Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Early detection of oral cancer directly results in improved survival after treatment.
Tobacco use and habitual alcohol consumption synergistically increase the risk of developing oral carcinoma.
For most presentations of cancer of the oral cavity, the risk of occult spread to the regional lymphatics exceeds 20% and warrants elective treatment of the regional lymphatics.
Functional recovery after a significant oral cavity resection depends on adequate mobility and bulk of the soft tissue components and frequently requires pedicled flaps or free tissue reconstructive techniques.
For patients with advanced-stage oral cavity carcinomas (overall stage III or IV), combined modality treatment with surgical resection and adjuvant radiation (or chemoradiation) therapy remain the treatment of choice.
Although impacting prognosis in the care of patients with oropharyngeal carcinoma, human papilloma virus–positivity does not offer a survival advantage for patients with an oral cavity cancer.
The topic of malignant neoplasms of the oral cavity is synonymous with a discussion of oral squamous cell carcinoma (SCC). The oral cavity is unique in that unlike other anatomic regions of the upper aerodigestive tract, the routine detection of early-stage lesions is possible. However, given the relatively common presentation of other benign pathology within the oral cavity, such as aphthous ulceration, delay in diagnosis can occur.
Oral cavity malignancies (excluding those of the lip) account for approximately 25% of all head and neck cancers. Perhaps more so than in other sites within the head and neck, primary surgical management represents the treatment of choice. In assessing the treatment strategy, the surgeon attempts to maximize locoregional tumor control while acknowledging the potential functional impact of a procedure on speech and swallowing. The appropriate selection of reconstructive techniques that assist appropriate wound healing, potentially prior to adjuvant radiation, while maximizing the patient's capacity for oral rehabilitation, requires a broad knowledge of available options.
The current estimate from the Centers for Disease Control and Prevention report is that 15.1% of adults in the United States are considered smokers. Tobacco and alcohol consumption are considered to be the most common preventable risk factors associated with the development of oral cavity SCC. In addition, this relationship is synergistic, with alcohol serving as a promoter for the carcinogenic effects of tobacco. When compared with nonsmokers, smoking confers a 1.9-fold risk to males and a 3-fold risk to females for development of head and neck SCC. The risk is directly proportional to the years spent smoking and the number of cigarettes smoked per day. Alcohol alone confers a 1.7-fold risk to males who drink one to two drinks per day compared with nondrinkers. This risk rises to more than 3-fold for heavy drinkers. Individuals who both smoke (two packs per day) and drink (four units of alcohol per day) are 35 times more likely to develop cancer when compared with controls. Approximately 9% of U.S. adults meet the criteria for an alcohol-use disorder.
In a review of the smoking-related data of 216,917 adults (25 years of age and older) from the U.S. National Health Interview Survey (1997 to 2004), Jha and colleagues noted that the rate of death from any cause among current smokers was three times that of those who had never smoked (ages 25 to 79 years). The majority of this increase in mortality was related to neoplastic, vascular, respiratory, and other smoking-related causes. They also found that life expectancy was decreased by more than 10 years in current smokers when compared with those without a history of smoking. However, if individuals stopped smoking before the age of 40, the risk of death (associated with continued use) was decreased by 90%. Although smoking rates have declined, the rate of death from chronic obstructive pulmonary disease continues to increase in both male and female smokers and may be related to the change in smoking habits associated with modifications in cigarette design that have promoted deeper inhalation. Given the high likelihood of chronic obstructive pulmonary disease in head and neck cancer patients the importance of the collaborative management of this diagnosis, while emphasizing smoking cessation, should not be understated. The length of time that smoking cessation is initiated prior to surgery has not been associated with an increased risk for postoperative complications.
A retrospective cohort study of 463 patients with the diagnosis of a head and neck cancer noted that patients who were smokers (56.2%) were more likely to be younger, unmarried, and drink alcohol regularly. Their median survival was also compromised when compared to nonsmokers (89 vs. 208 months). The authors advocated the importance of social support services as individualized cancer care models are adopted for those patients without a clear family or peer support network.
When patients are asked to pursue smoking cessation and later surveyed upon their success, a high false-negative rate is noted when the quality of the survey results are assessed with subsequent urinary cotinine levels. In a study by Alberg et al., 39% of head and neck surgical patients were biomarker positive yet denied recent tobacco use when surveyed. These findings support the concern that underreporting can occur when patients are questioned about their social habits.
Smokers more frequently present with tumors of the larynx, hypopharynx, and floor of the mouth. The time to first cigarette (TTFC), considered a distinct nicotine-dependence phenotype, is an indicator of risk for head and neck cancer. The odds ratios for the development of a head and neck cancer are highest for patients with a 1- to 30-minute TTFC. This early TTFC is also associated with the inability to quit smoking and relapse after cessation. Mutations of TP53 and genetic alterations such as loss of heterozygosity at 3p, 4q, and 11q13 and also losses in the overall number of chromosomal microsatellites (repeated base sequences) are significantly more likely in the tumors of smokers. Former smokers, defined as those individuals who had quit more than 10 years earlier, demonstrate a genetic profile more consistent with nonsmokers.
In a systematic review and meta-analysis, Hackshaw et al. showed that smoking only one cigarette a day still carried significant risk (50% that of individuals smoking 20 cigarettes per day) for future cardiovascular and cerebrovascular disease, reiterating the theme for patients that there is no “safe smoking” volume and cessation should always be the goal.
Despite conflicting reports from various cohort and case-control studies, the World Health Organization International Agency for Research on Cancer has concluded that evidence is sufficient to state that smokeless tobacco causes oral and pancreatic cancer in humans. Carcinogens N-nitrosonornicotine and 4-methylnitrosamino-1-(3-pyridyl) 1-butanone are found in smokeless tobacco and are considered to be responsible for the induction of oral tumors in animal models. A fourfold increased risk of oral cavity carcinoma was reported in users of smokeless tobacco compared with nonusers.
Experienced e-cigarette users can obtain the same amount of nicotine exposure as that from combustible tobacco cigarettes. The majority of flavorings and humectants (glycerol and polypropylene glycol) that are in use have been regarded as safe by the FDA; however this designation applies to oral consumption and little evidence exists regarding the safety of inhalational exposure. Although considered to have less risk for harm than combustible tobacco products, the long-term side effects remain unknown (first imported in 2006).
