Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Metastatic squamous cell carcinoma (SCC) in the neck often presents without a clinically apparent primary. The majority of cases of metastatic SCC to cervical lymph nodes are associated with high-risk human papillomavirus (HPV) from the oropharynx (base of tongue and tonsil), although conventional SCC from the upper aerodigestive tract is also common. The rich lymphatic plexus in the oropharynx can lead to early metastatic disease via the jugulodigastric lymph node chain, even for small and clinically inapparent primary tumors. Furthermore, tumors that involve the tonsils and tongue base will frequently localize to deep crypt locations, with little evidence for surface mucosal alterations. Metastatic SCC is often cystic, which may pose certain diagnostic difficulties, especially in younger patients.
Rarely, specific variants of SCC must be considered in the neck, such as nasopharyngeal carcinoma (which is associated with Epstein-Barr virus [EBV]) and NUT carcinoma (characterized by NUT M1 gene rearrangement), the latter representing an extremely aggressive subtype.
Patients most frequently present with a short history (< 6 months) of a painless mass in the upper neck involving the jugulodigastric lymph nodes. Patients may have bilateral disease (10%). There may be a history of smoking and/or alcohol abuse, especially in the context of conventional SCC. Most patients present during the 6th decade of life, with a strong male predilection (4 : 1). After the diagnosis of metastatic SCC is established, a primary tumor is discovered in at least 80% of patients, with the majority located in the oropharynx. Other primary sites can include the nasopharynx, oral cavity, esophagus, and laryngotracheal region. In up to 10% of patients a primary is never found, despite an extensive workup.
SCC that has metastasized to cervical lymph nodes
Approximately one-third of cervical metastatic SCCs are cystic
Many are from an oropharyngeal primary and are associated with high-risk HPV
Primary oropharyngeal HPV-associated SCC may be occult and small
Mucositis and xerostomia (secondary to radiotherapy and/or chemotherapy)
Approximately 30% mortality at 5 years
Males > > females (4 : 1)
Mean presentation in 6th decade
Painless mass involving jugulodigastric lymph nodes
Usually short duration (<6 months)
May have bilateral disease (10%)
Often have smoking and alcohol abuse history
Once metastatic disease is diagnosed, nearly 70% will have an oropharyngeal primary
70%-80% 5-year survival
Identification of the primary may require extensive examination under anesthesia, pan-endoscopy, high-resolution radiographic studies, and/or ipsilateral tonsillectomy
Selected lymphadenectomy (used to make diagnosis) followed by focused radiation therapy (targeted to primary or Waldeyer ring if no primary is identified)
HPV, Human papillomavirus; SCC, squamous cell carcinoma.
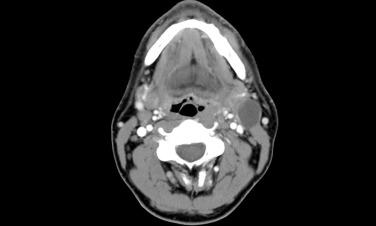
Computed tomography (CT) or magnetic resonance imaging (MRI) shows a cystic or multilocular mass with a thick capsule in the region of the jugulodigastric lymph nodes ( Fig. 22.1 ).
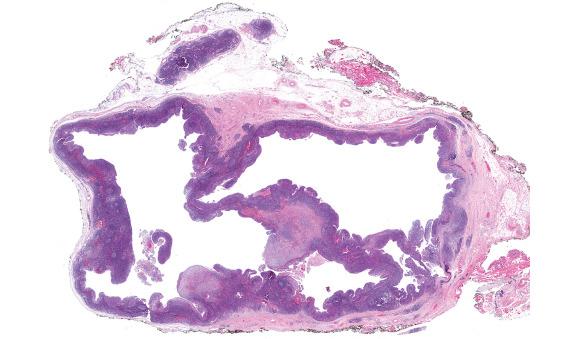
The metastatic lesions can range in size from 1.5 to 12 cm (average size of approximately 4 cm). There is often a thick, fibrotic capsule defining the well-circumscribed lymph node border. Tumors with extracapsular extension have irregular borders and infiltration into adjacent fibroadipose tissue or skeletal muscle. Matted lymph nodes of confluent metastases may be seen. The cut surface is unilocular or multilocular, with cyst(s) filled with granular, thick, tenacious, and purulent yellow-brown to hemorrhagic fluid.
