Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term thorax refers to the area between the neck and abdomen enclosed by the ribs, sternum, and vertebrae radially, the thoracic inlet superiorly, and the diaphragm inferiorly. The chest or thorax supports and protects the internal thoracic organs, provides for the negative inspiratory force that initiates ventilation and the positive expiratory force needed for vocalization, and creates a frame for the neck, upper extremities, thoracic structures, and abdomen. The major thoracic structures include the heart and lungs, chest wall—including the overlying musculature, ribs, sternum, and vertebrae—diaphragm, trachea, esophagus, and great vessels.
The thoracic organs are protected by the bony thorax and overlying chest musculature. The parietal pleura, the internal lining of the chest wall, is separated from the visceral pleura, the outer lining of the lung, by a small amount of pleural fluid. The parietal pleura covers the chest wall, mediastinum, diaphragm, and pericardium. The visceral pleura covers the lung and separates the lobes from one another. The pleural space is a potential space that may compress the lungs or heart with fluid, tumor, or infection. The right and left pleural spaces are separated from one another by the mediastinum.
The bony thorax is covered by three groups of muscles: the primary and secondary muscles for respiration and the muscles attaching the upper extremity to the body ( Fig. 58.1 ). The primary muscles include the diaphragm and intercostal muscles. The intercostal muscles of the intercostal spaces include the external, internal, and transverse or innermost muscles. The 11 intercostal spaces, each associated numerically with the rib superior to it, contain the intercostal bundles (vein, artery, and nerve) that travel along the lower edge of each rib. All intercostal spaces are wider anteriorly, and each intercostal bundle falls away from the rib posteriorly to become more centrally located within each space. The intercostal muscle layers assist with respiration and protect the thoracic structures. The extrinsic muscles of the chest, latissimus dorsi muscle, serratus anterior muscle, pectoralis major and minor muscles, and cervical muscles (sternocleidomastoid, scalene muscles) attach to the bony thorax, protect the chest wall itself, and may assist with ventilatory efforts in patients with chronic obstructive pulmonary disease (COPD).

The secondary muscles consist of the sternocleidomastoid, serratus posterior, and levatores costarum. The third muscle group attaches the upper extremity to the body. The pectoralis major and minor muscles lie anteriorly and superficially. Posterior superficial musculature includes the trapezius and latissimus dorsi. Deep muscles include the serratus anterior and posterior, the levatores, and the major and minor rhomboids. These superficial and deep muscles help to hold the scapulae to the chest wall. In respiratory distress, the deltoid, pectoralis, and latissimus dorsi muscles form a tertiary system for ventilatory assistance through fixation of the upper extremities.
The bony thorax consists of 12 ribs peripherally extending from the vertebrae posteromedially to the sternum or costal arch anteriorly ( Fig. 58.2 ). The 11th and 12th ribs are “floating ribs” and are not attached directly to the sternum. Ribs 1 to 5 are directly attached to the sternum by costal cartilages. The lower ribs (6–10) coalesce into the costal arch. The first rib is relatively flat and dense and travels from the first thoracic vertebra to the manubrium to create the thoracic inlet ( Fig. 58.3 ). Through this relatively small area pass the great vessels, trachea, esophagus, and innervation to the upper extremity, diaphragm, and larynx. Trauma to this area, manifested by a first rib fracture, is the consequence of a significant mechanical force with likelihood of injury to one or more of these structures. Other structures within the thoracic inlet include the phrenic nerve, the recurrent laryngeal nerve in the tracheoesophageal groove (which recurs around the aorta at the ligamentum arteriosum on the left and around the innominate artery on the right), and the insertion of the thoracic duct posteriorly at the junction of the left subclavian with the left internal jugular veins. The remaining ribs gradually slope downward. Each rib is composed of a head, neck, and shaft. Each head has an upper facet, which articulates with the vertebral body above it, and a lower facet, which articulates with the corresponding thoracic vertebra to that rib, establishing the costovertebral joint. The neck of the rib has a tubercle with an articular facet; this articulates with the transverse process, creating the costotransverse joint and imparting strength to the posterior rib cage.


The sternum is flat, 15 to 20 cm long and approximately 1.0 to 1.5 cm thick, and comprises the manubrium, body, and xiphoid. The manubrium articulates with each clavicle and the first rib. The manubrium joins the body of the sternum at the angle of Louis, which corresponds to the anterior aspect of the junction of the second rib. The angle of Louis is a superficial anatomic landmark for the level of the carina. The anterior cartilaginous attachments of the true ribs to the sternum, along with intercostal muscles and the hemidiaphragms, allow for movement of the ribs with respiration.
The trachea in adults is approximately 12 cm long with 18 to 22 cartilaginous rings. The internal diameter is 2.3 cm laterally and 1.8 cm anteroposteriorly. The larynx ends with the inferior edge of cricoid cartilage. The cricoid is the only complete cartilaginous ring in the trachea. The trachea begins approximately 1.5 cm below the vocal cords and is not rigidly fixed to surrounding tissues. Vertical movement is easily possible. The most rigid point of fixation is where the aortic arch forms a sling over the left mainstem bronchus. The innominate artery crosses over the anterior trachea in a left inferolateral to high right anterolateral direction. The azygos vein arches over the proximal right mainstem bronchus as it travels from posterior to anterior to empty into the superior vena cava. The esophagus is closely applied to the membranous trachea and lies to the left of the midline of the trachea. The recurrent laryngeal nerves run in the tracheoesophageal groove on both the right and the left. The blood supply to the trachea is lateral and segmental from the inferior thyroid, the internal thoracic, the supreme intercostal, and the bronchial arteries. During trachea reconstruction, circumferential dissection greater than 1 to 2 cm may lead to vascular insufficiency with necrosis or anastomotic dehiscence.
Lung development begins at approximately 21 to 28 days’ gestation. The true alveolar stage, with air sacs surrounded on all sides by capillaries, occurs from approximately 7 months to term. Alveolar proliferation continues after birth. There are approximately 20 million alveoli at birth, which increase to approximately 300 million by age 10 years, with no more increase after that time. There are 23 generations of bronchi between the trachea and terminal alveoli. Air accounts for 80% of the lung volume, blood accounts for 10%, and solid tissue accounts for approximately 10%. Alveoli make up approximately half of the entire lung volume.
The lungs are broadly divided into five lobes and multiple segments within each lobe ( Fig. 58.4 ). The right lung is composed of three lobes: upper, middle, and lower. Two fissures separate these lobes. The major, or oblique, fissure separates the lower lobe from the upper and middle lobes. The minor or horizontal fissure separates the upper lobe from the middle lobe. The left lung has two lobes—the upper lobe and the lower lobe; the lingula corresponds embryologically to the right middle lobe. A single oblique fissure separates the lobes.
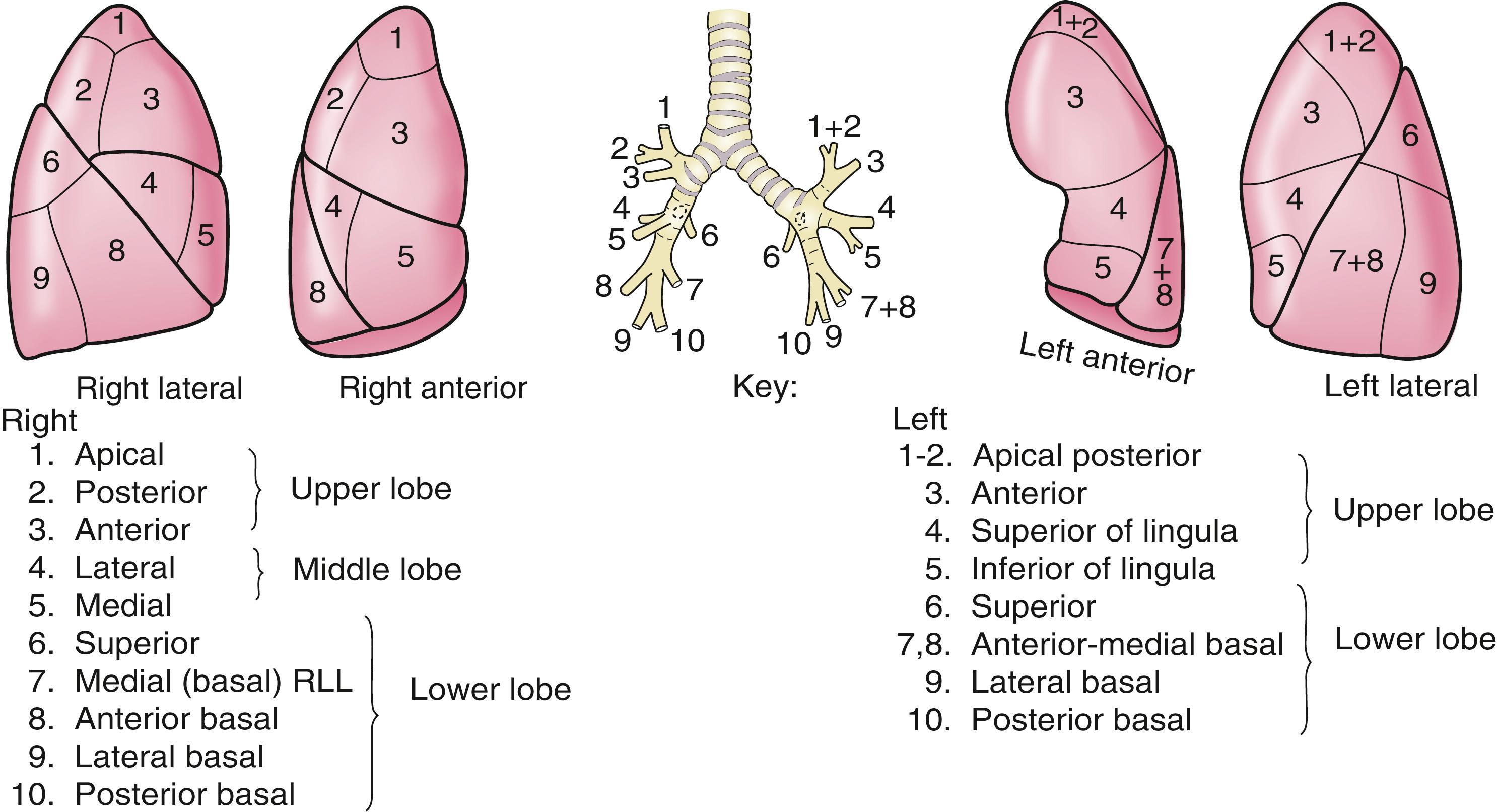
The bronchopulmonary segments are divisions of each lobe that contain anatomically separate arterial, venous, and bronchial supply. There are 10 bronchopulmonary segments on the right and 8 bronchopulmonary segments on the left.