Betel nut (including its derivatives, such as betel quid) is chewed by an estimated 10% of the world population. Various other substances, such as tobacco, are typically added to the betel nut prior to use. Surprisingly, the addition of tobacco does not significantly increase the carcinogenicity of the product beyond the already well-established risk seen with habitual use of betel nut. Oral submucosal fibrosis (OSF) is a chronic inflammatory reaction associated with the habitual use of betel nut and betel quid and typically presents as a burning sensation in the oral buccal mucosa that results in severe trismus on examination. A dose-response relationship occurs with habitual use, and the rate of malignant transformation has been reported to be greater than 5%.
Environmental ultraviolet light exposure is associated with the development of lip cancer. The projection of the lower lip, as it relates to this solar exposure, has been implicated in the pathogenesis of SCCs that arise on the vermilion border of the lower lip. Mechanical irritation, thermal injury, and chemical exposure are suspected to be responsible for the subsequent development of malignancy in pipe-smoking patients who develop lip carcinoma.
Fanconi anemia is a rare genetic disorder, with an incidence of about 1/130,000 live births, in which most patients develop subsequent bone marrow failure that requires stem cell transplantation. Development of various cancers, such as acute myelogenous leukemia or head and neck neoplasms, is not uncommon in this population. In a series of 12 patients reviewed by Birkeland and colleagues, head and neck cancer was diagnosed at a mean age of 35.5 years. The majority of the patients (8/12) were diagnosed with an oral carcinoma. Fanconi anemia patients have a high rate of complications with radiation therapy, including severe mucositis, dysphagia, and pancytopenia. In this series, four patients died during the course of radiation therapy. For the group overall, mean disease-free survival (DFS) and overall survival (OS) were 15.7 and 33.7 months, respectively.
Dental restorations composed of varying substances have been investigated for a potential association with the development of oral cancer. Patch testing for patients with oral dysplasia or carcinoma, without traditional risk factors, has been advocated for patients with metallic dental restorations adjacent to oral lesions of concern. In a study of 65 oral carcinoma patients, 34% were found to be allergic to at least one metal adjacent to their lesion of concern. Patients with oral carcinoma were three times more likely (12% overall) to react to mercury and amalgam compounds than nonallergic controls. The authors advocate that the removal of metal restorations should be considered in selected patients with positive reaction to patch testing.
Oral trauma remains a concern relative to the risk of future development of dysplasia and carcinoma. In a retrospective analysis of 881 patients with oral cavity and oropharyngeal carcinoma, Perry et al. showed that nonsmoking females were more likely to develop carcinoma in sites like the lateral tongue where dental trauma is more common. The authors also noted older nonsmoking denture-wearing patients were more likely to develop alveolar ridge and floor of mouth carcinoma in their series.
Other entities that have a potential association with the development of oral carcinoma include Plummer-Vinson syndrome (achlorhydria, iron deficiency anemia, and mucosal atrophy of the mouth, pharynx, and esophagus), chronic infection with syphilis, long-term immunosuppression, and HIV infection.
In a review of 200 HIV-positive patients, 8% had also been diagnosed with an oral cavity carcinoma. These patients typically presented at a younger age (mean 31.7 years) with poorly differentiated tumor and stage III/IV disease. During the era of highly active antiretroviral therapy (from 1996 through 2006), standardized incidence ratios (assessing risk relative to the general population) in patients with AIDS demonstrated elevated risk for the development of cancers of the oral cavity/pharynx, tongue, anus, liver, larynx, lung/bronchus, and penis and also Hodgkin lymphoma.
Patients on immunosuppression diagnosed with an oral cancer, with or without concomitant glucocorticoid therapy, demonstrate a higher likelihood of regional metastasis and extracapsular spread of lymph node metastases.
Patients who have undergone hematopoietic stem cell transplant can develop chronic graft-versus-host disease with significant oral manifestations. When oral cancer develops in this setting, the cancers are more likely to be multicentric and locoregional aggressive when compared with immunocompetent patients. This population requires regular follow-up assessments.
Tumor development represents the loss of multiple signaling mechanisms that regulate the control of cell growth. Advances in molecular biology have allowed for the identification of many of the mutations associated with this transformation. Contemporary molecular analysis of tumors is providing insight into the processes of malignant transformation and tumor progression.
Human papilloma virus (HPV) is an epitheliotropic virus detected to varying degrees within samples of oral cavity SCC. The overall incidence of oral HPV infection in the United States, based on 2009/2010 survey data, was 6.9% in men and women aged 14 to 69 years. Oral HPV subtype 16 infection was 1.0%. The prevalence of oral HPV was significantly higher in men and was linked to the number of sexual partners in the patient history and the number of cigarettes smoked per day. For nonoropharyngeal carcinomas, no significant data are available to suggest that a survival advantage or improved prognosis can be experienced at other head and neck primary sites found to be HPV positive.
The neutrophil-to-lymphocyte ratio (NLR), considered a marker reflecting of host inflammation status, was examined in over 1200 patients with oral squamous carcinoma. Researchers found that patients with a high NLR had a worse OS but were potentially better responders to systemic chemotherapy.
Chen et al. demonstrated a negative correlation between strong Rap-1A, a subgroup of the Ras family of G-proteins, expression and overall and 5-year disease-specific survival (DSS) for patients with oral cavity carcinoma. Rap-1A expression, modulated by Aurora-A, may be one of the mechanisms responsible for metastasis and was advocated by the authors as a potential marker for identifying patients with aggressive presentations of oral cavity carcinoma.
In 57 patients with oral squamous carcinoma, Metin et al. noted statistically significant lower mean serum levels of paraoxonase 1 than in healthy controls. Paraoxonase 1 is an enzyme with activity against carcinogenic liposoluble radicals and levels are noted to be decreased in patients who smoke.
MTBP is an MDM2-binding protein that can alter p53/MDM2 homeostasis, and it correlates with Ki-67 expression; it likely has both oncogenic and tumor-suppressing properties. Vlatkovic and colleagues generated and validated an antibody to MTBP and utilized it in evaluating 198 head and neck SCC samples. They revealed that the biomarker combination of p53 positivity and low MDM2 levels were significantly associated with reduced OS. In patients with this phenotype, the authors also found that loss of MTBP expression was associated with markedly reduced OS.
