Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Labour is defined as the onset of regular uterine activity, cervical effacement and dilatation with descent of the presenting part. The duration of labour is variable and is influenced by factors including parity, gestation or whether the labour was spontaneous or induced. First labours on average last 8 hours and are unlikely to last over 18 hours. Second and subsequent labours last on average 5 hours and are unlikely to last over 12 hours. In order to determine whether labour is progressing adequately, it is important to assess cervical dilatation and rate of change, uterine activity, and the position and station of the presenting part. The parity of the woman should always be considered for reasons just outlined. National clinical guidelines advise offering vaginal examination every 4 hours in labour in addition to abdominal palpation and assessment of vaginal loss.
Abdominal palpation should aim to define the lie, presentation, and position of the fetus. The lie refers to the long axis of the fetus in relation to the long axis of the uterus. The lie may be longitudinal, transverse or oblique. The presentation is that part of the fetus that is at the pelvic brim, in other words, the part of the fetus presenting to the pelvic inlet. ‘Normal’ presentation refers to the vertex of the fetal head, which is the area bounded by the anterior fontanelle (bregma), posterior fontanelle and biparietal eminences. ‘Malpresentation’ describes any non-vertex presentation. This may be of the face, brow, breech or some other part of the body if the lie is oblique or transverse.
The position of the fetus refers to the way in which the presenting part is positioned in relation to the maternal pelvis. This refers to any presenting part. However, it will be considered here in relation to those fetuses presenting head first (cephalic). As discussed in Chapter 31, the head is usually occipitotransverse at the pelvic brim and rotates to occipitoanterior (OA) at the pelvic floor. ‘Malposition’ is when the head, coming vertex first, does not rotate to OA, presenting instead as persistent occipitotransverse or occipitoposterior (OP). Vaginal examination should be performed to assess cervical dilatation and effacement in addition to station and position of the fetal head.
Uterine activity is monitored by measuring the strength, duration and frequency of contractions. This activity is recorded on the partogram in addition to the vaginal examination. During active labour, effective uterine activity is considered to be four to five contractions over a 10-minute period, lasting 40 seconds or more. Uterine overactivity presents as rapid, painful contractions, which are often associated with fetal distress. This can happen spontaneously but is more commonly associated with the use of oxytocics. Inadequate uterine activity is often associated with absent or slow cervical dilatation. Slow labour may result from inadequate uterine activity, cephalopelvic disproportion (CPD) or, more commonly, a combination of the two.
CPD refers to how well the fetal head fits through the pelvis and may occur if the fetal head is too big or the pelvis too small. It is subdivided into ‘true’ CPD if the head is in the correct position and ‘relative’ CPD if the obstruction is caused by malposition.
Precipitate labour has been defined as rapid birth of the fetus (a combined first stage and second stage of labour duration) within less than 2 to 3 hours of the onset of contractions, and may result from uterine overactivity.
Excessive uterine activity is commonly termed ‘uterine tachysystole’ or ‘hyperstimulation’. It is defined as more than five uterine contractions per 10 minutes in at least two consecutive intervals. There may be signs of fetal distress on the cardiotocograph due to interference with the placental blood supply.
Spontaneous hypercontractility, excessive uterine activity not resulting from the administration of medications, is rare. Spontaneous uterine hypercontractility may be associated with placental abruption (see p. 316).
Uterine hyperstimulation occurs much more commonly. By definition, it is caused by the use of oxytocics. Both oxytocin and prostaglandins may be implicated. The choice of dosage regimens for each represents a compromise between efficacy and the risk of hyperstimulation. The appropriate dose of oxytocin remains controversial, but there is good evidence for starting at a low dose, around 0.5 to 4 mU/min, and increasing incrementally to 12 mU/min. The dose should be increased no more frequently than every 30 minutes until there are 4 to 5 contractions in 10 minutes. While the licenced maximum dose in the United Kingdom is currently 20 mU/min, some clinicians support the use of regimens up to 32 or even 40 mU/min.
With prostaglandins, hyperstimulation is also a significant risk but is less likely if their administration is intravaginal rather than oral, intracervical or directly extra-amniotic.