The blood supply of the lung is twofold. Unoxygenated blood circulates from the right ventricle through the pulmonary artery to each lung. After oxygenation in the lung, the blood is returned to the left atrium through the pulmonary veins. Blood supply to the bronchi is from the systemic circulation by bronchial arteries arising from the superior thoracic aorta or the aortic arch, either as discrete branches or in combination with the intercostal arteries.
Lymphatic vessels are present throughout the lung parenchyma and pleura and gradually coalesce toward the hilar areas of the lungs. Generally, lymphatic drainage from the lung affects the ipsilateral lymph nodes; however, flow of lymph from the left lower lobe may drain to the right mediastinal (paratracheal) lymph nodes. Lymphatic drainage within the mediastinum moves cephalad. The pulmonary parenchyma does not contain a nerve supply.
The visceral pleura is separated from the parietal pleura by a small amount of pleural fluid, which allows nearly frictionless movement during respiration. The blood supply of the parietal pleura comes from the systemic arteries and veins, including the posterior intercostal, internal mammary, anterior mediastinal, and superior phrenic arteries and corresponding systemic veins. The blood supply of the visceral pleura is both systemic and pulmonary. The lymphatic drainage of the parietal pleura is into regional lymph nodes, including intercostal, mediastinal, and phrenic nodes. Visceral pleural lymphatics follow the superficial lung lymphatics and drain into the mediastinal lymph nodes. The parietal pleura underlying the ribs has rich nerve endings from the intercostal nerves. Generous local anesthesia is necessary for chest tube insertion. The visceral pleura is innervated by vagal branches and the sympathetic system.
The anatomic boundaries of the mediastinum include the thoracic inlet superiorly, the diaphragm inferiorly, the sternum anteriorly, the vertebral column posteriorly, and medially to the parietal pleura. Thoracic tumors that penetrate through the pleura (by definition) invade the mediastinum. Traditionally, the mediastinum can be divided into anterosuperior, middle, and posterior compartments. No specific anatomic planes define these areas. Fat and lymph nodes are found throughout the mediastinum.
The anterosuperior compartment includes the thymus gland. The right and left lobes of the thymus extend into the cervical areas, and these portions of the thymus must be resected to provide for complete extirpation of the gland.
The middle mediastinum contains the heart; pericardium; great vessels, including the ascending, transverse, and descending aorta; superior and inferior vena cava; pulmonary artery and veins; trachea and bronchi; and phrenic, vagus, and recurrent laryngeal nerves. The phrenic nerve enters the thorax through the thoracic inlet on the anterior aspect of the anterior scalene muscle.
The vagus nerve enters the thoracic inlet through the carotid sheath. It lies anterior to the subclavian and posterior to the innominate artery on the right. The right recurrent laryngeal nerve loops or “recurs” around the innominate artery to innervate the right vocal cord. The vagus nerve then continues posteriorly in the tracheoesophageal groove to innervate the trachea and continues down to innervate the esophagus. On the left side, the vagus nerve enters the thorax through the thoracic inlet, and as it exits the carotid sheath, it moves along the anterior aspect of the aortic arch. The recurrent laryngeal nerve arises from the vagus nerve and loops around under the ligamentum arteriosum and continues superiorly under the aorta and lies in the tracheoesophageal groove as it innervates the left recurrent laryngeal nerve. The left vagus continues posteriorly within the mediastinum along the esophagus to innervate both the trachea and the esophagus.
The posterior mediastinum contains structures between the heart/pericardium and trachea anteriorly and the vertebral column and paravertebral spaces posteriorly. The posterior mediastinum contains the esophagus, descending aorta, azygos and hemiazygos veins, thoracic duct, sympathetic chain, and lymph nodes. The thoracic duct originates from the cisterna chyli in the abdomen. It enters into the chest through the aortic hiatus in an anterolateral position and travels superiorly just to the right of midline in the chest along the anterolateral surface of the vertebral column. At approximately the level of T5, it crosses over to the left and continues superiorly to empty, posteriorly, into the junction of the left jugular and subclavian veins.
The inferior border of the mediastinum is the diaphragm, which separates the abdominal contents from the thorax. Hernias through the esophageal hiatus (paraesophageal hernias), through the foramen of Bochdalek (posteriorly), or through the foramen of Morgagni (anteriorly) may be initially identified as a mediastinal mass.
Each spinal root exits the neural foramina of the vertebral body and bifurcates to form a branch to the intercostal nerve to innervate the skin and intercostal musculature and a branch to the sympathetic ganglion. Intercostal nerves innervate the skin and musculature of the intercostal muscles. The spinal root divides as it exits the neural foramina. One branch goes to the intercostal nerve, and one lies in the posterior vertebral gutter to form the sympathetic ganglion. The thoracic sympathetic trunk comprises several ganglia that lie along the ribs. The most superior ganglion is the stellate ganglion.
The physiologic evaluation of the thoracic surgical patient must be individualized for each patient but generally emphasizes the pulmonary and cardiac function. The assessment of a patient’s ability to tolerate lung resection from a cardiopulmonary standpoint is fundamental to patient selection for surgery. Patients with advanced pulmonary disease and severe pulmonary dysfunction may have prohibitive risk, which may exist in greater than one third of patients with otherwise resectable lung disease.
Cigarette smoking is associated with increased postoperative pulmonary complications. If the patient is a smoker, he or she must stop smoking immediately. The physician must clearly communicate this message. Although there are few studies specific to pulmonary resection, there is evidence that smoking abstinence of 4 to 8 weeks’ duration preoperatively is necessary to reduce the incidence of complications. Ideally, patients are smoke-free for a minimum of 2 weeks and preferably for 4 to 8 weeks before surgery, although smoking cessation at any time is valuable. Smoking cessation programs may be helpful for these patients, and patients may need pharmacologic assistance. This combination may have increased efficacy in smoking cessation efforts over counseling alone.
Before the operation and in the perioperative period, deep venous thrombosis prophylaxis is provided by subcutaneous heparin or low-molecular–weight heparin and by sequential compression stockings. Perioperative antibiotics are used to minimize complications from infections. Postoperative morbidity may also be minimized by adequate pain control to facilitate early ambulation. Routine use of a thoracic epidural catheter, or intercostal rib blocks with long-acting local anesthetics, or patient-controlled analgesia provide excellent pain control. Incentive spirometry assists in expanding the lung and reducing the incidence of pulmonary morbidity. Nasal bilevel positive airway pressure for patients with obstructive sleep apnea may delay or eliminate the need for intubation or reintubation after pulmonary resection. Early mobilization is essential to avoid most perioperative complications.
Before thoracic operations, patients may be evaluated by a combination of radiographic and physiologic studies. A plain chest x-ray (CXR) is commonly obtained ( Fig. 58.5 ). Spirometry measures the lung volumes ( Fig. 58.6 ) and the mechanical properties of lung elasticity, recoil, and compliance. Pulmonary function testing ( Fig. 58.7 ) also evaluates gas exchange functions, such as carbon monoxide diffusing capacity (D lco ).