MicroRNA-137 plays an essential role in cell cycle control at the G1/S phase checkpoint. Langevin and colleagues detected aberrant microRNA-137 promoter methylation in 16.4% (11/67) of head and neck SCC specimens (oral cavity, 4; oropharynx, 5; larynx, 2). This finding was seen more frequently in individuals who ate fewer daily servings of fruit and vegetables and was significantly associated with a lower OS rate.
In a unique study examining the contents of patients’ postoperative drain fluid, Lassig et al. found that the matrix metalloproteinase 1 (MMP-1), MMP-3, and soluble FMS-like tyrosine kinase-1 (sFlt-1) levels in the drains of 20 patients, sampled during their postoperative hospitalization, correlated with patient's subsequent clinical course and was predictive of future recurrence. In the six patients who developed recurrence the MMP-1, MMP-3, and sFlt-1 drain fluid levels were significantly lower than in those patients who were recurrence-free at 1 year.
High perinodal monocarboxylate transporter (MCT) 4, normally a transporter of pyruvate and lactate out of cells, has been associated with worse survival in patients within regionally metastatic oral cavity carcinoma and may be a future marker for identifying patients with aggressive disease compromising DFS. MCT 4 is upregulated in the setting of hypoxia and inflammation and is found with cancer-associated fibroblasts.
A new approach in cancer therapy includes the development of the DNA damage response (DDR) kinase inhibitors. This class of drugs has the capacity to increase the efficacy of conventional DNA-damaging therapies by inactivating a cell's DNA repair pathway activation. DDR inhibitor-9, an example of this class of drugs, has demonstrated the ability to enhance the toxicity of etoposide and ionizing radiation in preclinical trials. Additional investigation into the role of this line of therapy is ongoing in clinical trials.
In a study of whole-exome sequencing, Agrawal and associates identified six gene mutations— TP53, CDKN2A, PIK3CA, HRAS, FBXW7, and NOTCH1 —in multiple specimens that were associated with the development of head and neck SCC. Findings from this study suggested that NOTCH1 functions as an important tumor suppressor gene in head and neck SCC. Overexpression of mutant TP53 has been associated with carcinogenesis at multiple sites. Point mutations in TP53 have been reported in up to 45% of head and neck squamous carcinomas. Koch et al. noted that TP53 mutation is a key event in the malignant transformation of more than 50% of head and neck SCCs in smokers.
The Akt receptor has been correlated with the histologic progression of oral premalignant lesions to carcinoma. Massarelli and colleagues demonstrated that phosphorylated Akt, when highly expressed, is associated with recurrence and shorter DFS independent of a patient's overall staging.
Apolipoprotein E (APOE), which is normally involved in cellular cholesterol efflux, is believed to have a significant role in tumor invasion with oral cavity squamous carcinoma. Jayakar et al. demonstrated with siRNA knockdown of specific genes in an oral carcinoma cell line that the reduction of APOE was associated with a reduction in tumor invasion. Additionally, levels of activator protein-1 were also reduced, as APOE was negatively affected, which resulted in a downstream impact on MMP-7 expression. The authors concluded that high levels of APOE expression are associated with a more aggressive and invasive phenotype of oral carcinoma.
DF3/MUC1 overexpression is associated with regional metastatic spread and is considered an indicator of poor prognosis. DF3/MUC1 protein, which functions as a oncogene, is not expressed in normal squamous epithelium and when expressed in cancer cells is typically at the invasive front of the tumor.
Habitual betel quid use that results in the development of an oral malignancy has been shown to have an association with tissue inhibitor of metalloproteinase-3 (TIMP3) rs9862 polymorphisms. TIMP3 normally binds extracellular matrix and can suppress tumor growth and migration and loss of TIMP3 expression is associated with a poor prognosis in the setting of cancer.
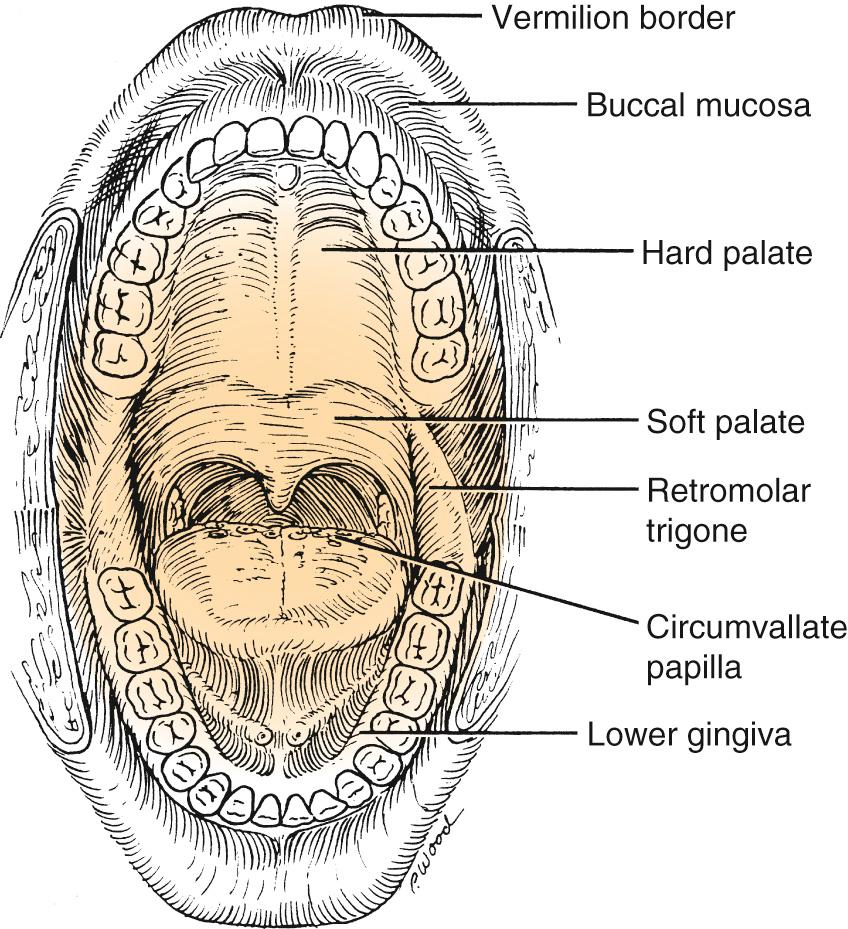
An understanding of the complex anatomic relationships of the oral cavity is paramount to achieving satisfactory oncologic and functional results. The oral cavity extends from the vermilion border of the lip posterosuperiorly to the hard palate–soft palate junction, posteroinferiorly to the circumvallate papillae (linea terminalis), and posterolaterally to the anterior tonsillar pillars. It is divided into seven specific subsites: (1) the lips, (2) dentoalveolar ridges, (3) oral tongue, (4) retromolar trigone, (5) floor of mouth, (6) buccal mucosa, and (7) hard palate ( Fig. 91.1 ).
