Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Defense against infectious agents is secured through a combination of anatomic physical barriers, including the skin, mucous membranes, mucous blanket, and ciliated epithelial cells, and the components of the immune system. The immune system of vertebrates integrates 2 fundamental response mechanisms. Innate (natural) immunity is rapid and utilizes receptors encoded in the germline. The innate defenses comprise cell-intrinsic responses to viral infections, leukocyte responses to pathogens, and soluble mediators such as complement proteins. Acquired (adaptive) immunity is specific to T and B cells. These cells undergo DNA recombination to generate receptors and require an education process to minimize autoreactive cells. In addition, there are lymphocyte subsets that are innate in nature and either do not require DNA recombination or utilize a single recombination event to generate a monospecific receptor.
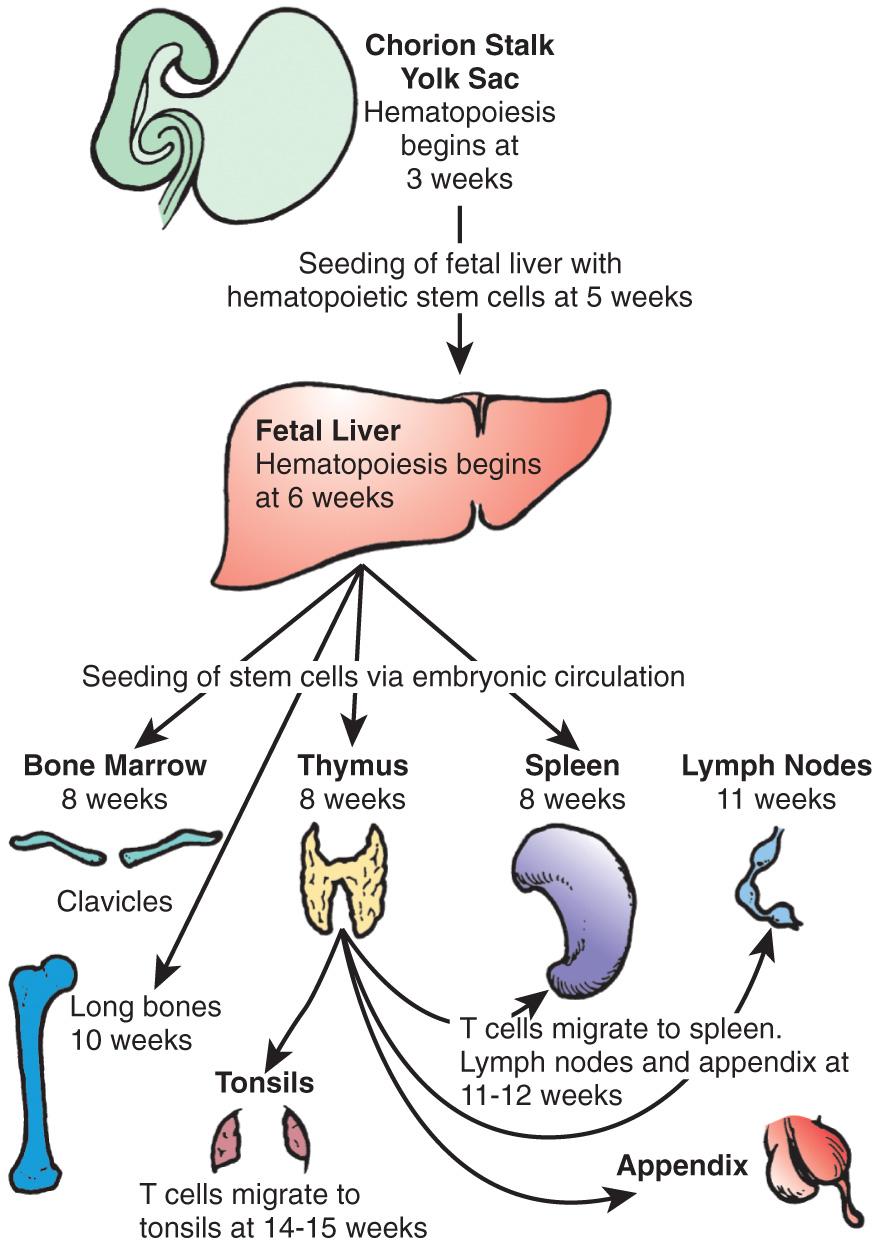
Pluripotential hematopoietic stem cells first appear in the yolk sac at 2.5-3 wk of gestational age, migrate to the fetal liver at 5 wk gestation, and later reside in the bone marrow, where they remain throughout life ( Fig. 149.1 ). Lymphoid stem cells develop and differentiate into T, B, or natural killer (NK) cells, depending on the organs or tissues to which the stem cells traffic. Development of the primary lymphoid organs —thymus and bone marrow—begins during the middle of the 1st trimester of gestation and proceeds rapidly. Development of the secondary lymphoid organs —spleen, lymph nodes, tonsils, Peyer patches, and lamina propria—soon follows. These organs serve as sites of differentiation of T, B, and NK lymphocytes from stem cells throughout life. Both the initial organogenesis and the continued cell differentiation result from the interaction of a vast array of lymphocytic and microenvironmental cell surface molecules and proteins secreted by the involved cells. Clusters of differentiation (CD) refer to cellular protein ( Table 149.1 ), whereas cytokines and chemokines refer to soluble mediators of immune function ( Table 149.2 ).
| CD NUMBER | TISSUE/LINEAGE | FUNCTION |
|---|---|---|
| CD1 | Cortical thymocytes; Langerhans cells | Lipid antigen presentation to TCRγδ cells |
| CD2 | T and NK cells | Binds LFA-3 (CD58); alternative pathway of T-cell activation |
| CD3 | T cells | TCR associated; transduces signals from TCR |
| CD4 | T-helper cell subset | Receptor for HLA class II antigens; associated with p56 Ick tyrosine kinase |
| CD7 | T and NK cells and their precursors | Mitogenic for T lymphocytes |
| CD8 | Cytotoxic T-cell subset; also on 30% of NK cells | Receptor for HLA class I antigens; associated with p56 Ick tyrosine kinase |
| CD10 | B-cell progenitors | Peptide cleavage |
| CD11a | T, B, and NK cells | With CD18, ligand for ICAMs 1, 2, and 3 |
| CD11b, c | NK cells | With CD18, receptors for C3bi |
| CD16 | NK cells | FcR for IgG |