The predicted postoperative forced expiratory volume in 1 second (FEV 1 ) is the most commonly used as an indicator of postoperative pulmonary reserve. Depending on other evaluable factors, most patients with FEV 1 greater than 60% predicted can tolerate an anatomic lobectomy. If FEV 1 is less than 60% of predicted, further testing in an attempt to estimate postoperative FEV 1 (predicted postoperative FEV 1 [ppo-FEV 1 ]) could be considered. The quantitative ventilation-perfusion lung scan is used to assist in the calculation of postoperative residual pulmonary function after resection. Patients with a ppo-FEV 1 of 35% to 40% should functionally tolerate the operation.
Quantitative radionucleotide lung perfusion ( Fig. 58.8 ) provides a measurement of the relative function of each lobe and lung and allows an estimation of pulmonary function after lung resection:

A ppo-FEV 1 of 30% or less carries a greater risk for supplemental oxygen and ventilator dependence, but a decision to deny surgical resection to this group of patients must be considered on an individual basis because some will do better than expected with careful selection at experienced centers. Finally, in the immediate postoperative period, the ppo-FEV 1 is not likely to be realized secondary to limited ambulation, pain, or other emotional or physical factors.
D lco can be measured by several methods, although the single-breath test is most commonly performed. D lco measures the rate at which test molecules such as carbon monoxide move from the alveolar space to combine with hemoglobin in the red blood cells. D lco is determined by calculating the difference between inspired and expired samples of gas. D lco levels less than 40% to 50% are associated with increased perioperative risk.
The ratio of FEV 1 to forced vital capacity (FEV 1 /FVC) describes the relationship between the FEV 1 and the functional lung volume. In obstructive disease, the ratio is low (FEV 1 is low, and FVC is high); in restrictive disease, the ratio is about normal because both FEV 1 and FVC are reduced.
Flow-volume loops derived from spirometry describe the relationship between lung volume and air flow as the lung volume changes during a forced expiration and inspiration. The typical test consists of tidal breathing at rest, followed by maximal inspiratory effort to total lung capacity, then maximal expiratory effort to residual volume, concluding with maximal inspiratory effort to total lung capacity.
Cardiopulmonary exercise testing (CPET) can be extremely useful in the evaluation of marginal candidates (ppo-FEV 1 or predicted postoperative D lco <50% predicted) or patients who appear more disabled than expected from simple spirometry measurements. CPET includes exercise electrocardiography, heart rate response to exercise, and measurements of minute ventilation and oxygen uptake per minute. CPET allows a calculation of maximal oxygen consumption (VO 2 max) and provides insight into overall cardiopulmonary function (the “cardiopulmonary axis”) that cannot be ascertained from other objective studies. CPET may identify clinically occult cardiac disease and provide a more accurate assessment of pulmonary function than spirometry and D lco , which tend to overestimate functional loss after resection.
A patient’s risk of perioperative morbidity and mortality may be stratified by VO 2 max. A level less than 11 to 15 mL/kg/min is associated with an increased risk, and VO 2 max less than 10 mL/kg/min indicates high risk.
In patients undergoing evaluation for lung volume reduction surgery or for lung transplantation, a 6-minute walk test is used for a measure of the cardiac and pulmonary reserve. Patients are told to walk as far and as fast as they can during this time period. Distances of more than 1000 feet suggest an uncomplicated course.
Measurement of diaphragm function by fluoroscopy, the “sniff test,” or by ultrasonography is needed to determine symmetry of effort and to exclude paradoxical movement of the diaphragm. Paradoxical movement (elevation of one hemidiaphragm with active contraction/retraction of the other diaphragm) suggests paresis or paralysis. This finding may suggest a specific reason for breathlessness. Diaphragm plication may be therapeutic.
No single test result should be viewed as an absolute contraindication to surgical resection. Although the physiologic assessment for patients undergoing normal spirometry and minimal comorbidity is straightforward, patients with marginal preoperative indices must be considered on an individual basis.
The choice of incision depends on the operation, the patient’s underlying physiologic condition, and the anticipated benefits and limitations of the planned approach. Video-assisted thoracoscopic surgery (VATS), robotic surgery, and other minimally invasive surgical techniques have been developed to treat most thoracic problems, including lung cancer, mediastinal tumors, pleural diseases, and parenchymal diseases, and to diagnose and stage thoracic malignancies. Various small incisions are made for the camera and other instruments depending on the location of the tumor. The ribs are not spread. Improved lighting and optics create excellent exposure and visualization. Advantages of minimally invasive surgical techniques include minimizing pain and surgical trauma from the incisions, decreasing hospitalization, and improving convalescence.
A thoracotomy requires spreading the ribs with a retractor and is used for operations on a single thorax. The patient is placed in a lateral decubitus position. The location of the incision may be posterior, axillary, or anterior. Posteriorly, an oblique incision is used with or without sparing the latissimus dorsi muscle. The chest is typically entered through the fifth interspace for pulmonary resection. A vertical axillary incision is made anterior to the latissimus dorsi muscle, and the chest is entered through the fourth interspace. This approach provides excellent hilar visualization. The anterior or anterolateral thoracotomy is created by a curvilinear incision underneath the inferior border of the pectoralis major muscle at the inframammary fold. A median sternotomy is performed using a vertical incision from the sternal notch to the xiphoid. A sternal saw is then used to divide the sternum in the midline. With gentle retraction, the sternum can be spread approximately 8 to 10 cm to allow access to the mediastinum, heart, great vessels, and right and left thorax. The pleura can be opened on either side to explore the hemithorax. The sternum is usually closed with stainless steel wire.
The transverse sternotomy or “clamshell” incision is larger than a median sternotomy and more uncomfortable for the patient. This incision combines two anterior thoracotomy incisions in the inframammary fold with transverse division of the sternum at the fourth intercostal space. Both internal mammary arteries are ligated. This approach is ideal for accessing both the right and the left hilum and providing additional exposure for large mediastinal tumors, bilateral hilar dissections, bilateral lung transplantation, or posterior-based metastases in both lungs.
Various congenital lung abnormalities can occur as a consequence of disturbed embryogenesis. Bilateral agenesis of the lungs is fatal. Unilateral agenesis may occur more frequently on the left (∼70%) than on the right (∼30%), with more than a 2:1 male-to-female ratio.
Hypoplasia of the lungs may occur as a result of interference with the development of the alveolar system during the last 2 months of gestation. Bochdalek hernia is the most frequent cause of hypoplasia. Conditions associated with hypoplasia of the lungs include oligohydramnios, prune-belly syndrome (deficiency in the abdominal musculature, genitourinary abnormalities), scimitar syndrome (abnormal pulmonary vein draining into the inferior vena cava, demonstrated as a crescent along the right heart border on cardiac angiography), and dextrocardia. Isolated pulmonary hypoplasia is rare.
Hyaline membrane disease (or infant respiratory distress syndrome) is frequent in premature infants (24–28 weeks’ gestation) and infants of diabetic mothers. At a gestational age of 24–28 weeks, infants have an immature surfactant system. Hyaline membrane disease develops in the alveoli, causing congestion and a lung with a deep purple gross appearance. Respiratory distress frequently ensues, requiring high concentrations of oxygen. CXRs demonstrate a reticulogranular ground-glass appearance from the interstitial edema. As needs for oxygen and ventilator pressure increase to counteract this interstitial edema, pneumothorax frequently occurs.
Congenital cystic lesions present in 1 in 10,000 to 35,000 births and present as a spectrum of anomalies. Majority of these cystic lesions comprise congenital pulmonary airway malformations (CPAM)/congenital cystic adenomatoid malformations, pulmonary sequestrations, congenital lobar emphysema, and bronchogenic cysts. They generally occur as a result of separation of the pulmonary remnants from airway branchings. Clinically, approximately one third of patients do not have symptoms; one third have cough; and one third have infection or, rarely, hemoptysis. Treatment may be with antibiotics or, for more severe localized cases, with resection. Any cystic lesion that enlarges on serial radiographs needs to be considered for resection.
Bronchogenic cysts arises from a tracheal or bronchial diverticulum (see also “Primary Mediastinal Cysts”). This diverticulum becomes completely separated from the trachea and is frequently found as an asymptomatic mass on routine CXRs. Symptoms may arise from compression of adjacent airways and from infection. On computed tomography (CT) of the chest, a homogeneous, well-circumscribed mass adjacent to the trachea may be seen ( Fig. 58.9 ). Infected cysts are characterized by an air fluid level. Bronchogenic cysts accounts for 10% of mediastinal masses in children, they are located in the midmediastinum. Treatment consists of excision in symptomatic cases while controversy exists regarding resection in asymptomatic patients.

Lobar emphysema is the most commonly resected congenital cystic lesion (50%). Its pathogenesis is related to intrinsic or extrinsic airway obstruction leading to the creation of a “ball-valve” mechanism and consequently to air trapping. The onset of rapidly progressive respiratory distress usually occurs 4 to 5 days to several weeks after birth. It rarely occurs after 6 months of age. It affects the upper lobes predominately. Treatment is lobectomy.
CPAMs, previously termed congenital cystic adenomatoid malformations , are the second most commonly resected congenital cystic lesion. They result from abnormalities in branching morphogenesis of the lung. There are five types of CPAM according to the Stocker classification (types 0-4), with type 1 being the most common one (60%–70%). In this type of malformation, single or multiple cysts larger than 2 cm that are covered by pseudostratified columnar epithelium are formed yielding an “adenomatoid” malformation. The lung has the appearance of Swiss cheese and feels like a large rubbery mass. With air trapping and overdistention, respiratory distress may occur, which is optimally relieved by lobectomy. Type 4 CPAM is strongly associated with malignancy in particular pleuropulmonary blastoma.
Bronchopulmonary sequestration (BPS) is an area of embryonic lung tissue, separate from the tracheobronchial tree, which receives blood supply from an anomalous systemic artery from the aorta, not the pulmonary artery. This condition occurs secondary to an accessory lung bud caudal to the normal lung, but with a lack of absorption of primitive surrounding splanchnic vessels. During lung development, interlobar sequestration (75%) occurs early. Later, after the pleura forms, extralobar sequestration occurs (25%), primarily on the left side (66%), and is completely enclosed by its own pleura. The extralobar sequestration blood supply is usually from the thoracic or upper abdominal aorta to systemic (azygos or hemiazygos veins). Extralobar sequestration is more common in male patients. Intralobar sequestration occurs within the lower lobes predominately (>95%) and is equally distributed between the right and left lower lobes. Intralobar sequestration blood supply is from the descending thoracic aorta that usually traverses the pulmonary ligament. Venous drainage is via the pulmonary veins. The thoracic aorta provides 95% of the systemic blood supply to the pulmonary sequestration. Infants with respiratory symptoms or with large BPS are treated by surgical excision. Asymptomatic small BPS can either be treated by embolization of the feeding artery or may be conservatively managed by observation ( Fig. 58.10 ). Hybrid BPS/CPAM lesions have been reported in a substantial proportion of cases of BPS. These hybrid lesions have histologic features of CPAM and a blood supply from a systemic artery.

Cystic fibrosis is an autosomal recessive disorder that is found more commonly in whites. Excessively thick mucus leads to recurrent infections, bronchitis, and bronchiectasis. Fibrosis and cystic changes on pathologic examinations are identified. Pneumothorax may occur secondary to air trapping. Lung failure is the most frequent cause of death. Bilateral lung transplantation should be considered when the disease rapidly progresses and the remaining pulmonary reserve is low.
Esophageal atresia with tracheoesophageal fistula is the most frequent abnormality of the trachea in infants (see Chapter 67 ). Bronchial atresia is the second most frequent congenital pulmonary lesion after tracheoesophageal fistula. The lung tissue distal to the atresia expands and becomes emphysematous as a result of air entry through collateral airways/pores. With no exit for air or mucus because of this blind bronchial stump, emphysema from air trapping or development of a mucocele may occur. CXRs may demonstrate hyperinflation of a lobe or a segment. The oval density may be identified between the hyperinflated lung and the hilum. The left upper lobe is the most frequently involved of all lobes within the lung. Diagnosis may be confirmed with bronchography or CT. The surgeon must rule out a mucous plug, adenoma, vascular compression, or sequestration.
Tracheal agenesis is a rare phenomenon and is fatal. The trachea is absent from the larynx to the carina, and bronchi communicate with the esophagus.
Tracheal stenosis is also rare and consists of generalized hypoplasia, a funnel-like trachea, and bronchial and segmental malformations. The right upper lobe bronchus may come from the trachea directly and may be associated with an aberrant left pulmonary artery (so-called pulmonary artery sling). Completely circular tracheal rings are commonly associated with a pulmonary sling. Repair of the trachea is by vertical incision and widening of the tracheal lumen.
Tracheomalacia can be identified by diagnostic imaging (dynamic expiratory CT) or bronchoscopy. The surgeon should notice marked variation of the tracheal lumen with inspiration and expiration. Collapse of greater than 70% of the lumen during expiration is consistent with this condition. Respiratory difficulty ensues from the intermittently collapsing trachea. Relief of the extrinsic compression is needed. Stent placement in adults or posterior splinting or primary tracheobronchoplasty may be required. This condition may have a congenital predisposition but is most often seen in adults with COPD.
Congenital vascular disorders of the lungs may occur. In Swyer-James and Macleod syndrome, there is idiopathic hyperlucent lung. This problem develops from chronic pulmonary infections such as bronchiectasis. As the consolidation persists, decreased pulmonary artery blood supply may cause an “autopneumonectomy” and a hyperlucent lung.
Scimitar syndrome is associated with hypoplastic right lung with drainage of the pulmonary vein to the inferior vena cava. The anomaly is usually corrected using extracorporeal cardiopulmonary support. A patch from the pulmonary vein to the left atrium via an atrial septal defect corrects this problem.
Pulmonary arteriovenous malformations may exist as one or more pulmonary artery-to-pulmonary vein connections, bypassing the pulmonary capillary bed. This connection results in a right-to-left shunt. Approximately one third of these patients have hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). Approximately half of the malformations are small (<1 cm) and tend to be multiple. Half are greater than 1 cm and usually less than 5 cm and tend to be subpleural. These lesions need to be considered in the differential diagnosis of any patient with hemoptysis that is unexplained on the basis of bronchoscopy or routine imaging. Either local resection or catheter embolization of these lesions can be curative.
A pulmonary vascular sling consists of an anomalous or aberrant left pulmonary artery, which causes airway obstruction, and is associated with other anomalies. The aberrant left pulmonary artery arises from the right (main) pulmonary artery and courses between the trachea and the esophagus to supply the left lung. More than 90% of patients have wheezing and stridor. Esophagoscopy shows the anomalous vessel anterior to the esophagus; bronchoscopy demonstrates the vessel posterior to the trachea. Surgical correction requires relocation of the left pulmonary artery from its right-sided origin to the main pulmonary artery. If tracheal stenosis with complete tracheal rings are identified segmental resection of the trachea or tracheoplasty should be performed.
Vascular rings constitute 7% of all congenital heart problems. The most common vascular ring is a double aortic arch, which occurs in 60% of these patients. The right, or posterior, arch is the larger arch and gives rise to the right carotid and right subclavian arteries. The ring wraps around both the trachea and the esophagus. A posterior indentation is noted in the esophagus on barium swallow. Simple division corrects the anomaly. A right aortic arch with a retroesophageal left subclavian artery and left ligamentum arteriosum occurs in approximately 25% to 30% of patients with vascular rings. Intracardiac defects occur with a double aortic arch. Most of these infants require operation within the first weeks or months of life. Patients with vascular rings require a careful history and barium swallow for diagnosis. Bronchoscopy or esophagoscopy are not routinely ordered because they may be harmful. Echocardiography is a complementary test. CT scan and magnetic resonance imaging (MRI) may be used to further delineate the anatomy. Repair is performed through the left chest. Division of the smaller arch, usually the left one, is undertaken. The ligamentum is divided, and the trachea and the esophagus are freed from the surrounding tissues. When a retroesophageal right subclavian artery with left ligament occurs, the patient may complain of dysphagia, which is referred to as dysphagia lusoria. The differential diagnosis includes neuromotor diseases of the esophagus or stricture.
Lung cancer is a significant global health problem. In the United States in 2018, there were estimated to be 234,030 new cases of lung cancer. Lung cancer is the most frequent cause of death from cancer in men and women and accounts for 13.0% of all cancer diagnoses and 26% of all cancer deaths in the United States. Lung cancer deaths exceed the combined total deaths from breast, prostate, and colorectal cancer. Since 1987, more women have died of lung cancer than breast cancer. Lung cancer deaths have decreased by approximately 3% per year in men and by approximately 2% per year in women. Smoking cessation in women has lagged behind smoking cessation in men, and thus the incidence of lung cancer in women has not declined as much as the incidence in men ( Fig. 58.11 ). The decline in lung cancer incidence and mortality rate likely reflects decreasing cigarette smoking and potentially earlier detection of smaller, asymptomatic lung cancers. African American men have both the highest incidence and the highest death rate from cancer of the lung and bronchus.