The local, regional, and distant spread of an oral cavity cancer is dependent on the course of the neurovascular anatomy, lymphatic pathways, and fascial planes of the head and neck. The latter serve as a barrier to the direct spread of tumor and can influence the pattern of growth. In addition, perineural and angiolymphatic invasion can act as a conduit for the spread. When present, these aggressive histologic findings can have a profound impact on the patient's prognosis and long-term survival.
Patients previously treated with either surgery or radiation for a head and neck malignancy may demonstrate atypical patterns of local invasion and regional spread of tumor. A brief discussion of the vascular and lymphatic anatomy pertinent to the oral cavity is necessary before considering diagnostic and treatment options.
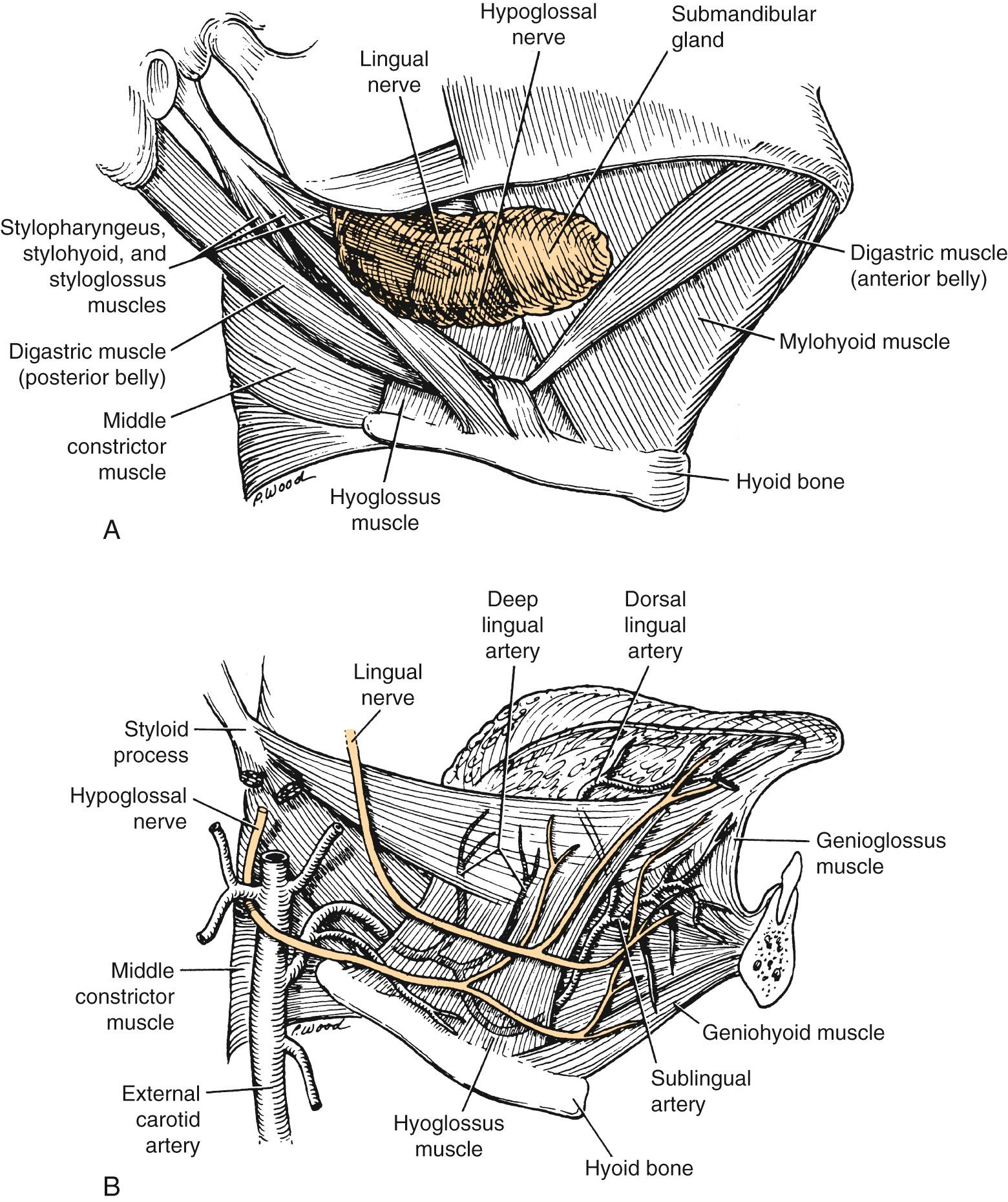
The arterial supply to the oral cavity includes multiple contributions from the external carotid artery. The lingual artery provides the majority of the vascular supply to the oral tongue and tongue base. Identification of the artery within the neck requires the exposure of the floor of the submandibular region. The artery is found deep to the hyoglossus muscle and requires the division of the muscle for maximal exposure. Superficial to the hyoglossus and deep to the mylohyoid muscle are the hypoglossal nerve and lingual veins ( Fig. 91.2A and B ). An understanding of this relationship can aid in the localization of the artery when necessary for microvascular reconstruction or selective ligation. The ranine vein, which closely approximates the nerve in this region, is prone to injury during dissection and necessitates care if hypoglossal nerve injury is to be avoided.