Typically well-circumscribed, thickly encapsulated cystic mass
Thick, tenacious, purulent, yellow-brown to hemorrhagic fluid
Mean size of 4 cm (but may be large, up to 12 cm)
Thick, desmoplastic fibrous capsule
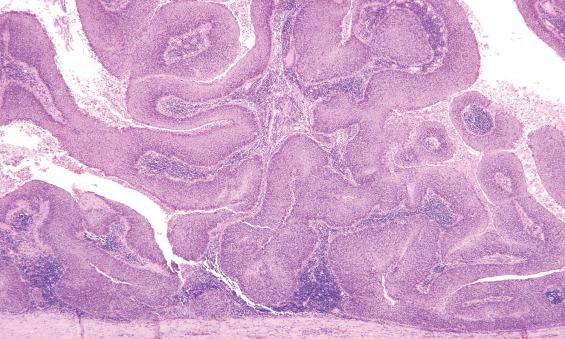
Metastases are often cystic, with cyst spaces lined by ribbon-like growth of malignant squamous cells
Conventional SCC may be well, moderately, or poorly differentiated with varying degrees of keratinization and atypia
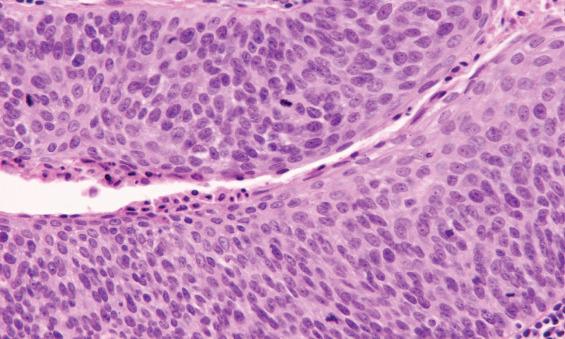
HPV-SCC appears nonkeratizining, with trabecular and ribbon-like growth of uniform squamous cells lacking maturation that demonstrate loss of polarity, high nuclear to cytoplasmic ratio, and mitotic figures; profound pleomorphism is typically absent
Extranodal extension should be noted
Keratins and p63/p40 are positive, but usually not necessary for diagnosis
Diffuse p16 nuclear positivity is an excellent surrogate marker of high-risk HPV
High-risk HPV can be detected by ISH or sequencing
Nasopharyngeal carcinoma is positive for EBV (best detected by ISH)
NUT carcinoma shows punctate nuclear staining for NUT immunohistochemistry
Cellular smears
Anucleate squames and debris
Atypical squamous cells with dyskeratosis, irregular nuclear contours, nuclear hyperchromasia, and increased nuclear to cytoplasmic ratio
Branchial cleft cyst, thymopharyngeal cyst, thymic cyst, bronchial cyst
Pilomatricoma
High-grade mucoepidermoid carcinoma
EBV, Epstein-Barr virus; HPV, human papillomavirus; ISH, in situ hybridization; SCC, squamous cell carcinoma.