Lung cancer survival is stage specific. The overall 1-year and 5-year survival rates are 44% and 17%, respectively. Patients presenting with localized (early-stage) lung cancer have a 5-year survival rate of 54%. However, greater than 50% of patients present with locally advanced or metastatic disease and their 1-year and 5-year survival rates do not exceed 26% and 4%, respectively.
Cigarette smoking is unequivocally the most important risk factor in the development of lung cancer. Other environmental factors may predispose to lung cancer. Environmental radon gas exposure is estimated to be the second most important risk factor. Other factors include asbestos, arsenic, chromium, nickel, organic chemicals, iatrogenic radiation exposure, air pollution, and secondary smoke from nonsmokers.
Radon is associated with approximately 18,000 lung cancer deaths a year. Radon is a natural radioactive gas released from the normal decay of uranium in the soil. Inhalation is associated with health risk. Inexpensive test kits are available to determine the amount of radon present in homes.
Optimal treatment of lung cancer requires accurate diagnosis and clinical staging before treatment begins. The anatomic basis for staging (tumor, lymph nodes, and metastases) includes the physical properties of the tumor and the presence of regional or systemic metastases. The biologic and immunologic basis for staging/disease characterization (molecular and immunologic markers prognostic for survival and indicative of the potential to respond to specific treatments) may be incorporated into staging systems of the future.
In 2015 the World Health Organization (WHO) issued a revised classification of tumors of the lung. By expanding the use of immunohistochemistry and by providing recommendations for genetic characterization of the tumors more accurate and clinically relevant subtyping of the tumors was established. The major types of malignant tumors of the lung are adenocarcinomas, squamous cell carcinomas (SCCs), large cell carcinomas, and neuroendocrine tumors of the lung; each of these groups has multiple subtypes that differ by their morphologic, genetic, and biologic properties. Key characteristics of these tumors are described below.
Adenocarcinomas are malignant epithelial tumors with glandular differentiation or mucin production, showing acinar, papillary, lepidic (bronchioloalveolar), or solid with mucin growth patterns or a mixture of these patterns. Adenocarcinoma of the lung is the most frequent histologic type of lung cancer accounting for approximately 45% of all lung cancers. Microscopic features consist of cuboidal to columnar cells with adequate to abundant pink or vacuolated cytoplasm and some evidence of gland formation. Most of these tumors (75%) are peripherally located. Adenocarcinoma of the lung tends to metastasize earlier than SCC of the lung and more frequently to the central nervous system.
The pathology of adenocarcinoma has been revised. Bronchoalveolar or bronchioloalveolar carcinoma and mixed type adenocarcinoma have been eliminated, and adenocarcinoma in situ (pure lepidic growth, tumor cells proliferating along the surface of intact alveolar walls without stromal or vascular invasion) and minimally invasive adenocarcinoma (predominantly lepidic growth with <5 mm invasion) have been created. A solitary tumor focus of adenocarcinoma in situ or minimally invasive adenocarcinoma is treated in a manner similar to invasive adenocarcinoma (in the majority of cases anatomic resection of the affected segment/lobe of the lung). The management of multifocal adenocarcinoma in situ disease is generally more complex. In this scenario, surgical resection, ablation, and radiation of the most active lesions is performed while following up on the progression of the additional lesions. The aim is to eliminate the lesion that progress while preserving as much lung tissue as possible.
SCC is a malignant epithelial tumor showing keratinization and/or intercellular bridges that arises from bronchial epithelium. Over 90% of SCC occur in cigarette smokers, these tumors occur in approximately 30% of patients with lung cancer. Approximately two thirds of these tumors are centrally located and tend to expand against the bronchus, causing extrinsic compression. SCC are prone to undergo central necrosis and cavitation. SCC tends to metastasize later than adenocarcinoma. Microscopically, keratinization, stratification, and intercellular bridge formation are exhibited. SCC may be more readily detected on sputum cytology than adenocarcinoma.
A diagnosis of large cell undifferentiated carcinoma may be made when specific cytologic features of SCC or adenocarcinoma or neuroendocrine differentiation are lacking. These tumors tend to occur peripherally and may metastasize relatively early. Microscopically, these tumors show sheets of round to polygonal cells with prominent nucleoli and abundant pale-staining cytoplasm without differentiating features.
Neuroendocrine tumors of the lung share specific morphologic, ultrastructural, immunohistochemical, and molecular features; they arise from cells derived from the embryologic neural crest. This group of tumors includes small cell carcinomas, large cell neuroendocrine carcinomas, and typical and atypical carcinoids. Typical carcinoids show a relatively indolent growth pattern while small cell carcinoma and large cell neuroendocrine carcinomas are highly aggressive. Small cell lung cancer represents approximately 20% of all lung cancers. In the majority of cases (80%), these tumors are centrally located and tend to spread early to mediastinal lymph nodes and distant sites, especially the bone marrow and brain. Microscopically, the tumors appear as sheets or clusters of cells with dark nuclei and little cytoplasm. Neurosecretory granules are evident on electron microscopy. Small cell lung cancer is staged according to the lung cancer TNM staging system; however, from a clinical perspective, the disease may also be addressed as limited stage (disease restricted to an ipsilateral hemithorax within a single radiation port) and extensive stage (obvious metastatic disease). These tumors are often advanced at presentation with an aggressive tendency to metastasize. Chemoradiotherapy is generally used for treatment. Prophylactic cranial irradiation is considered in a patient with limited or extensive disease that responds well to first-line therapy. Complete responses may occur in approximately 30%, of patients; however, the 5-year survival rate is only 5%. Patients with early-stage disease (e.g., <3 cm in size, no nodal metastases, and no extrathoracic metastases) may be considered for surgical resection, followed by adjuvant systemic therapy. Staging before resection includes 18 F-fluorodeoxyglucose positron emission tomography (FDG-PET), brain CT or MRI, and mediastinoscopy. Mediastinal metastases on clinical staging suggest advanced disease, which is best treated with chemoradiotherapy. ,
Lung cancers commonly metastasize to the pulmonary and mediastinal lymph nodes (lymphatic spread). Hematogenous spread of lung cancer commonly results in metastases to the adrenal glands, brain, lung, and bone. Adenocarcinoma is more likely to metastasize to the central nervous system. Bone metastases are osteolytic. Extrathoracic metastases may occur without hilar nodes or mediastinal metastases.
Patients with lung cancer often present with advanced disease stage and symptoms. The pulmonary parenchyma does not contain nerve endings, and tumors may grow undetected until symptoms of pain, hemoptysis, or obstructive pneumonia arise. With the increased use of CT in the United States, smaller asymptomatic lung cancers are being identified.
Screening for lung cancer has been evaluated by the National Lung Screening Trial (NLST). The NLST is a prospective randomized multicenter study evaluating annual low-dose helical CT with annual chest radiography. The 53,454 enrolled patients were randomly assigned between the two arms. The men and women screened were asymptomatic and older (age range: 55 to 74 years), with 30 pack-years or more of cigarette smoking at the beginning of the trial, and were either current smokers or had recently quit (within 15 years). The NLST found that patients randomly assigned to low-dose helical CT screening for 3 years (compared with CXR) had a reduced lung cancer-specific mortality and all-cause mortality. The death rate from lung cancer in this high-risk population was reduced by 20%, and all-cause mortality was reduced by 7%. The study showed the benefit is statistically significant, as 354 lung cancer deaths occurred in the CT group compared with 442 lung cancer deaths in the CXR group ( P = 0.0041), leading to early study closure.
More recently, the results of the European Nelson lung cancer screening trial have been reported. In this population-based controlled trial, 15,792 individuals were randomized 1:1 to either the study arm or control arm. Study arm participants were offered CT screenings at baseline, one, three, and five and one-half years after randomization. No screenings were offered to control arm participants. The follow-up period comprised a minimum of 10 years, unless deceased, for 93.7% of enrolled participants. Detection rates across the rounds varied between 0.8% and 1.1%, and 69% of screen-detected lung cancers were detected at Stage IA or IB. A total of 261 lung cancers (52 interval cancers) were detected before the fourth round of follow-ups. In a subset of analyzed patients, surgical treatment was three times significantly more prevalent in the study lung cancer patients than in control arm patients (67.7% vs. 24.5%, P < 0.001). Overall the study has shown that the use of CT screening among asymptomatic men at high risk for lung cancer led to a 26% (9-41%, 95% confidence interval [CI]) reduction in lung cancer deaths at 10 years of study follow-up (at 86% compliance). In the smaller subset of women, the rate-ratio of dying from lung cancer varied between 0.39 and 0.61 in different years of follow-up, indicating an even larger reduction in lung cancer mortality than in men.
Screening for early lung cancer detection using low-dose helical CT is recommended by the National Comprehensive Cancer Network (NCCN) for 1) individuals aged 55 to 74 years with a 30 or more pack-year history of smoking tobacco who currently smoke or, if a former smoker, have quit within 15 years and 2) individuals aged 50 years or older with a 20 or more pack-year history of smoking tobacco who are either current or former smokers and whose risk for lung cancer is greater than 1.3% , (key risk factors include personal history of cancer or lung disease, family history of lung cancer, radon exposure, and occupational exposure to carcinogens). The U.S. Preventive Services Task Force is currently revising its recommendations for lung cancer screening.
Physicians may discuss testing for early-stage lung cancer with their patients on an individual basis. This discussion with the patient should include the risks, benefits, and limitations associated with lung cancer screening with low-dose helical CT and should occur before a decision is made to start any lung cancer screening. Screening is not an alternative to smoking cessation. A clear and unambiguous statement is needed from the physician that smoking cessation is essential. Pharmacologic or other strategies need to be tailored to the individual patient. Screening of asymptomatic patients may identify nonspecific findings, such as over diagnosis of benign nodules, which could result in patient anxiety as well as additional radiation exposure.
The diagnosis of lung cancer can be challenging. Many benign conditions mimic lung cancer. Physical examination should focus on the cardiorespiratory system. In addition, the presence of cancer in supraclavicular lymph nodes, identified by a careful examination of the cervical and supraclavicular lymph nodes, suggests advanced disease (N3 lymph node descriptor), and therapy other than resection is recommended. Paraneoplastic syndromes are distant manifestations of lung cancer (not metastases) as revealed in extrathoracic nonmetastatic symptoms. The lung cancer causes an effect on these extrathoracic sites by producing one or more biologic or biochemical substances. Small cell lung cancer frequently causes neurologic paraneoplastic syndromes. Other lung cancers may cause hypertrophic osteoarthropathy.
Non–small cell lung cancer (NSCLC) typically occurs in patients who are 50 to 70 years old with a history of cigarette smoking. Patients develop symptoms based on the physical impact of tumor growth within the lung parenchyma. Symptoms such as cough, dyspnea, chest wall pain, and hemoptysis are related to the physical presence of the tumor and its interactions with the structures of the lung and chest wall.
Once a clinical suspicion for NSCLC arises the clinician should aim to achieve a timely diagnosis and accurate staging so that appropriate therapy can be administered. The workup of a primary solitary pulmonary nodule (SPN) involves the combination of imaging modalities including CXR, CT, and often also a PET-CT. In addition, a tissue biopsy is often performed based on the suspicion level for malignancy. Guidelines for management of a SPNs are available. Under certain circumstances, a SPN may be deemed benign with adequate confidence in the absence of a pathologic diagnosis. SPNs that are entirely calcified, or radiologically stable on CT of the chest over a minimum of 2 years, are very likely to be benign. Review of old radiographs or other prior imaging studies can assist in evaluation of changes in the mass.
In patients with a clinically suspicious SPN, histologic information may be needed to assess risk and benefit of the various available treatment options. The least invasive strategy compatible with obtaining a diagnosis would be recommended. Diagnostic bronchoscopy, transthoracic needle aspiration, or navigational bronchoscopy can be selected based on the size, location, and condition of the patient. In a physiologically fit patient with a suspicious yet undiagnosed SPN, nonanatomic wedge or sublobar resection provides a diagnosis. Confirmation of NSCLC by the pathologist should be followed by definitive (anatomic) resection in the same setting. For a SPN in the absence of a cancer diagnosis (that cannot be removed by wedge resection), a lobectomy can be considered for diagnosis (and treatment). A pneumonectomy is not performed without a cancer diagnosis.
One third of patients with NSCLC may have a pleural effusion at the time of presentation. Pleural fluid sampling with thoracentesis is required for cytologic examination. Malignant pleural effusion (MPE) is a contraindication to resection, but many pleural effusions in this setting may be reactive in origin.
Bronchoscopy is recommended before any planned pulmonary resection. The surgeon independently assesses (via bronchoscopy) the endobronchial anatomy to exclude secondary endobronchial primary tumors and to ensure that all known cancer will be encompassed by the planned pulmonary resection. Secretions can be cleared with suctioning and gentle irrigation. When pneumonectomy or bronchoplastic resection is contemplated for a central tumor, the surgeon’s assessment at bronchoscopy is critical to the determination of whether complete (R0) resection can be achieved.
If the patient has hard palpable lymph nodes in the cervical or supraclavicular area, fine-needle aspiration or biopsy may provide an accurate diagnosis of N3 disease.
Staging is a description of the extent of the cancer based on similarities in survival for the group of patients with those characteristics. The staging system creates a shorthand description of the tumor, lymph nodes, and metastatic characteristics of the patient to facilitate the choice of optimal therapy and to evaluate outcomes based on the clinical and pathologic stage. The American Joint Committee on Cancer (AJCC) and the Union for International Cancer Control work to establish and promulgate staging system guidelines. The 2018 eighth edition TNM stage classification for lung cancer provides the basis for specific patient stage groupings and is used for initial treatment recommendations based on the clinical stage and on the pathologic stage after pulmonary resection.
The clinician’s responsibility is to ensure the highest possible degree of certainty of the extent of the disease and to recommend the therapy or therapeutic combination of greatest efficacy based on the disease stage. Optimal staging assists the clinician in providing the best recommendations for therapeutic interventions for the patient. The clinical stage is the physician’s best and final estimate of the extent of disease based on all available information from invasive and noninvasive studies before the initiation of definitive therapy. Key imaging modalities used in clinical staging of NSCLC patients are CT, PET-CT, and MRI of the brain. Invasive staging of the mediastinum, pleural taps and biopsies from suspected metastatic sites are also often performed to complement and more accurately determine disease stage. The pathologic stage is the determination of the physical extent of the disease based on histologic examination of the resected tissues, including the hilar and mediastinal lymph nodes.
As the tumor size increases, survival decreases. Diagnostic imaging commonly includes a CXR and CT scan of the chest and upper abdomen, including the liver and adrenals ( Fig. 58.12 ). The CXR provides information on the size, shape, density, and location of the primary tumor and its relationship to the mediastinal structures. CT scan of the chest provides more detail on tumor characteristics and provides information on the relationship of the tumor to the mediastinum, chest wall, and diaphragm as well as invasion into the vertebrae or mediastinal structures. MRI of the chest may complement CT in better delineating tumor invasion in such patients. MRI of the brain is reserved for patients with stage I or II cancer with new neurologic symptoms (vertigo, headache) and for all patients with stage III and IV cancer, as well as patients with small cell carcinoma or superior sulcus tumors (Pancoast tumor) because these patients have a higher incidence of occult brain metastases.