| CD19 | B cells | Regulates B-cell activation |
| CD20 | B cells | Mediates B-cell activation |
| CD21 | B cells | C3d, also the receptor for EBV; CR2 |
| CD25 | T, B, and NK cells | Mediates signaling by IL-2 |
| CD34 | Stem cells | Binds to l -selectin |
| CD38 | T, B, and NK cells and monocytes | Associates with hyaluronic acid |
| CD40 | B cells and monocytes | Initiates isotype switching in B cells when ligated |
| CD44 | Bone marrow stromal and many other cells | Matrix adhesion molecule |
| CD45 | All leukocytes | Tyrosine phosphatase that regulates lymphocyte activation; CD45R0 isoform on memory T cells, CD45RA isoform on naïve T cells |
| CD56 | NK cells | Mediates NK homotypic adhesion |
| CD62L | Marker for recent thymic emigrants Also found on other leukocytes |
Cell adhesion molecule |
| CD69 | T cells and NK cells | Early activation marker |
| CD73 | T and B cells | Associates with AMP |
| CD80 | B cells | Co-stimulatory with CD28 on T cells to upregulate high-affinity IL-2 receptor |
| CD86 | B cells | Co-stimulatory with CD28 on T cells to upregulate high-affinity IL-2 receptor |
| CD117 | Pro-B cells, double-negative thymocytes | Receptor for stem cell factor |
| CD127 | T cells | Mediates IL-7 signaling |
| CD132 | T, B, and NK cells | Mediates signaling by IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21 |
| CD154 | Activated CD4 + T cells | Ligates CD40 on B cells and initiates isotype switching |
| CD278 | T cells | Interacts with B7-H2 |
| CATEGORY | CYTOKINE | FUNCTION |
|---|---|---|
| Interferons | IFN-α | Antiviral defense |
| IFN-β | Antiviral defense | |
| IFN-γ | Antiviral defense | |
| Innate responses | TNF | Regulates endothelial adhesion molecules for recruitment of neutrophils; activates macrophages for killing |
| IL-1β | Drives the inflammatory response, fever | |
| IL-12 | Polarizes T cells toward Th1; activates NK cells | |
| Lymphocyte regulation | IL-2 | Key growth factor for T cells |
| IL-4 | Polarizes T cells toward Th2 | |
| IL-6 | Growth factor for B cells | |
| IL-7 | T-cell homeostatic factor | |
| IL-10 | Growth factor for B cells, immunosuppressive | |
| IL-12 | Polarizes T cells toward Th1, activates NK cells | |
| IL-17 | Polarizes T cells toward Th17, stimulates antimicrobial peptide expression | |
| IL-21 | Supports B-cell class switching |
The primitive thymic rudiment is formed from the ectoderm of the 3rd branchial cleft and endoderm of the 3rd branchial pouch at 4 wk gestation. Beginning at 7-8 wk, the right and left rudiments fuse in the midline. Bloodborne T-cell precursors from the fetal liver then begin to colonize the perithymic mesenchyme at 8 wk gestation and move into the thymus at 8.0-8.5 wk. The earliest cells to enter the thymus are found in the subcapsular region and do not express CD3, CD4, CD8, or either type of T-cell receptor (TCR). These lymphoid cell precursors are triggered to proliferate and become thymocytes through interactions with the