed neurogenic TOS, showed that the surgically treated patients were three to four times more likely to be work disabled at follow-up. The treatment of spontaneous thrombosis of the subclavian vein has been conservative, but 50% of patients treated conservatively have persistent disabling symptoms. If vascular complications of TOS occur, aggressive, immediate surgical or endovascular intervention is needed.
The anatomy of the thoracic outlet extends from the intervertebral foramina and superior mediastinum to the axilla. The apex of the axilla is bounded by the clavicle and subclavius muscle anterolaterally, and the upper border of the scapula and subscapularis muscle dorsally. The anterolateral border of the first rib is medial. The brachial plexus and subclavian vessels leave this area and pass beneath the coracoid process. The nerve roots of the brachial plexus and the subclavian artery pass through the scalene hiatus (interscalene triangle) formed by the scalenus medius posteriorly, the scalenus anterior anteriorly, and the first rib (or cervical rib) inferiorly ( Fig. 192.1A ). It is important to note that the subclavian vein runs anterior to the anterior scalene muscle. Under normal circumstances, there is ample room for their passage, but congenital variations affecting the arrangement of ribs and scalene muscles in this area are responsible for almost all the compression lesions of the lower trunk and subclavian artery that fall into the category of TOS. Immediately distal to the interscalene triangle, the neurovascular bundle enters the costoclavicular triangle, which is bordered anteriorly by the middle third of the clavicle, posteromedially by the first rib, and posterolaterally by the upper border of the scapula. The neurovascular bundle then enters the subcoracoid space, also referred to as the retropectoralis minor space, beneath the coracoid process deep to the pectoralis minor tendon.
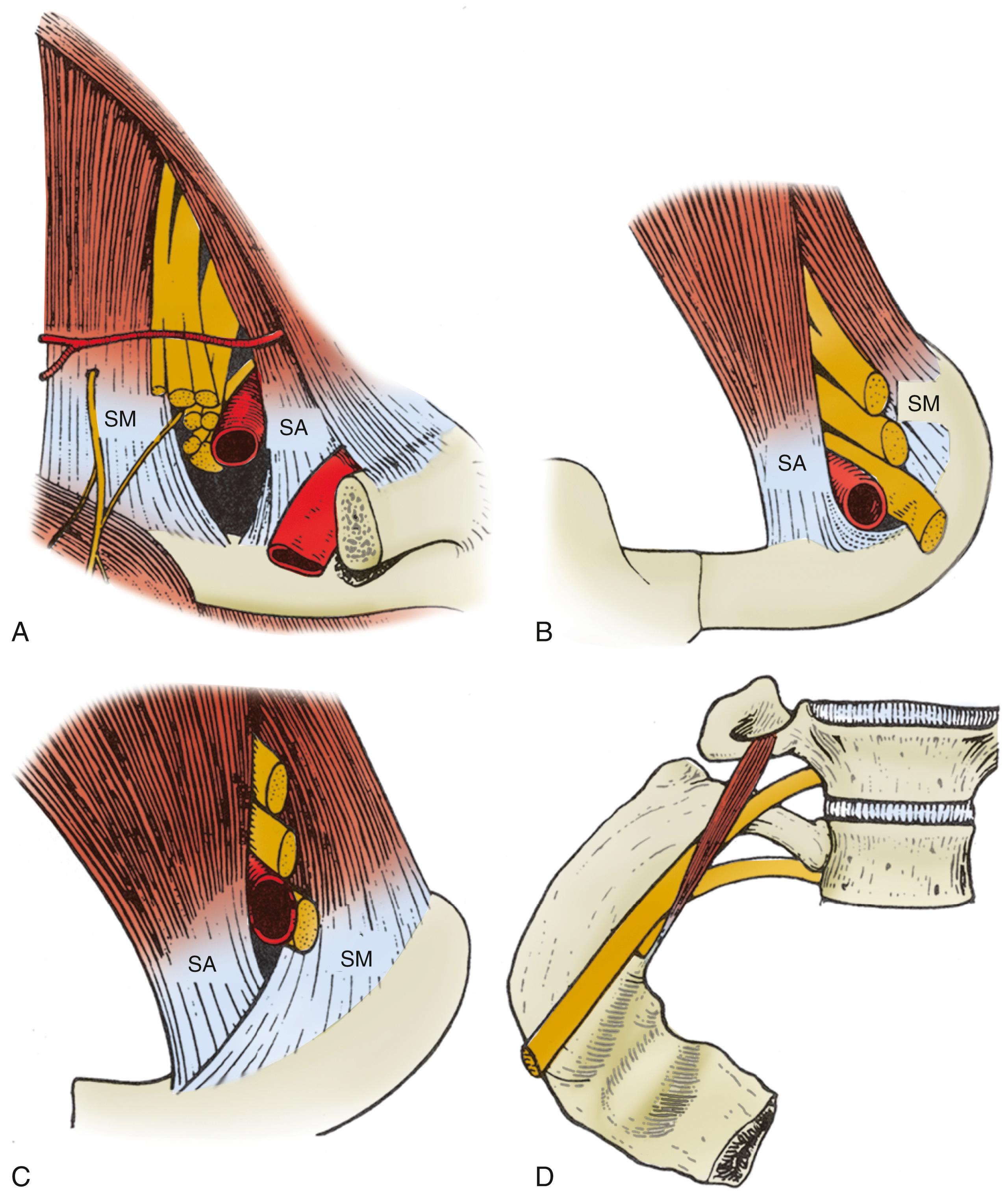
Compression and/or irritation of the brachial plexus within the thoracic outlet have been well described in three spaces: the interscalene triangle, the costoclavicular space, and the subpectoral tunnel. Magnetic resonance imaging (MRI) and computed tomography (CT) angiography studies also indicate that compression and/or irritation of the brachial plexus occurs within each of these spaces. Scalenus medius is normally inserted into the superior aspect of the first rib posterior to the vascular and neural groove and scalenus anterior into the scalene tubercle, which lies to the front of the groove separating the subclavian artery from the vein. In cases of TOS the scalene insertions may overlap or fuse, presenting sharp tendinous ridges over which the nerves and artery must pass (see Fig. 192.1B and C ). The presence of a