Determination of metastases to mediastinal lymph nodes constitutes a critical point in staging and treatment recommendations. Mediastinal lymph node metastases are present in 26% to 32% of patients at the time of diagnosis and initially assessed with chest CT. Lymph nodes may be enlarged normally from infection (e.g., histoplasmosis, previous bronchitis, or pneumonia) or other inflammatory processes, such as granulomatous disease. Mediastinal adenopathy is most often defined as lymph nodes with a maximal transverse diameter greater than 1 cm on axial tomographic images. In the absence of mediastinal nodes greater than 1 cm in diameter, the likelihood of N2 or N3 disease is low. If mediastinal nodes greater than 1 cm are identified, nodal tissue must be examined (e.g., with endoscopic bronchial ultrasound (EBUS), cervical mediastinoscopy, endoscopic ultrasound, VATS) for histologic evidence of metastases before definitive resection can be considered.
CT has a reported sensitivity of 57% to 79% for mediastinal lymph node assessment in NSCLC, with a positive predictive value of 56%. No CT size criteria are entirely reliable for the determination of mediastinal lymph node involvement. Larger mediastinal lymph nodes are more likely to be associated with metastasis (>70%); however, normal-sized lymph nodes (<1 cm) have a 7% to 15% chance of containing metastases.
PET may assist in evaluating the local extent and presence of known or occult metastases based on the differential increased metabolism of glucose by cancer cells compared with normal tissues ( Fig. 58.13 ). A PET scan is not a cancer-specific study or a “cancer scan,” as high cellular glucose metabolism is seen in inflammatory processes in addition to malignancy. Histologic confirmation of FDG avid mediastinal lymph node involvement is indicated to complete clinical staging before final treatment decisions. FDG-PET coupled with CT may yield increased sensitivity and specificity in determining the stage of patients with lung cancer before treatment interventions. The negative predictive value of PET-CT for mediastinal lymph node metastases from NSCLC is in the range of 85% to 95% being more accurate in smaller (T1) rather than larger (T2) tumors and in larger (>1 cm) than smaller (<1 cm) lymph nodes.