Precipitate labour resulting from either spontaneous hypercontractility or uterine hyperstimulation may lead to fetal distress. Normal labour, with sufficient physiological relaxation time, allows the oxygenation level of an uncompromised baby to be restored between contractions. However, strong contractions and a shortened relaxation time does not allow the blood supply to the placenta to return to baseline levels before the next contraction, which can result in fetal acidosis ( Fig. 34.1 ). Precipitate labour may also predispose to uterine rupture in parous women, particularly if there is a pre-existing caesarean section scar.
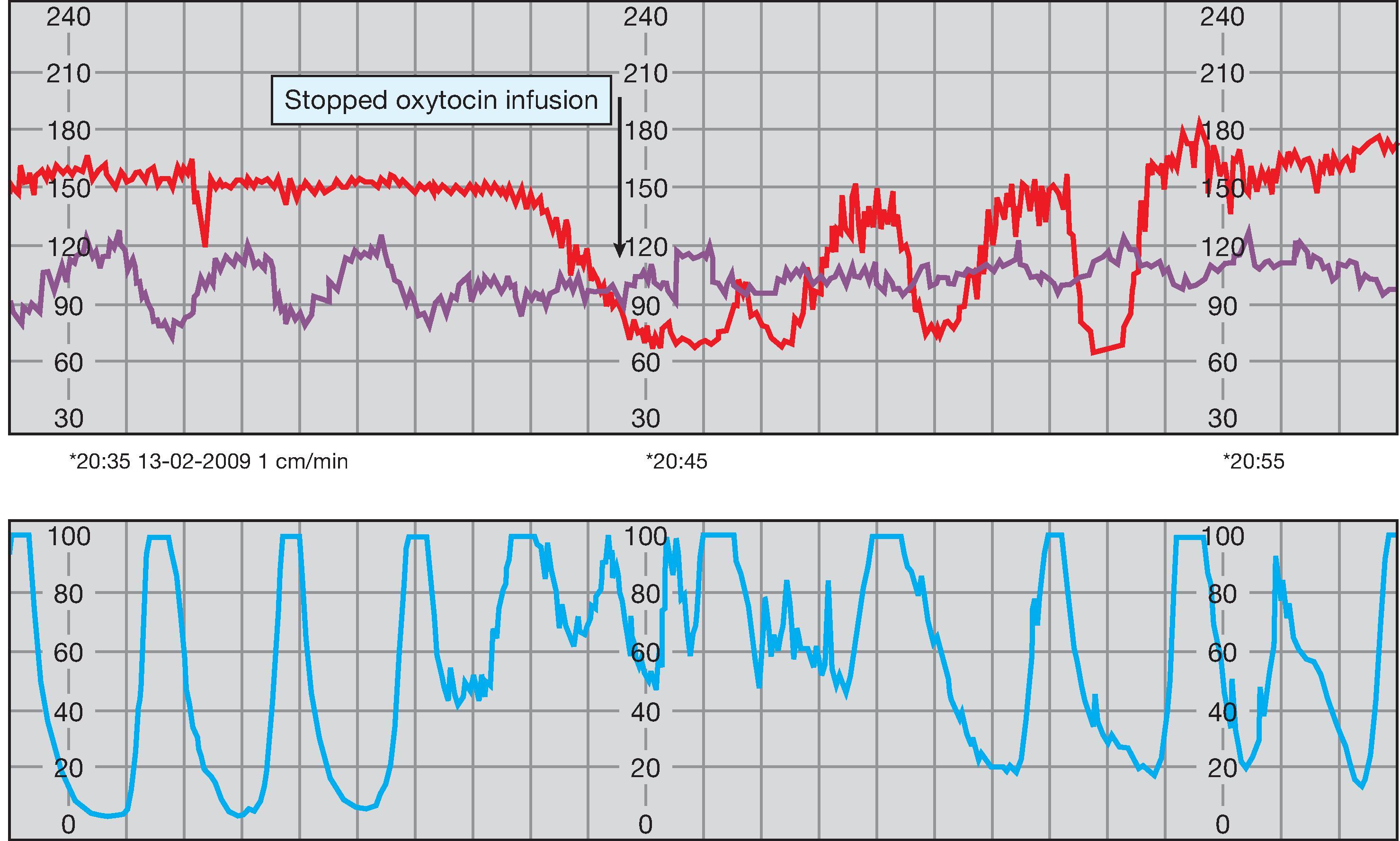
Management of precipitate labour is largely dependent on the fetal condition. If an oxytocin infusion is running, it should be stopped and the woman turned to the left lateral position. A tocolytic agent (a drug to relax the uterine muscle, for example, a bolus of subcutaneous terbutaline or sublingual glyceryl trinitrate spray) may be administered. If severe fetal distress is apparent, it may be necessary to expedite the birth of the baby, either instrumentally or by caesarean section, depending on the dilatation of the cervix. If a caesarean section is arranged, a vaginal examination prior to starting the operation should be considered, as the cervix may dilate rapidly during the time taken to transfer to theatre, especially in a parous woman.