cervical rib further alters the insertion of these muscles. If the rib is complete, the muscles are inserted into the cervical rib as they would be into the normal first rib; but when the cervical rib is incomplete, scalenus medius may be partly inserted into it and may continue as a tight fibrous band to be inserted into the first rib. This fibrous extension, known as the scalenus medius band, corresponds to the continuation of the cervical rib whose bony development has been arrested and is one of the more common findings in TOS. , Scalenus minimus, normally a small, inconstant muscle extending from the seventh cervical transverse process to the inner margin of the first rib, has occasionally been implicated as a source of nerve pressure as the first thoracic nerve root passes between this muscle and the scalenus medius (see Fig. 192.1D ). The arterial syndrome, on the other hand, is more likely to be associated with the complete cervical rib over which the artery must pass. The incomplete rib cannot extend far enough to exert pressure on the artery.
Brachial plexus compression (most often involving the lower trunk) within the thoracic outlet may occur in the following anatomic sites :
Where it rubs against a sharp tendinous posterior border of the scalenus anterior
Where it is compressed between the clavicle and a normal or abnormal rib, especially in cases when the costoclavicular space is reduced by an incomplete abnormal rib or callus around a healed fracture of the clavicle
Where it is crossed by the firm, free posterior border of Sibson’s fascia (the suprapleural membrane, a band of fibrous connective tissue that runs between the C7 transverse process and the apex of the parietal pleura)
Where it crosses the crescentic tendinous fibers of the scalenus medius
Where it is compressed in the intermuscular cleft between the scalenus medius and scalenus anterior
Where it is wedged in the narrow tendinous angle between the scalenus medius and scalenus minimus
Where it crosses an abnormal rib or the ligamentous extensions associated with such anomaly
Where it rubs across the site where an incomplete cervical rib articulates with the upper surface of the first rib
Many patients with suspected TOS fail to exhibit a clear-cut neurophysiologic and radiologic picture. Pathologies may present with signs and symptoms that mimic TOS, including cervical disc disease, cervical spondylosis, peripheral nerve entrapment disorders such as cubital tunnel syndrome, carpal tunnel syndrome, radial tunnel syndrome and pronator syndrome, nerve sheath tumors, Pancoast’s syndrome from bronchogenic carcinoma and brachial plexus metastases from breast carcinoma or other primary tumors. The diagnosis of TOS is best reached by careful clinical, radiologic, and electrophysiologic assessment.