The hard palate blood supply is derived from the greater palatine and the superior alveolar arteries. After branching off the descending palatine artery at the greater palatine foramen in the region medial to the second maxillary molar, the artery runs anteromedially within the soft tissue of the hard palate ( Fig. 91.3 ). The venous drainage is to the pterygoid plexus and subsequently to the internal jugular venous system. The superior alveolar arteries—anterior, middle, and posterior—arise as terminal branches after the transition of the internal maxillary artery to the sphenopalatine artery at the pterygopalatine fossa. These arteries provide blood supply to the maxillary gingiva, alveolar ridge, and dentition.

The facial artery crosses over the lateral aspect of the mandible approximately 1 cm anterior to the ascending ramus and courses toward the oral commissure, where it gives rise to the labial arteries. These paired vessels are readily apparent during lip-splitting procedures and anastomose in the midline to create a vascular ring.
The primary vascular supply to the mandible and the lower dentition is from the inferior alveolar artery. Blood supply from the mandibular periosteum becomes more important with advancing age. The inferior alveolar artery, vein, and nerve enter the mandibular foramen along the medial aspect of the ramus of the mandible. Before their entry into the foramen, both the nerve and artery send off branches that extend anteriorly to supply the mylohyoid muscle.
The posterior floor of the mouth and retromolar trigone has an arterial supply and venous drainage similar to that of the anterior tonsillar region. The ascending pharyngeal and lesser palatine vessels contribute to the vascularity that may be encountered with surgical procedures at this site.
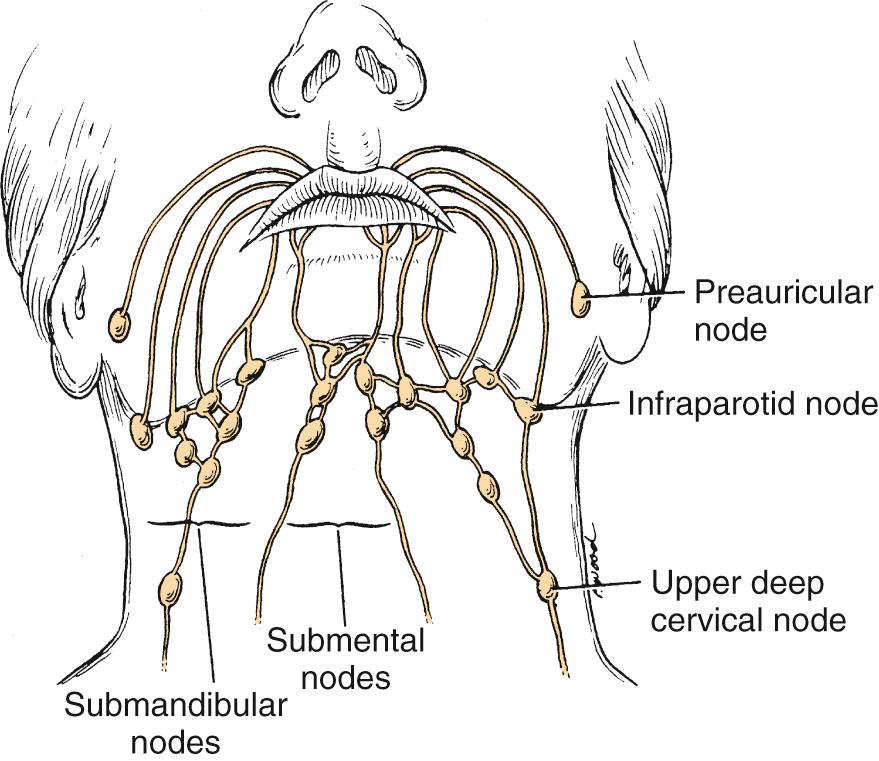
The lips represent a transition from external skin to internal mucous membrane that occurs at the vermilion border. The underlying musculature of the orbicularis oris, innervated by the facial nerve, creates a circumferential ring that allows the mouth to have a sphincter-like function. The sensation for the upper lip is supplied by the infraorbital nerve (cranial nerve [CN] V2), whereas sensation for the lower lip is provided by the mental nerve (CN V3). Lymphatics from both the upper and lower lips drain primarily to the submandibular lymph nodes, yet midline lower-lip lesions may present with submental lymphatic spread. In addition, the upper lip may drain to preauricular, infraparotid, and perifacial lymph nodes ( Fig. 91.4 ).
The lateral aspect of each alveolar ridge is represented by the mucosal sulcus created by the transition of tissue to buccal mucosa. On the lower alveolus, the medial margin is marked by the transition to the floor of the mouth; on the upper maxillary alveolus, the transition is the horizontal orientation to the hard palate. The posterior margin of the lower alveolus is the ascending portion of the ramus of the mandible, whereas it is the superior aspect of the pterygopalatine arch for the upper alveolus. The close approximation of mucosa to underlying bone facilitates the potential for early cortical invasion for malignant tumors in this region.
The oral cavity portion of the tongue is defined as that portion anterior to the linea terminalis. The tongue is composed of four intrinsic and four extrinsic muscles separated at the midline by the median fibrous lingual septum. The extrinsic muscles originate outside the substance of the tongue and include the genioglossus, hyoglossus, styloglossus, and palatoglossus. Of these, the genioglossus, which functions to depress and protrude, provides the majority of the bulk to the tongue. The paired intrinsic muscles of the tongue (superior-inferior longitudinal, transverse, and vertical) lie superficial to the genioglossus and function to alter the overall shape of the tongue. These muscles run with the tongue in three different orientations, and this lack of distinct planes between muscles can allow for a diffusely infiltrating pattern of tumor growth. All of the musculature of the tongue derives its motor innervation from the hypoglossal nerve with the exception of the palatoglossus, which is supplied by a pharyngeal branch of the vagus nerve. The general sensory function of the anterior two thirds of the tongue is provided by the lingual nerve. It arises deep to the lateral pterygoid muscle, spirals from lateral to medial around the submandibular duct, and divides into several branches that lie in the submucosa of the oral tongue. The special sensory innervation of the oral tongue for taste is provided by the chorda tympani nerve (CN VII) and travels to the anterior tongue with the lingual nerve. In contrast, both functions are performed by the glossopharyngeal nerve for the base of the tongue.