Invasive staging includes cervical mediastinoscopy or mediastinotomy (Chamberlain procedure), EBUS, or endoscopic ultrasound. Cervical mediastinoscopy is traditionally indicated in patients with otherwise operable NSCLC with enlarged paratracheal or subcarinal lymph nodes, particularly if the cancer is proximal, if pneumonectomy is planned, or if the patient is at increased risk for the planned resection. Cervical mediastinoscopy is commonly performed for biopsy of bilateral paratracheal (levels 2 and 4) and subcarinal (level 7) lymph nodes. A left anterior mediastinotomy is used to gain access to the mediastinum after resection of the second costosternal cartilage to evaluate the aortopulmonary window (level 5) or anterior mediastinum (level 6) lymph nodes. Cervical mediastinoscopy has a negative predictive value greater than 90%, it may be performed as an outpatient procedure, and is associated with a low rate of significant complications. When pathologic “frozen section” evaluation fails to demonstrate malignant nodal involvement, mediastinoscopy may be followed by resection under the same anesthetic. The use of cervical mediastinoscopy regardless of radiographic evidence of nodal involvement (“routine mediastinoscopy”) is not a cost-effective approach and adds little to the accuracy of staging in patients with an adequate noninvasive preoperative evaluation. Additional sampling techniques may be helpful. In particular, EBUS, which provides access to nodal stations 2, 4, 7, 10, 11, and endoscopic ultrasound via the esophagus, which provides access to nodal stations 2, 4, 7, 8, and 9, may be as sensitive as and less invasive than mediastinoscopy. VATS techniques can evaluate enlarged level 4, 7, 8, 9, and 10 lymph nodes bilaterally and levels 5 or 6 lymph nodes on the left.
Endothoracic (M1a) and extrathoracic metastases (single extrathoracic metastasis M1b or multiple extrathoracic metastasis [M1c]) are common in lung cancer. Beyond a thorough history, physical examination, and standard imaging based staging techniques (CT, PET-CT, and MRI of the brain), additional evaluation for metastatic disease is indicated only in selected cases. In particular, a tissue diagnosis should be obtained if confirmation of metastasis is anticipated to alter the treatment plan. When pleural effusion is present a diagnostic tap is usually performed to confirm tumor spread to the pleural space. Up to 7% of patients have metastatic adrenal involvement at presentation. The standard CT evaluation of the chest should also include evaluation of the upper abdomen including the liver and the adrenal glands. Indeterminate adrenal lesions on CT may be further evaluated with MRI or with CT-guided percutaneous biopsy.
The International Association for the Study of Lung Cancer (IASLC), together with the AJCC, has recently issued the eighth edition of lung cancer staging system. For this project the IASLC has collected data on a total of 94,708 patients diagnosed with lung cancer from 1999 to 2010. The data has originated from 35 different databases in 16 countries on 5 continents. The information was provided by credible centers, which facilitated data collection and analysis of a large patient population. After exclusions, 77,156 patients remained evaluable, including 70,967 with NSCLC and 6189 with small cell lung cancer. Nearly 85% of the patients included in the database underwent surgical treatment, either alone (57.7%) or together with chemotherapy (21.1%), radiotherapy (1.5%), or both (4.4%). Survival was analyzed using Kaplan-Meier methods, and survival estimates were compared using the likelihood ratio test from Cox proportional hazards regression. Extensive analysis allowed definition of TNM categories and stage groupings that demonstrated consistent discrimination overall and within multiple different patient cohorts (e.g., clinical or pathologic stage, R0 or R-any resection status, geographic region). Additional analyses provided evidence of applicability over time, across a spectrum of geographic regions, histologic types, evaluative approaches, and follow-up intervals. ,
The TNM definitions, nodal characteristics, and stage groupings of the TNM subsets are shown in Tables 58.1 to 58.3 . Other schematics have been created for the lymph node map and T characteristics. The mediastinal and regional lymph node classification schema is presented in Fig. 58.14 . This map presents a graphic representation of mediastinal and pulmonary lymph nodes in relation to other thoracic structures for optimal dissection and anatomic labeling by the surgeon.
| T: Primary Tumor | |
| TX | Primary tumor cannot be assessed, or tumor proven by the presence of malignant cells in sputum or bronchial washings but not visualized by imaging or bronchoscopy |
| T0 | No evidence of primary tumor |
| Tis | Carcinoma in situ |
| T1 | Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus) a |
| T2 | Tumor >3 cm but ≤5 cm or tumor with any of the following features c : |
|
|
|
Tumor >3 cm but ≤4 cm in greatest dimension Tumor >4 cm but ≤5 cm in greatest dimension |
| T3 | Tumor >5 cm but ≤7 cm in greatest dimension or associated with separate tumor nodule(s) in the same lobe as the primary tumor or directly invades any of the following structures: chest wall (including the parietal pleura and superior sulcus tumors), phrenic nerve, parietal pericardium |
| T4 | Tumor >7 cm in greatest dimension or associated with separate tumor nodule(s) in a different ipsilateral lobe than that of the primary tumor or invades any of the following structures: diaphragm , mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, and carina |
| N: Regional Lymph Nodes Involvement | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastases |
| N1 | Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension |
| N2 | Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s) |
| N3 | Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s) |
| M (Distant Metastasis) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis present |
|
Separate tumor nodule(s) in a contralateral lobe; tumor with pleural or pericardial nodule(s) or malignant pleural or pericardial effusion d Single extrathoracic metastasis e Multiple extrathoracic metastases in one or more organs |
a The uncommon superficial spreading tumor of any size with its invasive component limited to the bronchial wall, which may extend proximal to the main bronchus, is also classified as T1a.
b Solitary adenocarcinoma, ≤ 3cm with a predominately lepidic pattern and ≤ 5mm invasion in any one focus.
c T2 tumors with these features are classified as T2a if ≤4 cm in greatest dimension or if size cannot be determined, and T2b if >4 cm but ≤ 5 cm in greatest dimension.
d Most pleural (pericardial) effusions with lung cancer are due to tumor. In a few patients, however, multiple microscopic examinations of pleural (pericardial) fluid are negative for tumor and the fluid is nonbloody and not an exudate. When these elements and clinical judgment dictate that the effusion is not related to the tumor, the effusion should be excluded as a staging descriptor.
e This includes involvement of a single distant (nonregional) lymph node.
| Occult Carcinoma | TX | N0 | M0 |
|---|---|---|---|
| Stage 0 | Tis | N0 | M0 |
| Stage IA1 | T1a(mi) | N0 | M0 |
| T1a | N0 | M0 | |
| Stage IA2 | T1b | N0 | M0 |
| Stage IA3 | T1c | N0 | M0 |
| Stage IB | T2a | N0 | M0 |
| Stage IIA | T2b | N0 | M0 |
| Stage IIB | T1a-c | N1 | M0 |
| T2a | N1 | M0 | |
| T2b | N1 | M0 | |
| T3 | N0 | M0 | |
| Stage IIIA | T1a-c | N2 | M0 |
| T2a–b | N2 | M0 | |
| T3 | N1 | M0 | |
| T4 | N0 | M0 | |
| T4 | N1 | M0 | |
| Stage IIIB | T1a-c | N3 | M0 |
| T2a–b | N3 | M0 | |
| T3 | N3 | M0 | |
| T4 | N2 | M0 | |
| Stage IIIC | T3 | N3 | M0 |
| T4 | N3 | M0 | |
| Stage IVA | Any T | Any N | M1a |
| Any T | Any N | M1b | |
| Stage IVB | Any T | Any N | M1c |
| Lymph Node Station No. | Anatomic Limits |
|---|---|
| Supraclavicular Zone | |
|
|
| Upper Zone | |
|
|
|
|
|
|
| Aortopulmonary Zone | |
|
|
|
|
| Subcarinal Zone | |
|
|
| Lower Zone | |
|
|
|
|
| Hilar/Interlobar Zone | |
|
|
|
|
| Peripheral Zone | |
|
Adjacent to the lobar bronchi |
|
Adjacent to the segmental bronchi |
|
Adjacent to the subsegmental bronchi |

In the eighth edition of the IASLC/AJCC, lung cancer staging project significant innovations were introduced into the definitions of the T descriptor. In particular, the eighth edition includes for the first time special definitions for carcinoma in situ (Tis) and for minimally invasive carcinomas (T1mi). Tis are less than 3-cm noninvasive tumors that histologically display a pure lepidic growth pattern. T1mi are less than 3-cm tumors that histologically display a predominant lepidic growth pattern; however, they also have a small (<0.5-cm) invasive component. In addition, the definitions of the four classic lung cancer T categories (T1–T4) have also been refined. In the current edition, T1 tumors (<3 cm) are subcategorized as T1a <1 cm, T1b >1 to 2 cm, T1c >2 to 3 cm. T2 tumors (>3 to 5 cm) are subcategorized as T2a >3 to 4 cm, T2b >4 to 5 cm. T3 tumors are defined as >5 up to 7 cm and T4 tumors are defined as >7 cm. Other important tumor characteristics that dictate the T stage are involvement of the main bronchus/invasion of the visceral pleural/associated lobar or lung atelectasis in the T2 descriptor, invasion of the parietal pleura/chest wall/phrenic nerve/parietal pericardium or associated separate tumor nodule(s) in the same lobe as the primary tumor in the T3 descriptor, and invasion of the diaphragm/mediastinum/heart/great vessels/trachea/recurrent laryngeal nerve/esophagus/vertebral body/carina or separate tumor nodule(s) in a different ipsilateral lobe to that of the primary tumor in the T4 descriptor. Contrast-enhanced CT of the chest is the main imaging modality used to determine the T stage. MRI of the chest wall may assist in identifying chest wall involvement and in staging of superior sulcus tumors.
The node descriptor (N0–N3) is defined according to the extent of lymph node metastasis along a predefined lymph node map. There are 14 lymph node stations: stations 10 to 14 are confined to the lung, and metastasis to these nodes indicates N1 disease if ipsilateral to the tumor and N3 disease if contralateral to the tumor; stations 9 to 2 are confined to the mediastinum, and metastasis to these nodes indicates N2 disease if ipsilateral to the tumor and N3 disease if contralateral to the tumor; station 1 are supraclavicular or suprasternal or low cervical nodes, and metastasis to these nodes indicates N3 disease. The nodal characteristics and designations did not change in the eighth edition of the IASLC lung cancer staging project. However, a recommendation is made to define nodal involvement not only by the N0 to N3 descriptors, but also by quantifying the number of involved lymph nodes. In particular, nodal quantification by the number of involved nodal stations is defined as follows: N1a: involvement of a single N1 nodal station; N1b: involvement of multiple N1 nodal stations; N2a1: involvement of a single N2 nodal station without N1 involvement (skip metastasis); N2a2: involvement of a single N2 nodal station with N1 involvement; and N2b: involvement of multiple N2 nodal stations. Prognosis worsens as the number of involved nodal stations increases, but N1b and N2a1 have the same prognosis. Asamura and colleagues have shown that the five-year survival rates in the population of patients who underwent complete resection for the different N subcategories were: N1a, 59%; N1b, 50%; N2a1, 54%; N2a2, 43%; and N2b, 38%. FDG-PET combined with contrast-enhanced CT is the main imaging modality used to determine the N stage. Hilar and mediastinal nodes that are suspected to be involved by cancer (>1 cm) or have positive FDG uptake are in the majority of cases sampled to confirm tumor metastasis.
The eighth edition of lung cancer stating system has refined the categorization of the M descriptor. It defines two M descriptors, M0 and M1, with M1 being subcategorized to M1a, M1b, and M1c. M1a indicates endothoracic metastasis (malignant pleural/pericardial effusion or malignant pleural/pericardial nodules or separate tumor nodule in a contralateral lobe). M1b indicates the presence of a single extrathoracic metastasis in a single organ. M1c indicates the presence of a multiple extrathoracic metastases in a single organ or in multiple organs. Remarkably, M1a and M1b tumors have similar prognosis; however, since they represent different forms of metastatic involvement and require different diagnostics and therapeutics, they were separately categorized. FDG-PET combined with contrast-enhanced CT is the main imaging modality used to determine the M stage. Brain MRI is used to identify brain metastasis. Suspected metastatic lesions may be samples in order to confirm NSCLC diagnosis or if biopsy results will alter the treatment plan. Otherwise routine sampling of metastatic lesions in not performed.
The eighth edition of lung cancer stating system has refined and expanded the lung cancer stage definitions to produce a more precise tool to predict prognosis and guide treatment plan ( Fig. 58.15 ).