Precipitate labour is associated with an increased risk of complications for the woman, including cervical and perineal tears, retained placenta, postpartum haemorrhage and the need for a blood transfusion.
Frequent uterine contractions are also a feature of placental abruption (see Chapter 26). Contractions with a frequency of more than one every 2 minutes are highly suggestive of this and these frequent contractions may increase the distress of a fetus already compromised by partial placental separation. The diagnosis of placental abruption is even more likely if there is associated lower abdominal pain, backache or vaginal bleeding. As a general rule, tocolytic drugs should not be used to manage the uterine hypercontractility associated with placental abruption, as uterine relaxation may exacerbate the bleeding and precipitate further placental separation.
Slow progress in the first stage of labour is diagnosed by assessing the rate of cervical dilatation. As discussed on pages 374 and 404, progress can be monitored on a partogram, and alert lines can be used to identify women who are progressing slowly. Early identification and intervention makes it more likely that the woman will have a vaginal birth. The definition of slow labour is controversial; traditional obstetric practice suggested that any nulliparous woman with a rate of cervical dilatation less than 1 cm/h required treatment for slow progress. More recently, a rate of cervical dilatation of less than 0.5 cm/h has been adopted as the threshold. UK national clinical guidance suggests that a diagnosis of delay in labour should be made when there is dilatation of less than 2 cm in 4 hours.
The second stage of labour is defined as between full dilatation of the cervix to birth of the baby, and is divided into passive and active stages. Active second stage is commenced when the woman develops expulsive contractions with the urge to push or when active pushing is commenced and usually follows 1 to 2 hours of passive second stage. Delay in the second stage should be diagnosed if birth is not imminent despite 2 hours of active second stage in a primigravida or 1 hour in a parous woman.
Slow labour is associated with:
Eventual fetal ‘distress’ and risk of fetal hypoxic injury
Increased risk of intrauterine infection, leading to fetal and maternal morbidity
Increased risk of postpartum haemorrhage
Maternal anxiety and longer-term psychological morbidity
A loss of confidence in those providing maternity care.
These, in turn, are associated with a greater chance of the woman giving birth by caesarean section or requiring an instrument vaginal birth. The causes of slow labour are summarised in Table 34.1 and the outcomes in Table 34.2 .
| Clinical Features | Caused by |
|---|---|
| Prolonged latent phase | Idiopathic |
| Prolonged active phase and secondary arrest | Inadequate uterine activity: hypoactive |
| incoordinate | |
| Obstruction (CPD): | |
|
|
|
| Cases | SpontaneousVertex Birth | InstrumentalBirth | CaesareanBirth | |
|---|---|---|---|---|
| Normal pattern | 65–70 | 80 | 18 | 2 |
| Prolonged latent phase | 2–5 | 75 | 10 | 15 |
| Prolonged active phase | 20–30 | 55 | 30 | 15 |
| Secondary arrest | 5–10 | 40 | 35 | 25 |
Chapter 31 describes how the first stage of labour is divided into two parts: the latent phase (from the onset of contractions until the cervix is fully effaced) and the active phase (when the cervix begins to dilate). The normal duration of the latent phase of labour in primigravidae ranges from 1.7 hours up to 15.0 hours. The latent phase is most likely to be prolonged in those whose cervix is unfavourable. Therefore, a prolonged latent phase is much more common in primigravidae ( Fig. 34.2 ).