The lymphatic drainage of the oral tongue varies by the region within the tongue. The tip drains preferentially to submental nodes, whereas the lateral tongue drains primarily to levels I and II. However, it is important to note that lymphatic metastasis of lateral tongue lesions directly to the level III/IV nodal group can occur without level I/II spread. The base of the tongue drains to the upper cervical lymphatics. The lack of anastomoses between the anterior lymphatics results in lateralized oral tongue lesions tending to drain ipsilaterally, whereas with base-of-tongue lymphatics, crossover and bilateral cervical lymphatic spread may occur more readily.
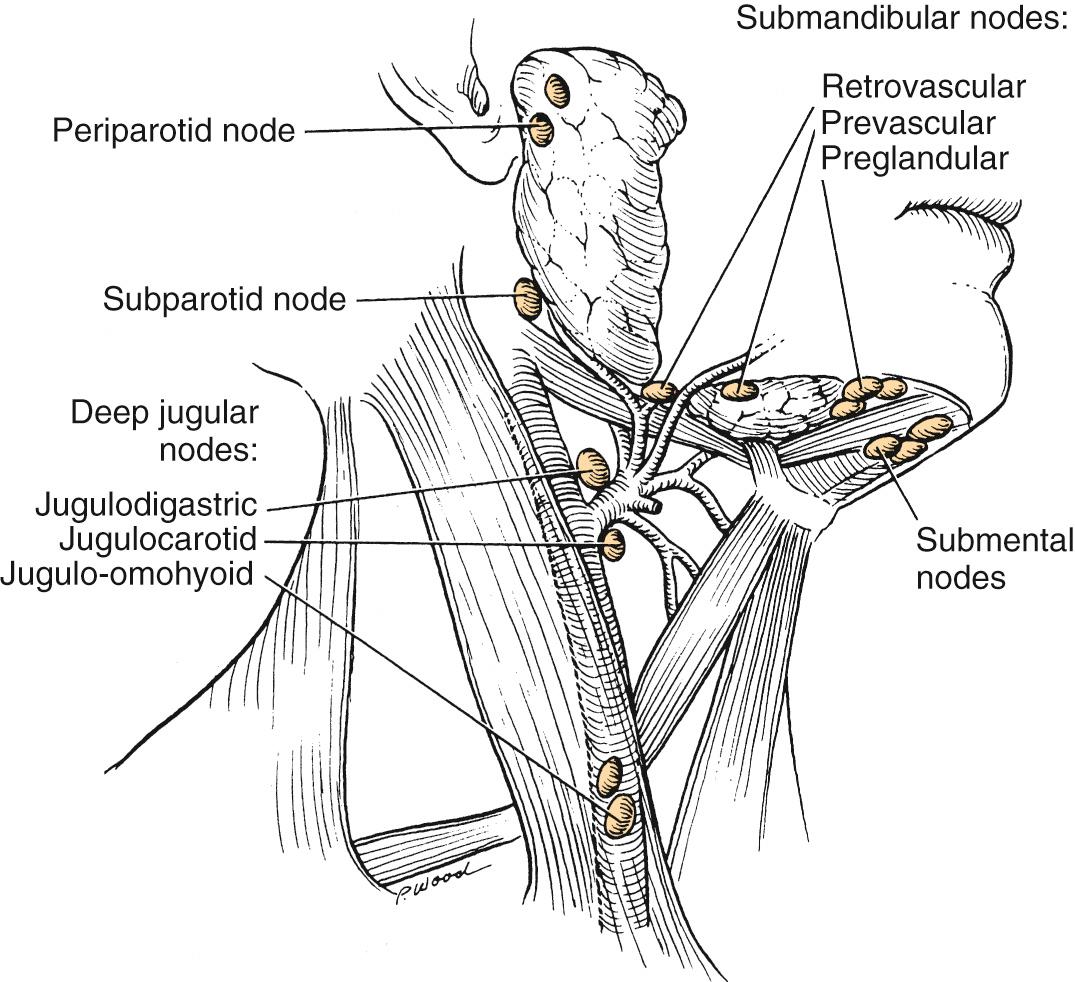
This region is represented by the mucosa that overlies the ascending ramus of the mandible toward the coronoid process. It is continuous with the buccal mucosa laterally and the anterior tonsillar pillar medially. The superior extent is the maxillary tuberosity, and the anterior margin is the posterior aspect of the second mandibular molar. The same considerations that were true for alveolar lesions apply for this anatomic site, given the close approximation of mucosa to the underlying mandible. Lower-lip paresthesia may be an indication of perineural invasion (PNI) at the level of the mandibular foramen with invasive lesions. The sensation to this region is provided by the lesser palatine nerve and branches of the glossopharyngeal nerve. It is the presence of CN IX that causes patients with lesions in this area to present with referred otalgia. The primary lymphatic drainage for this region is to the upper cervical-jugulodigastric nodal group ( Fig. 91.5 ).
The floor of the mouth is a mucosal surface bordered by the oral tongue and alveolar ridge laterally and anteriorly. The posterior margin is the anterior tonsillar pillar, and the lingual frenulum divides the region into two oval spaces. The mylohyoid and hyoglossus muscles provide the structural support for contents of the space. The significance of the floor of the mouth comes from the anatomy that the region overlies. Hypoglossal or lingual nerve dysfunction may be the presenting complaint for patients with lesions in this region. The sublingual gland is also vulnerable to direct invasion. A branch of the lingual nerve provides sensation for the floor of the mouth. The lymphatic drainage of the anterior aspect of this space may cross to contralateral submental-submandibular nodes, whereas the posterior portion of the space tends to drain to ipsilateral upper cervical lymph nodes.
The buccal surface extends from the posterior aspect of the lip to the alveolar ridges medially and to the pterygomandibular raphe posteriorly. The parotid duct orifice is located next to the second maxillary molar, after it exits the parotid and pierces the buccinator muscle. The buccinator muscle represents an important landmark when resecting invasive squamous carcinomas in this region. The sensation is provided by branches of the trigeminal nerve (CN V2 and CN V3). The lymphatics of this region drain preferentially to submental and submandibular lymph nodes.
The hard palate has the maxillary alveolar ridges as anterior and lateral margins and the soft palate as a posterior border. Invasion through the hard palate results in extension of tumor into the nasal cavity or maxillary sinus. Infrastructure maxillectomy is frequently required for invasive lesions, and a prosthetic obturator or flap reconstruction is necessary to reestablish oral competence and avoid hypernasal speech. The nasopalatine nerve (CN V2) provides sensation to the region. Most of the lymphatic drainage from this site is to the upper cervical lymphatics or lateral retropharyngeal nodes.