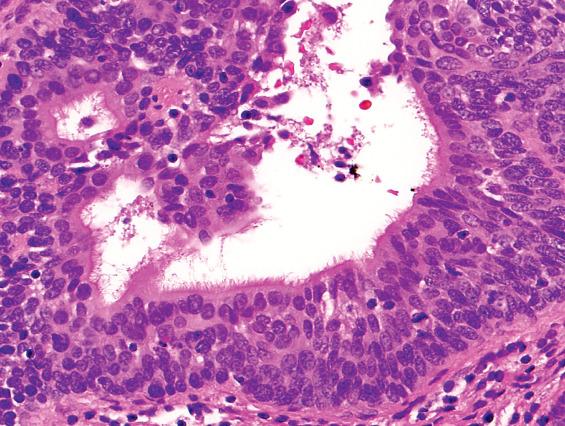
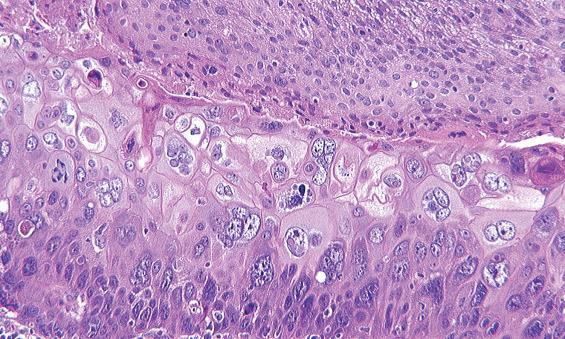
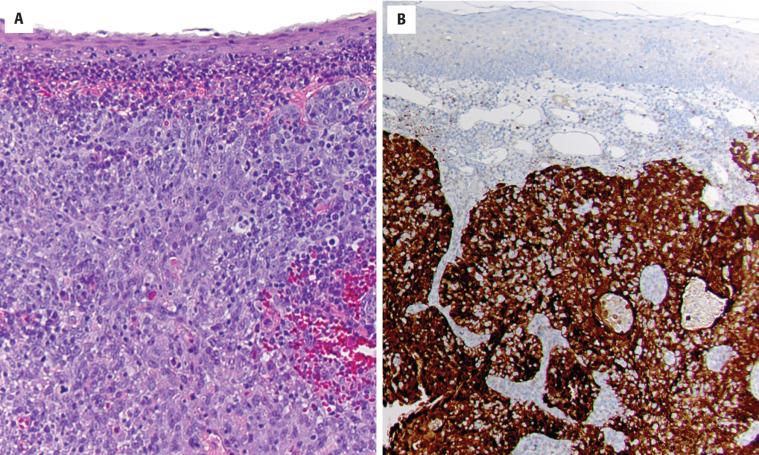
On microscopic examination, a dense, fibrous connective tissue capsule will often surround the lymph node that contains metastatic tumor ( Fig. 22.2 ). The cystic spaces are lined by a ribbon-like growth of squamous epithelium, which has a generally uniform thickness ( Fig. 22.3 ). Metastatic SCC can vary in appearance, ranging from transitional, basaloid, and nonkeratinizing morphology to a more conventional keratinizing squamous appearance. In some areas, metastatic tumor has an endophytic growth pattern, budding into the lymphoid stroma, whereas in other areas it is exophytic or papillary, with projections into the cyst spaces. The cyst contents are often washed away during fixation and histologic processing, leaving these variably sized spaces largely empty. For metastatic oropharyngeal HPV-related squamous cell carcinoma (HPV-SCC) in particular, the overall histologic appearance may be somewhat bland, recapitulating the normal squamous or transitional-type epithelium that is present in a normal deep tonsillar crypt ( Fig. 22.4 ). In exceptional cases of metastatic HPV-SCC, the tumor cells even retain cilia, an extremely rare finding in malignant neoplasms ( Fig. 22.5 ). Nonetheless, the cells are enlarged with a high nuclear to cytoplasmic ratio, no appreciable degree of surface maturation, and limited keratinization. Occasionally, an abrupt transition to remarkably atypical epithelium can be seen, facilitating the diagnosis ( Fig. 22.6 ). Because of the often bland histologic appearance on initial low-power examination, these lesions may require careful inspection to make the correct diagnosis. Notably, extranodular extension should be noted although for oropharyngeal HPV-associated primaries, it may not be associated with prognosis.