There is rarely any serious cause for a prolonged latent phase. CPD is usually evident at more advanced stages of cervical dilatation. With a prolonged latent phase, the woman often becomes weary, exhausted and demoralised from what can sometimes be discomfort over a number of days. A prolonged latent phase of labour is associated with more obstetric intervention (e.g., caesarean birth) and poor fetal outcomes (e.g., admission to the neonatal unit). Within reason, it is important to resist the temptation to actively intervene by artificially rupturing the membranes or administering oxytocics, at least until the cervix is 2 or 3 cm dilated and fully effaced with a well-applied presenting part. Intervention may actually increase the risk of further obstetric intervention in what might, with patience, have been an uneventful labour. Reassurance, encouragement, hydration and appropriate analgesia over this time are extremely important.
The active phase may be prolonged because of inadequate uterine activity or CPD ( Fig. 34.3 ).

The uterus may be hypoactive or incoordinate. A hypoactive uterus is one with low resting tone and only weakly propagated contractions. There is often a longer interval between contractions and the contractions are not particularly painful.
Incoordinate uterine activity may occur because of inadequate ‘fundal dominance’. Normal uterine contraction begins at a pacemaker point close to the junction of the uterus and the fallopian tube. It spreads from this point downwards, with its intensity maximal at the fundus (where the muscle is thickest), intermediate at the mid-zone, and least at the lower segment. Uterine contractions can be described in terms of baseline tone, amplitude, frequency, and duration. With incoordinate uterine activity, the intensity profile appears to be reversed, with the maximal intensity in the lower segment (where the muscle is thinnest) and weakest at the fundus. This is much less efficient. The resting tone is increased throughout and, therefore, the threshold for pain is reached earlier in the contraction. Incoordinate uterine activity is common, especially in women in their first labour. Contractions may be incoordinate in terms of frequency, duration or strength, or a combination.
Inadequate uterine activity has no specific cause—it may simply be a developmental feature of the uterine muscle. There is evidence that many will resolve spontaneously given sufficient time. There is also some evidence that inadequate uterine activity is associated with CPD. This is because cervical dilatation itself may improve uterine activity, but it is less likely to occur if the presenting part is pressing less firmly on the cervix.
If progress is satisfactory, there is no need to consider treatment of incoordinate uterine activity. Most will respond well to oxytocics, usually given by a stepwise intravenous oxytocin infusion, as described earlier. As labour is likely to be prolonged, care should be taken to make sure that the woman does not become dehydrated or ketotic, as this will further exacerbate the uterine problem.
This may occur because of the following:
The baby’s head is presenting in the optimal way but is too large relative to the pelvis (‘true’ CPD). It is diagnosed only if the head does not become engaged despite adequate uterine activity. It is not possible to predict CPD antenatally, and even using the strictest antenatal criteria, many of those considered to be at risk by clinical pelvic assessment will go on to have a vaginal birth. More complicated attempts to predict CPD using ultrasound measurements of the fetal head together with X-ray or computed tomography pelvimetry measurements have also proved to be unreliable and only lead to unnecessary surgical intervention. Short maternal stature or small shoe size are not predictive of CPD. The only true test is labour itself.
There is a malpresentation or malposition of the baby’s head so that a wider part of the head is being presented to the pelvis. This is ‘relative’ CPD. It may occur with deflexed malpresentations (particularly of the brow and face; see p. 409), but the most common cause of relative CPD occurs when the head rotates to the OP (see p. 417) rather than the OA position. The first stage and second stage progress more slowly; although spontaneous delivery is quite possible with the head coming out ‘face to pubis’, secondary arrest is not uncommon.
There is some form of pelvic abnormality. Major abnormalities are uncommon, particularly in well-resourced settings, and are usually associated with disease, injury or severe nutritional problems. The obstetric classification is based on the shape of the pelvic brim, as it is the pelvic inlet, which seems to be the major determinant of vaginal birth ( Fig. 34.4 ).

The round ‘gynaecoid’ pelvis is the most common and, as would be teleologically predicted by the theory of natural selection, it is obstetrically ideal. The long oval ‘anthropoid’ pelvis is also relatively common but is associated with OP presentation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here