Certain histopathologic findings can have significant implications for treatment. Tumor thickness, in particular with oral tongue carcinoma, has been shown to have a direct relationship to the incidence of regional metastatic spread and survival. The degree of differentiation and the presence of vascular or PNI have important prognostic implications and may warrant the use of postoperative radiation therapy. The findings of PNI and vascular invasion can be missed with standard hematoxylin-eosin staining. Kurtz and colleagues demonstrated an increase in the identification of these pathologic findings when immunohistochemical staining with S-100 (for PNI) and CD31 (for vascular invasion) is used.
Leukoplakia is a white, mucosal-based keratotic plaque that cannot be wiped free from the underlying tissue. It is a clinical term without a histologic definition. Leukoplakic lesions may demonstrate parakeratosis, hyperkeratosis, and acanthosis on histologic examination. Paradoxically, an increased risk of malignant transformation of leukoplakic lesions is seen more commonly in nonsmokers. If a leukoplakic lesion is associated with an area of dysplasia (in 1% to 3% of all lesions), the risk of progression to malignancy increases sevenfold. Bánóczy followed 670 patients with leukoplakic lesions for 3 years and noted that 31% of lesions disappeared, 30% improved, 25% experienced no change, and 7.5% demonstrated progressive enlargement. Only 6% of lesions in the series underwent subsequent progression to SCC.
Erythroplakia is a red mucosal plaque that does not arise from any obvious mechanical cause and persists after removal of possible etiologic factors. The associated risk for progression to carcinoma is significantly greater than for leukoplakic lesions. Shafer and Waldron resected erythroplakic lesions in 58 patients and found that 91% had evidence of dysplasia (mild, moderate, or severe) or carcinoma in situ within specimens.
Telomere dysfunction is associated with oncogenesis in many cancer types. Short leukocyte telomere length (LTL) in peripheral blood leukocytes has been to found to be associated with the likelihood of progression of normal oral mucosa to premalignancy and subsequent carcinoma. Bau et al. reported on 174 patients with oral premalignant lesions in which LTL was assessed. Of the 23 who eventually progressed to oral carcinoma, the mean LTL of this subgroup was noted as shorter than the “non-progressors.” This finding was noted to be independent of tobacco and alcohol use histories.
The CCND1 gene, located at 11q13, encodes the protein cyclin D1, which is critical to the regulation of the G1 phase of the cell cycle. In a study by Ye and associates, single-nucleotide polymorphism analysis showed a CCND1 P241P polymorphism to be associated with an increased risk of developing oral premalignant lesions when expressed as a variant homozygous genotype. “Ever smokers” with a common homozygote cyclin-dependent kinase 6 (CDK6) genotype and a variant allele–carrying genotype of p27 5′UTR were noted to have the highest percentage of oral premalignant lesion cases (75%) in the study. It is the combination of CDK6/CDK4 and CCND1 that regulates the activity of the RB1 tumor suppressor gene.
OSF is most frequently encountered in individuals who chew betel nut and is associated with poor oral hygiene, advanced periodontitis, and the potential development of oral carcinoma. With betel nut use, the buccal mucosa becomes thickened and the entire cheek becomes fibrotic, which results in trismus. Resection of tumors that arise in the buccal mucosa in patients with submucosal fibrosis can be challenging, and reconstruction can be complicated by wound breakdown. Chaturvedi and colleagues reviewed 371 patients from India with oral cancer, 112 of whom had a history of prior OSF in association with habitual betel nut use. The most common oral cancer subsite was the buccal mucosa in more than 50% of cases, followed by the oral tongue. Patients with oral cancer associated with OSF were typically younger men (mean age, 45.11 years) with better histologic differentiation, lower rates of regional metastasis, and a lower likelihood of extranodal spread when compared with their counterparts who had oral carcinoma without OSF. Patients with a history of betel chewing also require long-term follow-up because of the incidence of multicentric primary tumor presentation and recurrent new primary presentations over time. In a study of 1836 patients in an endemic betel-chewing region the incidence of 2nd, 3rd, and 4th primary oral cavity cancer over a 10-year period was 34.6%, 8.6%, and 2.3%, respectively. In patients with their fourth primary lesion, surgery remained the treatment of choice and offered a 3-year OS of 57%.
Although uncommon, oral lichen planus, in particular the erosive subtype, has the potential for malignant degeneration to oral carcinoma. The etiology of lichen planus is unknown. T-cell lymphocyte infiltration is noted in this lesion, yet the development of lichen planus is not typically associated with immunologic disorders. The typical patient is a female in the fourth decade of life. Lesions demonstrate a lacy pattern of white striae; atrophic lesions are red and smooth, whereas erosive lesions have depressed margins and are covered by a layer of fibrinous exudate.
Dysplasia is the abnormal maturation and differentiation of mucosal epithelium with features of an increased nuclear/cytoplasmic ratio, loss of polarity, increased mitoses, and loss of intercellular adherence. Dysplasia is graded as mild, moderate, or severe. Techniques that have been described to assist in margin assessment at the time of surgery include the use of tissue fluorescence with indocyanine green conjugated to a chlorotoxin (known as BLZ-100). Baik et al. demonstrated that subcutaneous injection of BLZ-100 had good sensitivity (95%) and specificity (91%) in discerning between a tumor and nontumor interface and aiding the identification of high- versus low-risk dysplasia in a hamster dysplasia model.
Several variants of SCC exist and may be encountered in the oral cavity. The spindle cell variant of SCC, also known as sarcomatoid SCC , is typically diagnosed in the oral cavity, oropharynx, or larynx. It demonstrates a heterogeneous appearance with spindle-shaped cells interwoven with squamous cells. The diagnosis of sarcomatoid SCC is confirmed by immunohistochemical staining for keratin markers. It has a high risk of locoregional recurrence; however, OS is similar to that of conventional SCC. Data suggest that this variant of squamous carcinoma may be more responsive to primary surgical management than to chemoradiation.
Basaloid carcinoma has traditionally been considered a high-grade variant with a predilection for regional and distant metastasis; however, when clinical staging is matched, the 5-year DFS associated for oral basaloid carcinoma is similar to that of poorly differentiated and moderately differentiated oral carcinomas.