The choice of initial therapy (whether single-modality or multimodality therapy) depends on the patient’s clinical stage at presentation and on his or her functional class and comorbidities. Treatment options may vary, even among different subsets of patients within the same clinical stage. Pretreatment staging is the critical step before initiating therapy. With current efforts, 5-year survival rates by pathologic stage are 90% for stage IA1, 85% for stage IA2, 80% for stage IA3, 73% for stage IB, 65% for stage IIA, 56% for stage IIB, 41% for stage IIIA, 24% for stage IIIB, and 12% for stage IIIB. The 5-year survival rates by clinical stage are 13% for stage IVA and 0% for stage IVB. Treatment for lung cancer can broadly be grouped into three major categories, as follows:
Stage I disease and stage II disease indicate the presence of tumor that is contained within the lung and that may be completely resected with surgery. Anatomic resection of the lobe where the tumor resides with complete sampling of mediastinal lymph nodes is the treatment of choice. The key aim of this treatment approach is to achieve complete resection of the tumor and its intralobar draining lymph nodes. In certain cases, sublobar anatomic resections may be considered for small and peripheral tumors. Nonanatomic resections (wedge resection) are considered inferior to anatomic resection and should be performed only when more extensive surgery cannot be tolerated by the patient (due to reduced pulmonary reserve for example). Stereotactic body radiation therapy (SBRT) has had good early results (local control rates of 90% at 3 years) in selected patients that cannot withstand surgical resection.
Stage IV disease (metastatic disease) and stage IIIB disease (advanced disease presenting either as a relatively small tumor with N3 nodes or as a large tumors with N2 nodes) are not typically treated by surgery except in patients requiring surgical palliation. Systemic therapies for metastatic disease are common. Chemoradiation is often used in stage IIIB disease. Targeted therapies and immunotherapy are providing encouraging results in properly screened and selected patient groups.
Stage IIIA lung cancer indicates a locally advanced disease that may have a wide spectrum of presentations. Remarkably, the majority of stage IIIA tumors are too advanced for consideration of resection; however, if complete resection is deemed possible, it may be associated with improved outcomes. In this clinical scenario, surgical resection is performed as part of a multimodality treatment protocol. In particular, resectable stage IIIA tumors are either small tumors that present with a low metastatic burden to the ipsilateral mediastinal (N2) lymph nodes or larger tumors that do not involve mediastinal lymph nodes (T4N0/1M0). These tumors, by their advanced nature, may be mechanically removed with surgery; however, surgery does not consistently control the micrometastases that exist within the general area of the operation or systemically. Combinations of chemotherapy and radiotherapy, and in recent years also immunotherapy, are used for locally advanced disease either in the adjuvant or neoadjuvant settings. A multidisciplinary team of experts usually predefines the desired treatment plan in each case.
More broadly, lung carcinoma should be resected when the local disease can be controlled, the patient’s physical condition can tolerate the planned resection and reconstruction, and the anticipated operative morbidity and mortality are reasonable. Conditions such as superior vena cava syndrome, tumor invasion across the mediastinum into the main pulmonary artery, N3 nodal metastases, malignant pleural or pericardial disease, or extrathoracic metastases carry greater risk than benefit for resection in most patients. Some centers have had good results with resection and reconstruction of the trachea, atrium, great vessels, or other mediastinal or vertebral structures. These are complex operations requiring dedicated multidisciplinary teams during the preoperative phase and multispecialty teams in the operating room. Patients with tracheoesophageal fistula have a limited life expectancy, and palliative care with stent placement would be recommended.
Stages I and II NSCLC can be treated safely with surgery and mediastinal lymph node dissection alone, and most patients have long-term survival. Anatomic resection with lobectomy, with systematic mediastinal lymph node dissection/sampling, is the procedure of choice for lung cancer confined to one lobe ( Fig. 58.16 ). The American College of Surgeons Oncology Group defined a systematic sampling strategy for specific mediastinal lymph nodes. At a minimum, samples of nodal (not adipose) tissue from stations 2R, 4R, 7, 8, and 9 for right-sided cancers and stations 4L, 5, 6, 7, 8, and 9 for left-sided cancers should be obtained. Mediastinal lymphadenectomy should include exploration and removal of lymph nodes from stations 2R, 4R, 7, 8, and 9 for right-sided cancers and stations 4L, 5, 6, 7, 8, and 9 for left-sided cancers.

Lesser operations, such as wedge resection or segmentectomy, may be considered for patients at greater risk for lobectomy. Segmentectomy may be appropriate in patients with peripheral small tumors that have a low metabolic activity on PET-CT. A retrospective propensity matched analysis comparing segmentectomy to lobectomy in stage I lung cancer has shown that at a mean follow-up of 5.4 years, comparing segmentectomy with lobectomy, no differences were noted in locoregional (5.5% vs. 5.1%, respectively; P = 1.00), distant (14.8% vs. 11.6%, respectively; P = 0.29), or overall recurrence rates (20.2% vs. 16.7%, respectively; P = 0.30). Furthermore, when comparing segmentectomy with lobectomy, no significant differences were noted in 5-year freedom from recurrence (70% vs. 71%, respectively; P = 0.467) or 5-year survival (54% vs. 60%, respectively; P = 0.258). Patients with NSCLC that invades into the chest wall may undergo resection with lobectomy with en-bloc chest wall resection.
SBRT is another local control modality that may be applied in patients who are medically inoperable. Radiation dose and the number of fractions are determined according to tumor location and size. In general, SBRT is well tolerated with good early results. Prospective clinical trials have shown local control and overall survival rates with SBRT to be more than 85% and about 60% at 3 years (median survival, 4 years), respectively. Novel radiation protocols use advanced technologies to better plan and direct radiation delivery to the tumor while minimizing damage to the surrounding tissues.
Advanced stage lung cancer, particularly with extensive nodal spread, cannot typically be considered a disease effectively treated with a single modality. Survival after resection may be improved in selected patients with adjuvant chemotherapy. The International Adjuvant Lung Trial enrolled 1,867 patients with completely resected stage I to III NSCLC. These patients were randomly assigned to observation or chemotherapy. Radiation therapy was at the discretion of the institution. The treatment group received one of four cisplatin-based doublet adjuvant regimens. Survival was increased 5% in the adjuvant chemotherapy group. Consequently, all patients staged IB and IIB should be considered for adjuvant chemotherapy after resection.
Surgery alone for stage IIIA (N2), IIIB, or IV lung cancer is infrequently performed; however, selected patients may benefit from a multidisciplinary approach to treatment. Resection for isolated brain metastasis is warranted for improvement in symptoms, quality of life, and survival rate. The primary lung tumor can be treated according to T and N stage. Additional treatment beyond resection is needed.
Even with complete resection, patients with resectable NSCLC have poor survival. Preoperative therapy (induction/neoadjuvant) has been evaluated: preoperative paclitaxel and carboplatin followed by surgery was compared with surgery alone in patients with stage IB to IIIA NSCLC without N2 involvement. Overall survival (62 months vs. 41 months) and progression-free (33 months vs. 20 months) survival were higher with preoperative chemotherapy, although the differences did not reach statistical significance. Further, a metaanalysis of randomized clinical trials evaluating preoperative chemotherapy in resectable NSCLCs has indicated that the overall survival of NSCLC patients receiving neoadjuvant chemotherapy was significantly improved compared to those in who had surgery alone (hazard ratio [HR] 0.84; 95% CI, 0.77–0.92; P = 0.0001). Other studies have shown that the benefit from preoperative chemotherapy is similar to that attained with postoperative chemotherapy. These results further confirm the recognition that operable NSCLC patients with disease stage IB or higher should be considered for preoperative chemotherapy. Induction chemoradiotherapy has been evaluated for treatment of clinical stage IIIA (N2) NSCLC. In one phase III trial, concurrent chemotherapy and radiotherapy followed by resection was compared with standard concurrent chemotherapy and definitive radiotherapy without resection. The median overall survival was similar in both groups (∼23 months). Progression-free survival was better in the surgery group (12.8 months median vs. 10.5 months; P = 0.017). The authors reported pneumonectomy was associated with poor outcomes. In an exploratory analysis, overall survival was improved for patients who were found to have undergone induction chemoradiotherapy and lobectomy. In selected patients with resectable stage IIIA NSCLC, induction chemoradiotherapy followed by resection is an alternative treatment to chemoradiotherapy alone. Patients with local extension of lung cancer at the apex of the lung into the thoracic inlet may have characteristics of shoulder and arm pain, Horner syndrome, and occasionally paresthesia in the ulnar nerve distribution of the hand (fourth and fifth fingers) ( Fig. 58.17 ). Patients with all these characteristics may be classified as having Pancoast syndrome. Pain comes from the C8 and T1 nerve roots. Sympathetic nerve involvement may result in Horner syndrome (miosis, ptosis, anhidrosis, and enophthalmos). Typically, the first, second, and third ribs are involved and require resection, but the bony spine and intraforaminal spaces can also be involved. MRI is necessary, in addition to CT, to plan the surgical procedure. Preoperative therapy includes chemoradiotherapy.

Metastatic disease (stage IV NSCLC) is usually incurable. Performance and quality of life decline. Patients and families should be informed of the diagnosis and potential outcomes of treatment. Treatment decisions should take into consideration the wishes of the patient and family, and realistic expectations should be set and monitored during therapy. Nevertheless, in recent years, a growing number of biologic and immunologic therapies have been approved for the treatment of advanced NSCLC. Utilization of such therapeutics and their incorporation into conventional anti NSCLC protocols (chemotherapy and radiation) has significantly expanded the therapeutic options for patients with advanced inoperable NSCLC (stages IV and IIIB). Modern NSCLC therapeutics is based on genetic and immunologic phenotyping of the tumor. Treatment is often tailored according to disease characteristics and according to the patients’ functional status. NSCLC tumors may be categorized as oncogene addicted, as highly sensitive to immunotherapy, and as tumors that are less likely to respond to either targeted or immunologic therapies ( Figs. 58.18 and 58.19 ). Oncogene addicted tumors are treated with specific small molecules and antibodies that target key NSCLC driving mutations (epidermal growth factor receptor [EGFR], BRAF, ALK, ROS, and MET). Resistance to such therapies eventually develops; however, newer and more efficient second line agents are continuously being developed. To illustrate, osimertinib a novel EGFR tyrosine kinase inhibitor (TKI) had significantly greater efficacy than platinum therapy plus pemetrexed in patients with T790M-positive (a mutation conferring resistance to first line EGFR TKI) advanced NSCLC (including those with CNS metastases) in whom disease had progressed during first-line EGFR-TKI therapy (progression-free survival of (10.1 months vs. 4.4 months; HR 0.30; 95% CI, 0.23–0.41; P < 0.001). Tumors that are considered to be highly sensitive to immunotherapy are treated with immune checkpoint inhibitors that block the PD-1/PD-L1 and CTLA4/CD80/CD86 pathways. In particular, immunotherapy is effective against tumors that express high levels of the immune inhibitory molecule PD-L1, against tumors that have a high mutational burden (as seen in smoke induced NSCLC), and against tumors that have defective DNA repair mechanisms. To illustrate, in patients with advanced NSCLC and PD-L1 expression on at least 50% of tumor cells, pembrolizumab (an anti PD-1 antibody) was associated with significantly longer progression-free and overall survival and with fewer adverse events than was platinum-based chemotherapy (median progression-free survival was 10.3 months; 95% CI, 6.7 to not reached) in the pembrolizumab group versus 6.0 months (95% CI, 4.2–6.2) in the chemotherapy group (HR for disease progression or death, 0.50; 95% CI, 0.37–0.68; P < 0.001). NSCLC tumors that are less likely to respond to either targeted or immunologic therapies are treated with conventional chemotherapy (therapeutics for squamous and nonsquamous NSCLC slightly differ). Platinum-based combinations produce 1-year survival rates of 30% to 40% and are more efficacious than single agents. In the United States, for patients with good functional status, frequently used initial cytotoxic regimens for nonsquamous NSCLC include: 1) cisplatin (or carboplatin)/pemetrexed or 2) carboplatin/paclitaxel with (or without) bevacizumab. Gemcitabine/cisplatin is recommended for patients with either SCC or nonsquamous NSCLC. More recently combination of immunotherapy with chemotherapy have shown promising anti-NSCLC effects even in subgroups of patients whose tumors where less likely to respond to immunotherapy. The side-effect profile of chemotherapy and immunotherapy significantly differs. Autoimmunity it the leading cause for treatment discontinuation in patients that receive immunotherapy while systemic toxicity is the leading cause for treatment discontinuation in patients that receive chemotherapy.