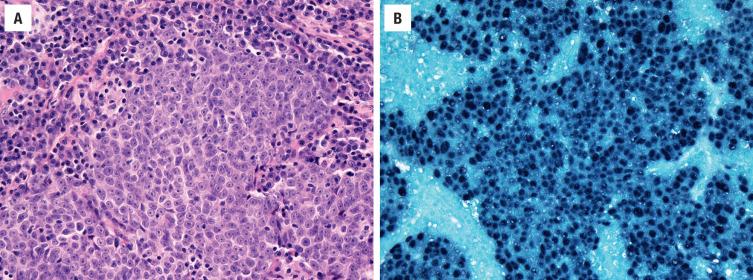
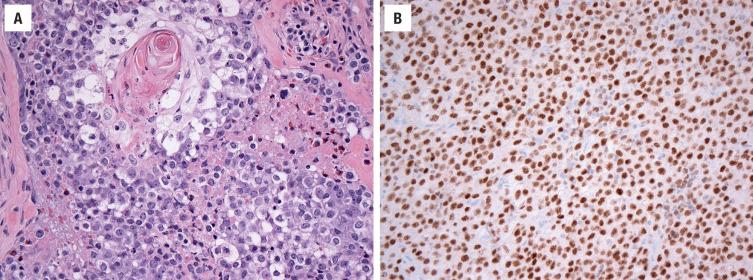
Specific rare variants of SCC that are nonkeratinizing or primitive appearing may need to be considered in the absence of HPV. Nasopharyngeal carcinoma is associated with a dense lymphocytic infiltrate (but may appear indistinct from normal lymph node), and tumor cells often have large vesicular nuclei and prominent nucleoli ( Fig. 22.7 ). NUT carcinoma is composed predominantly of a uniform undifferentiated epithelioid morphology, but careful histologic examination will usually identify abrupt small foci of keratinization ( Fig. 22.8 ).
Immunohistochemistry is often not necessary for the recognition of SCC. However, tumor cells are positive with a variety of keratins (AE1/AE3, CK5, CK8, CK14, and CK19), although CK7 is usually negative. Squamous differentiation can be identified by p63 and its more squamous-specific isoform, p40, which is helpful for poorly differentiated tumors.
Given the high frequency (70%) of patients with HPV-SCC who present with cervical lymph node metastases, all cases of metastatic SCC in the neck should undergo testing for high-risk HPV. p16 is an excellent immunohistochemical surrogate marker for high-risk HPV; to be regarded as positive, nuclear and cytoplasmic staining should be present in at least 70% of tumor cells ( Fig. 22.9 ). The detection of HPV is helpful in localizing the primary oropharyngeal site but also has clinical implications given that HPV-SCC is associated with better outcomes in comparison to conventional SCC.
In most cases, p16 positivity is sufficient for identifying HPV-SCC if the histologic features (i.e., nonkeratinizing morphology) and clinical context (i.e., level 2 or 3 lymph node, oropharyngeal or unknown primary) are typical. However, there are more pitfalls in the interpretation of p16 in the neck than in the oropharynx because metastatic lung and skin carcinomas and even benign cysts can be p16 positive. For that reason, many laboratories follow positive p16 staining with confirmatory HPV detection by a more specific technique. High-risk HPV can be detected via in situ hybridization (ISH) or through amplification detection via sequencing. ISH has the advantage of assessing cellular location, which distinguishes between episomal and integrated virus by two distinct staining patterns: punctate (dot-like) staining with integrated virus and diffuse nuclear staining with episomal virus ( Fig. 22.10 ).
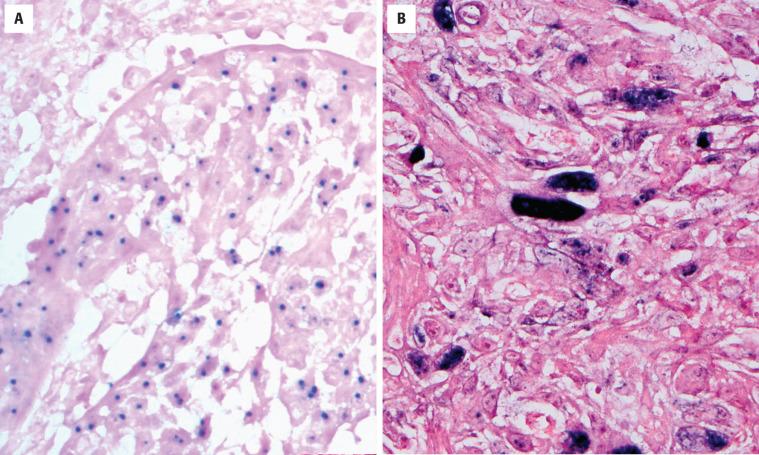
EBV can be detected in nasopharyngeal carcinoma by ISH ( Fig. 22.7 ). NUT carcinoma will show punctate nuclear immunoreactivity for NUT ( Fig. 22.8 ); NUTM1 rearrangements can be detected using fluorescence in situ hybridization (FISH) break-apart probe for the NUT locus on 15q14 or by sequencing the NUT-BRD4 fusion gene.