Radiation-induced squamous cell carcinomas (RISCCs) have reported median latency to development of 13 years. The prognosis is worse than for de novo development of squamous carcinoma yet less likely to be associated with regional metastasis. In a review of 34 cases by Tay et al. from Singapore General Hospital, the oral cavity was the most common site of presentation for RISCC in the head and neck. The 2-year DSS was 48.8% for RISCC versus 71.2% for de novo development of carcinoma.
With verrucous carcinoma, a thick zone of nonproliferation and nonkeratinizing cells distinguishes this entity histologically. The typical presentation is on the buccal mucosa (50%). It is considered a low-grade variant of SCC and is exophytic in appearance, has the capacity to invade locally, yet carries a low risk of regional spread. Traditionally, this lesion has been considered to be “radioresistant,” and surgical excision has been the treatment of choice. Verrucous hyperplasia is a histologic finding that appears similar to verrucous carcinoma yet differs from the malignant form in that it does not invade the lamina propria.
Additional pathologies to consider in the differential diagnosis of oral cavity lesions include pyogenic granuloma, pseudoepitheliomatous hyperplasia, lymphoma, minor salivary gland tumors, and sarcomas.
The most common malignant minor salivary gland tumors (MMSGTs) of the oral cavity are adenoid cystic carcinoma, mucoepidermoid carcinoma (low and high grade), polymorphous low-grade adenocarcinoma, and adenocarcinoma. All of these may present as a painless, slow-growing, submucosal mass at the junction of the hard and soft palate. Adenoid cystic carcinoma can manifest with PNI that can extend within the greater palatine nerve to the pterygopalatine ganglion and can ascend to the skull base.
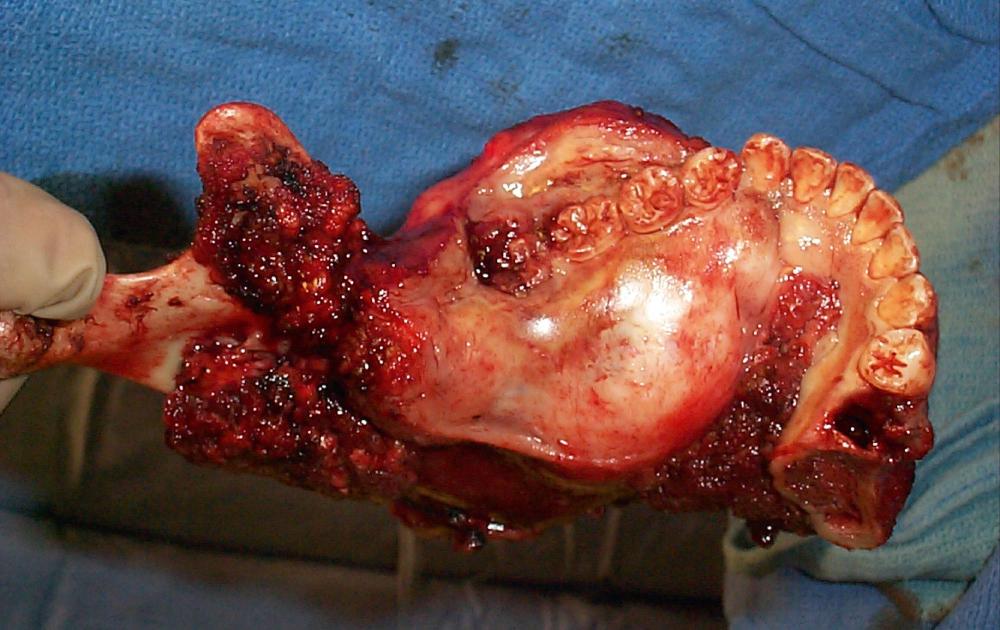
Sarcomas of the oral cavity usually arise in the mandible or hard palate and include osteosarcoma ( Fig. 91.6 ), chondrosarcoma, malignant fibrous histiocytoma, rhabdomyosarcoma, and liposarcoma. Patel and colleagues demonstrated a 5-year local control rate for head and neck osteosarcoma of 78% and OS of 70%. Patients presented with osteosarcoma within the maxilla and mandible with approximately equal frequency, 45% to 41%, respectively. Surgery was performed in all patients and neoadjuvant chemotherapy was used in 68%. Positive surgical margins were found to be the only significant negative predictor with respect to DSS.
Malignant tumors of odontogenic origin, although uncommon, can present a challenge for diagnosis and treatment. Agar et al. performed a SEER database review from 1973 to 2011 and identified 308 cases. Of the three main categories of lesion, malignant ameloblastoma was the most common (59.7%), followed by malignant odontogenic tumors (35.4%) and ameloblastic fibrosarcoma (2.9%). The 5-year survival for the entire cohort of patients was 81% with patients diagnosed with malignant ameloblastoma having the best mean survival (237 months). Malignant odontogenic tumors encompassed a group of diagnoses including odontogenic carcinoma, primary intraosseous carcinoma, odontogenic sarcoma, and ameloblastic carcinoma. For all lesion types, patients with tumors that were 41 mm or greater in size experienced the lowest survival rate.
Typically presenting in children, Ewing sarcoma has a 1% to 2% incidence of presentation in the facial skeleton. The most common site of diagnosis in the mandible is at the ramus. Treatment typically entails wide surgical excision in combination with chemotherapy. If possible, radiation is avoided to minimize the impact on subsequent facial growth.
Kaposi sarcoma is the most common HIV-associated malignancy. The head and neck is the site for two-thirds of all presentations and may present as a pigmented mucosal nodule and is most commonly seen on the hard palate. Despite being considered an incurable disorder, a variety of treatment options may offer remission for limited disease. Local therapies include radiation, intralesional injection of chemotherapy, cryotherapy, laser therapy, and surgical excision. Systemic chemotherapy is reserved for advanced disease.
Desmoplastic neurotrophic melanoma is a nonpigmented lesion of the lower lip that presents as an ulceration and has a high incidence for PNI. Mucosal melanoma typically presents as a pigmented lesion of the oral cavity that may be associated with preexisting melanosis. Pigmented lesions of the oral cavity should be considered for biopsy to exclude this diagnosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here