thymic stroma. The cells are arrested at this stage until they productively rearrange the β-chain locus of the TCR. The β chain then pairs with the surrogate pre-T α chain. This tests the function of the β chain, and if signaling occurs, β-chain rearrangement ceases. CD4 and CD8 are then expressed simultaneously (i.e., they are double-positive thymocytes). Fetal cortical thymocytes are among the most rapidly dividing cells in the body and increase in number by 100,000-fold within 2 wk after stem cells enter the thymus. As these cells proliferate and mature, they migrate deeper into the thymic cortex. The double-positive thymocytes begin efficient rearrangement of the α-chain locus. TCR gene rearrangement occurs by a process in which large, noncontiguous blocks of DNA are spliced together. V (variable) , D (diversity) , and J (joining) blocks exist in families of minimally different segments. Random combinations of the segments account for much of the enormous diversity of TCRs that enables humans to recognize millions of different antigens. TCR gene rearrangement requires the presence of recombinase-activating genes , RAG1 and RAG2, as well as other recombinase components.
As immature cortical thymocytes begin to express TCRs, the processes of positive and negative selection take place. Positive selection occurs in immature thymocytes, recognizing major histocompatibility complex (MHC) antigens present on cortical thymic epithelial cells. Some cells are selected to mature into CD4 or CD8 single-positive cells. Negative selection occurs next in the thymic medulla on medullary thymic epithelial cells. Autoreactive T cells undergo apoptosis and die. T cells begin to emigrate from the thymus to the spleen, lymph nodes, and appendix at 11-12 wk of embryonic life and to the tonsils by 14-15 wk. They leave the thymus via the bloodstream and are distributed throughout the body, with the heaviest concentrations in the paracortical areas of lymph nodes, the periarteriolar areas of the spleen, and the thoracic lymph duct. Recent thymic emigrants co-express the CD45RA isoforms and CD62L ( l -selectin).
Rearrangement of the TCR locus during intrathymic T-cell development results in the excision of DNA and the excised elements form circular episomes as a by-product. These TCR recombination excision circles can be detected in T cells that are recent thymic emigrants. TCR recombination excision circles detected in dried-blood spots collected from infants shortly after birth is the test used for newborn screening for severe combined immunodeficiency (SCID). By 12 wk gestation, T cells can proliferate in response to plant lectins, such as phytohemagglutinin and concanavalin A. Antigen-specific T cells have been found by 20 wk gestation. Hassall corpuscles (bodies), which are swirls of terminally differentiated medullary epithelial cells, are first seen in the thymic medulla at 16-18 wk of embryonic life.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here