The pain of TOS has no characteristic pattern and may be absent in cases with a severe neurologic deficit. The pain here is more common during the day. Typically, it can be aggravated by a variety of repetitive physical activities (particularly overhead), cold, and carrying heavy weights, but this is also true for such a wide range of disorders affecting the neck and arm that the character of the pain alone rarely is specific to the diagnosis. Also, coincidence of arm pain and a cervical rib is not sufficient for a diagnosis of TOS, although in cases with long-term follow-up it can suggest TOS.
Typically, patients complain about changes in manual dexterity or handwriting. Commonly, they experience similar symptoms with overhead use of the arm such as reaching to a high shelf or holding a hair dryer. Sometimes, driving or lifting weights provokes symptoms. In these cases, hypothenar, interosseous, or adductor pollicis weakness of a subtle degree is often detected. The muscle power of little and ring fingers may be weak, and less commonly, the median motor nerve distribution of the lower trunk may be affected. However, it is usually not observed in the absence of weak ulnar innervated musculature. Muscles supplied by the median, ulnar, and radial nerves may all be involved. It has been recognized that selective thenar muscle wasting, particularly of the abductor pollicis brevis and opponens pollicis, is visible in TOS patients. In classic neurogenic TOS, sensory disturbances are found in ulnar nerve distribution and motor disturbances in median and at times in ulnar distributions. Some patients exhibit significant weakness and atrophy of intrinsic hand muscles, the so-called Gilliatt-Sumner hand, in which a dramatic degree of atrophy occurs in the abductor pollicis brevis and lesser atrophy in the interossei and the hypothenar muscles. However, about half of TOS patients have no motor deficit at all. The sensory deficit, if present, usually affects the medial forearm, hypothenar eminence, and little and ring fingers. It essentially includes the ulnar nerve sensory distribution and that of the medial cutaneous nerve of the forearm. As with the motor findings, those of the sensory deficit may be subtle or even absent in symptomatic patients. The finding of neurologic deficits within the territory of more than one peripheral nerve points to the possibility of brachial plexus involvement.
Other clinical signs of importance are tenderness to pressure over the lower trunk at the site of compression. A cervical rib may produce a visible and palpable swelling. Vasomotor disturbances such as skin color and temperature changes may be seen in advanced cases, presumably related to compression of sympathetic fibers in the lower trunk, C8, and/or T1. Unilateral Raynaud’s phenomenon due to a sympathetic dystrophy sometimes occurs with neurologic TOS without involvement of the subclavian artery. Some patients report that they feel a cold arm, intermittent swelling, and fatigue of the limb when exercising, pallor, and/or cyanosis of the affected hand with diminished or absent distal pulses, which may reflect arterial compression. A supraclavicular mass or bruit may also be present. Thrombosis of the subclavian vein, also known as Paget-von Schrotter syndrome, manifests as upper extremity edema and cyanosis, with distended superficial veins of the shoulder and chest, often without complaints of pain. Some patients exhibit acute thrombosis of the subclavian vein, or so-called “effort thrombosis,” which should be treated aggressively with intravenous catheterization using thrombolytic agents and then anticoagulation.
Positive Tinel sign (pain or tingling on plexus percussion) over the brachial plexus beneath the scalene muscles and positional provocative maneuvers, and bruit or diminished or loss of radial artery pulse are helpful in increasing clinical suspicion, but many asymptomatic persons have these findings. Positional provocative maneuvers have sensitivity and specificity of 72% and 53%, respectively, although false-positive results were described in 45% for the Adson’s test, 77% in the Roos test, and 61% in the SCP (supraclavicular pressure) test.
Classic positional provocative maneuvers may be useful ( Fig. 192.2 ). The Adson test is performed with the patient seated and the examiner palpating the radial pulse with the patient’s arm dependent. The neck is turned with full extension toward the side of the lesion, while a deep breath is taken. In a positive test the radial pulse is reduced or lost.