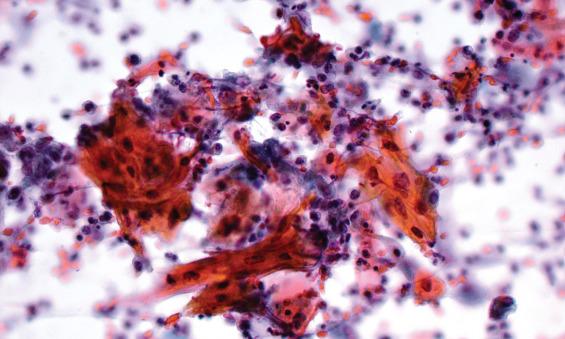
Aspirate smears of metastatic SCC are often quite cellular and, in many cases, dominated by anucleate squamous and debris from the cyst contents. Fragments of atypical squamous epithelium are often present, as well as individual atypical keratinocytes ( Fig. 22.11 ). Nuclear atypia, pleomorphism, increased nuclear to cytoplasmic ratio, and mitotic figures all help to confirm the diagnosis. All cytologic specimens, especially with cell block material of metastatic SCC should be assessed for high-risk HPV, and if initially negative, studies should be repeated on any subsequent surgical specimens. Notably, p16 immunostaining is less consistently strong and diffuse in cytology material than it is in tissue specimens.
Especially in younger patients, cystic, metastatic SCC must be distinguished from a branchial cleft cyst. Branchial cleft cysts will usually not have a thickened or desmoplastic capsule and will often contain clear fluid. The epithelium in branchial cleft cyst may be variable, with areas of respiratory epithelium and squamous epithelium, which can show keratinization; however, frank atypia is absent. Immunoreactivity for p16 may be seen in the epithelium of branchial cleft cysts but is usually limited to areas infiltrated by inflammatory cells. Ciliated HPV-related carcinomas are particularly treacherous as the presence of cilia in a lateral neck cyst is sometimes presumed to be diagnostic of a branchial cleft cyst. Using an HPV-specific testing such as ISH will resolve this diagnostic dilemma. Other benign developmental cystic lesions that may enter the differential include thymopharyngeal cyst, thymic cyst, and bronchial cyst, which can be identified by the presence of thymic or respiratory components.
Pilomatricomas are another diagnostic pitfall, especially for HPV-SCC. Pilomatricoma is characterized by a monomorphous basaloid cell population and abundant “ghost” cells (anucleate squames with pale central zone) admixed with keratin. An adjacent inflammatory infiltrate and giant cell reaction and large dystrophic calcifications are common in pilomatricoma, but these features may also be seen as reactive changes to metastatic SCC. Pilomatricomas are more likely in younger patients and show a female predominance. The absence of cytologic atypia favors pilomatricoma; SCC should be considered if there is significant pleomorphism, hyperchromatic nuclei with prominent nucleoli, and significant mitotic activity with atypical forms.