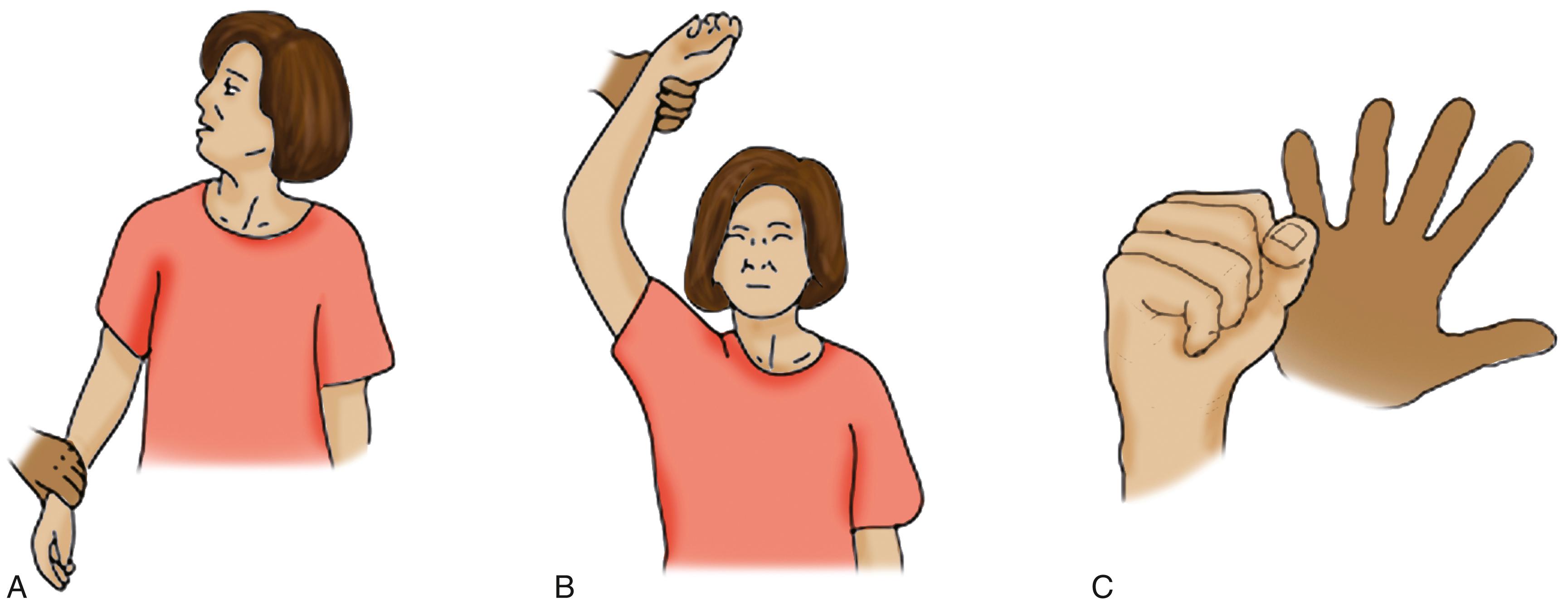
The Roos’s sign is markedly positive: rapid onset of symptoms when the arm is placed in the “surrender position” with the arm abducted, externally rotated and the elbow flexed. In the Wright test the arm is placed in the overhead position. This test has a higher rate of positivity, which may, in some cases, be increased by having the patient inhale deeply, or turn the head to the other side. The elevated arm stress test requires the patient to flex and extend the fingers with the arms in the surrender position, and in patients with significant compression, symptoms of fatigue and cramping will occur within 30 seconds.
With all of these tests, the examiner should auscultate the subclavian artery for the presence of a bruit. In some cases, color changes, indicating pallor or cyanosis, may be observed with the various maneuvers.
Electrophysiological evaluation can be of potential value in the diagnosis of TOS; however, it should always be interpreted in the context of clinical findings. For true neurogenic TOS, electrodiagnosis has traditionally rested on the findings of nerve conduction studies showing prominent loss of the median compound muscle action potential (CMAP) and ulnar sensory nerve action potential (SNAP) amplitudes, with less involvement of the ulnar CMAP in the setting of a normal median SNAP. Levin and colleagues and Cruz-Martinez and Arpa showed that medial antebrachial cutaneous SNAP is important in the electrodiagnosis of TOS. Abnormal nerve conduction velocities of the medial antebrachial cutaneous nerve, in the absence of other electrophysiologic findings, suggest neurogenic TOS. , Reduction of the ulnar SNAP amplitude is a nearly universal finding in this disorder, although the ulnar SNAP is less affected than the medial antebrachial cutaneous response. Many patients with TOS show normal electrophysiologic studies ; this is the typical finding in the disputed TOS cases. Lai and colleagues showed that the finding of abnormal preoperative somatosensory evoked potentials (SSEPs) correlates with a favorable outcome after surgery for TOS. Patients (93%) with abnormal preoperative SSEPs showed good postoperative outcomes compared to patients (60%) with normal preoperative SSEPs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here