Metastatic salivary gland neoplasms may need to be considered, namely high-grade mucoepidermoid carcinoma, as well as salivary duct carcinoma and carcinoma ex pleomorphic adenoma. High-grade mucoepidermoid carcinoma shows a predominance of the squamoid cells and limited cyst formation and absence or paucity of mucocytes. Careful histologic examination is necessary to find focal glandular differentiation, which may be visualized by mucicarmine special stain. Genetic testing may be helpful because mucoepidermoid carcinoma harbors recurrent MECT1-MAML2 fusion gene (or rarely alternate CRCT3-MAML2 ). Salivary duct carcinoma has foci resembling high-grade in situ ductal carcinoma of breast. Most salivary duct carcinomas are positive for androgen receptor, and a subset show membranous expression of Her2/neu (30%). Carcinoma ex pleomorphic adenoma (including salivary duct carcinoma ex pleomorphic adenoma) often shows cytologic and architectural heterogeneity and a myoepithelial immunophenotype, and the subsets arising from a precursor harboring either PLAG1 or HMGA2 rearrangement will show overexpression of the corresponding protein.
After the diagnosis of metastatic SCC is accurately classified, efforts toward identifying the primary tumor are typically undertaken and include extensive physical examination under anesthesia, pan-endoscopy (nasopharynx, larynx, esophagus, nasal cavity), and detailed, high-resolution CT or MRI studies of the oropharynx and Waldeyer ring area. Again, this search is informed by initial assessment of the metastatic lesion for the presence of high-risk HPV. If these studies do not identify the primary, then prophylactic lingual and palatine tonsillectomy, specifically on the ipsilateral side, should be performed, with complete embedding of the tonsils and thorough sectioning. Still, attempts at identifying the primary tumor will be defied in an appreciable proportion of patients (up to 10%). Radiation therapy in the region of Waldeyer ring, after selected lymph node dissection, will yield a good long-term clinical outcome of 70% to 80% survival at 5 years. Patients with HPV-SCC may be managed with intensity-modulated or brachy-radiation treatment. Concurrent radiation and multiagent chemotherapy may be used. A common complication of radiotherapy or chemotherapy is mucositis and xerostomia. Overall, HPV-SCC are associated with a better outcome (up to 80% 5-year survival, stage dependent) in comparison to conventional SCC of the upper aerodigestive tract (survival rates of <35% at 5 years).
The term “occult primary tumor” refers to a primary neoplasm that has not been found in a patient with lymph node, organ, or soft tissue metastasis, even after thorough clinical evaluation. Evaluation includes pan-endoscopy, radiographic studies, and serologic markers. A fine needle aspiration (FNA) or core needle biopsy is frequently the initial procedure. Neck metastasis may represent disease from a regional or distant primary neoplasm. Despite aggressive assessment, in up to 10% of patients, a primary tumor will not be identified. Axiomatic, lymphomas must always be excluded because their management is unique from that of metastatic carcinoma.
The most common symptom is a painless mass in the neck. The most frequent sites of adenopathy are upper jugulodigastric (70%), midjugular (22%), supraclavicular (18%), and posterior cervical lymph nodes (12%), frequently with more than one site affected. The mass may be present for quite some time and is often slowly enlarging. The mean age at presentation is in the 6th decade, although this depends on the primary tumor type. When the primaries are from the upper aerodigestive system or salivary gland, men are affected more commonly than women (4 : 1), with many patients reporting a history of heavy smoking and drinking. Non–head and non-neck carcinoma primary sites include melanoma, lung, gastrointestinal tract, breast, pancreas, ovary, kidney, prostate, and less rarely sarcomas.
An unidentified primary neoplasm with cervical metastasis
Neck lymph node metastasis is frequent
Upper jugular lymph nodes account for site of most metastatic tumors (70%)
Mortality depends on primary tumor
For upper aerodigestive tract and salivary primaries, males > > females (4 : 1)
Usually adults, with a mean presentation in the 6th decade
Other primaries are sex and age specific
Painless cervical mass
Slow growing over several months
Primary sites include oropharynx, nasopharynx, larynx, and esophagus; and lung, gastrointestinal tract, breast, pancreas, and prostate account for carcinomas outside of the head and neck region
Melanoma and sarcoma also present as metastatic tumors
For a subset of patients (up to 10%), no known primary is identified after thorough work-up
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here