Quality-of-life issues arise in patients with metastatic NSCLC. Dyspnea from MPE, superior vena cava syndrome, tracheoesophageal fistula, bone metastases, and pain occur. Nutrition and hydration are significant issues. Palliation from symptoms may be accomplished with good results. For MPE associated dyspnea, insertion of a tunneled indwelling pleural catheter such as the pleurX drainage systems is indicated.
The trachea is a semi-flexible tube of 1.5 to 2 cm in width and 10 to 13 cm in length, reaching from the lower portion of the larynx at the level of the sixth to seventh cervical vertebra to the fourth to fifth thoracic vertebra, where it bifurcates to form the two bronchi for the lungs.
The location of the carina is at the level of the angle of Louis anteriorly and the T4 vertebra posteriorly. The tracheal wall consists of up to 20 incomplete rings of hyaline cartilage forming the anterior and lateral circumference, and smooth muscle at the posterior side, which are both embedded into a fibrous membrane of elastic connective tissue.
Its major physiologic role is to conduct air between the larynx and the bronchi, exchange heat and moisture and remove particles. The transport of air is critically dependent on the inner diameter of the trachea. Mucosal swelling, constriction of airway muscles, or tumors that reduce the airway space, but also endotracheal tubes, considerably increase the resistance to airflow: a 50% reduction of the inner diameter increases the resistance sixteenfold, and during turbulent flow up to thirty-twofold. During inspiration, the upper airways warm and humidify the inspired air. This process is very efficient. During quiet breathing at room temperature, air is completely warmed up to 37°C and humidified to 100% saturation shortly distal of the bifurcation; this is called the isothermal saturation point. Tracheobronchial glands produce a mucin-rich secretion that forms a protective barrier between the epithelium and the environment. This secretion is largely controlled by the autonomic nervous system. The mucus collects debris and microorganisms and is transported orally by the mechanical forces of coordinated ciliary beating and the airflow during expiration.
Stenosis of the trachea implies significant functional impairment. A normal 2 cm trachea has a 100% peak expiratory flow rate. A 10 mm opening provides an 80% peak expiratory flow rate. At 5 to 6 mm, only a 30% expiratory flow rate is obtained. Benign stenosis of trachea results mainly from tracheotomy, ventilation, or trauma. Tracheotomy leads to a transmural defect of the ventral part of the cervical trachea. The tracheotomy wound is colonized by bacteria with local necrosis by mechanical alteration. After removal of the tracheostomy tube, the defect is closed by the secondary scar tissue healing, which tends to contract. This process of healing results in an A-shaped stenosis of the trachea ( Fig. 58.20 ). The severity of shrinkage depends on the extension of the defect, necrosis, and infection. Low-volume, high-pressure cuffs of ventilation tubes induce circular necrosis of the tracheal mucosa. Depending on the pressure, the duration of ischemia, and local infection, the underlying cartilages may be bare, necrotic, and destroyed. Mucosal defects without infection can be recovered from surrounding epithelium without relevant morbidity. Deeper destruction and infection of the tracheal wall leads to a ring of granulation tissue forming a sand-glass stenosis. Cuff-induced stenosis appears in the middle part of the trachea. The introduction of low-pressure, high-volume cuffs make this kind of tracheal stenosis a rare disease.

Symptoms of tracheal obstruction can occur immediately after extubation or slowly over several years. Clinical signs like stridor and dyspnea appear when the lumen is obliterated by more than 50%; however, clinical signs and lung function testing are not very sensitive or specific for tracheal stenosis. Standard of treatment for symptomatic patients consists of resection of the pathologic segment of the trachea with end-to-end anastomosis. In case of involvement of the larynx, partial resections of the anterior cricoid cartilage or division of the larynx with tracheolaryngeal silicone stents is used. Short-term and long-term results are satisfying.
Most tumors of the trachea in adult patients are malignant, with approximately one half to two thirds being SCCs; adenoid cystic carcinomas (ACCs) were the second most common, accounting for approximately 10% to 15% of cases. Less common primary tracheal tumors include mucoepidermoid carcinoma, nonsquamous cell bronchogenic carcinomas, sarcomas, carcinoid tumors, and pleomorphic adenoma. Benign tracheal lesions include hemangioma, hamartoma, neurogenic tumors, granular cell tumor, and squamous papillomas. Rather than being primary tracheal tumors, the majority of tracheal tumors occur via direct invasion of the trachea from carcinoma of the lung, esophagus, larynx, or thyroid gland. Hematogenous tracheal metastases have been described in patients with carcinoma of the breast, colon, and kidney, as well as those with melanoma.
SCCs are the most common histopathologic type of tracheal malignancy. Up to 10% can be multifocal. Tumors may arise as an intraluminal nodule and progress to include mediastinal extension or lymph node metastases and may lead to stenosis or tracheoesophageal fistula. They are histologically identical to SCCs of the lung.
ACCs, previously called cylindroma, of the tracheobronchial tree are well-differentiated, slow-growing neoplasms. ACCs typically form polypoid lesions in the trachea or main stem bronchi, but they may form infiltrative plaques with longitudinal or circumferential extension and often breach the cartilaginous plate. Perineural invasion and extension along vascular structures is very common and accounts for the high rate of positive surgical margins, well beyond the gross limits of the tumor. ACCs can have multiple recurrences with late metastases. They are histologically identical to ACCs of the salivary glands.
The most common presenting symptoms of tracheal tumors are due to the presence of a mass within the trachea. These symptoms frequently do not arise until the tumor is large enough to obstruct at least 50% of the diameter of the lumen. Symptoms vary based on the location of the tumor as well as the histologic subtype.
SCCs often present with hemoptysis, given mucosal irritation and ulceration, and are typically diagnosed within four to six months of symptom onset. Dysphagia and hoarseness may also be present. The peak incidence is in the sixth to seventh decade of life. These tumors are seen primarily in smokers.
ACC commonly presents with wheezing or exertional dyspnea, with hemoptysis present in only a minority of cases. Diagnosis is established on average 18 months after symptom presentation. The peak incidence occurs in the fourth and fifth decade of life. It affects men and women equally and usually affects nonsmokers. Low-grade tumors, such as mucoepidermoid carcinomas or benign tumors, may be asymptomatic for years before diagnosis.
The diagnosis of tracheal tumors is often delayed due to similar presenting symptoms with other etiologies, including asthma, COPD, and pneumonia. Chest CT is typically ordered for patients in whom a tracheal pathology is suspected. This study may reveal polypoid lesions, focal stenosis, eccentric narrowing, or circumferential wall thickening. Bronchoscopy is mandatory to obtain a tissue diagnosis and to differentiate between benign and malignant tumors. PET/CT may be useful for staging the cancer, but data on tracheal tumors are limited. Preoperative PET/CT scans may help to assess extent of disease and resectability, particularly for SCC.
The primary treatment modalities for tracheal tumors are surgery and radiation therapy; there are no randomized trials directing the most efficacious treatment approach. The outcome of treatment depends on the stage, as well as the histology of the tracheal tumor. Complete surgical resection is the treatment of choice for malignant tracheal tumors whenever possible, given retrospective data suggesting improved disease outcomes and acceptable postoperative morbidity. Because of the lack of suitable replacement material, the suggested maximum resected length of trachea is 5 cm. Available data suggest that postoperative radiotherapy improves survival for patients with incompletely resected squamous SCC and ACC, but not for those with completely resected tumors. For patients with unresectable, nonmetastatic SCC or ACC, concurrent chemoradiotherapy with a platinum-based regimen may be attempted, though data are limited.
Involvement of the trachea because of local extension from bronchogenic carcinoma may contraindicate resection. Involvement of the trachea because of local extension of esophageal carcinoma may require palliative therapy or stent placement.
Blunt or penetrating injuries of the tracheobronchial tree are most often accompanied by a variety of different and sometimes life-threatening injuries. Almost 75% to 80% of penetrating injuries involve the cervical trachea, whereas 75% to 80% of blunt injuries occur within 2.5 cm of the carina and 40% occur within the first 2 cm of the right main bronchus.
Blunt or penetrating trauma to the neck or trachea can produce lacerations, transections, or shattering injuries of both the cervical and the mediastinal trachea. Blunt trachea-bronchial injuries are associated with major accompanying injuries in 40% to 100% of cases, primarily involving orthopedic, facial, pulmonary, and intraabdominal injuries. Major associated injuries, mainly of the esophagus and great vessels, were reported in 50% to 80% of penetrating injuries.
Tachypnea and subcutaneous emphysema are the most common clinical signs. Other signs include air escaping from the neck wound, massive air leak after placement of a tube thoracostomy, hemoptysis, stridor, and dysphagia. Chest roentgenogram and chest CT scan are the first step in diagnosis. Paratracheal air, deep cervical emphysema, and pneumomediastinum are common findings. Associated injuries include pneumothorax/hemothorax, ribs fractures, pulmonary contusion, laryngeal fracture, esophageal injury, cervical spine, and great vessels injuries. Bronchoscopy is the most important procedure to exactly locate and assess trachea-bronchial injuries. Early airway assessment followed by definitive airway protection is the key to neck trauma management and trachea-bronchial injuries. Concurrent esophageal injury needs to be excluded by barium esophagography or esophagoscopy. Anesthetic management with laryngeal mask airway may be helpful for initial examination for full visualization of the airway before endotracheal intubation.
Patients with blunt trauma and small injuries or no appreciable air leaks, who do not require positive pressure ventilation and are nonprogressive, may be treated nonoperatively with close monitoring. For all other cases, immediate exploration of neck wounds is crucial for survival because vascular and esophageal injuries are frequent and the tracheal injury often includes cartilages as well as ligamentous portions. Primary surgical repair represents the treatment of choice to reestablish airway continuity. Bronchial disruption may require thoracotomy for repair. Right thoracotomy provides excellent visualization of the carina and proximal left mainstem bronchus.
Acquired tracheoesophageal fistula can occur from cancer or from prolonged intubation with erosion posteriorly. Repair is with separation of the trachea and esophagus, repair of the fistulous tract, and interposition of normal tissue, such as muscle between the two structures.
Tracheoinnominate fistula may result from prolonged cuff erosion inferiorly and anteriorly in the trachea. Inappropriate low stoma may further increase the likelihood of a direct erosion of the trachea by the innominate artery. The tip of the endotracheal tube may predispose to erosions or granulomas within the trachea. Tracheoinnominate fistula may manifest with a sentinel hemorrhage before sudden exsanguinating hemorrhage. Investigation of these sentinel hemorrhage episodes is critical. Evaluation in the operating room may provide for optimal situational control should additional interventions be required.
Elective or emergent tracheal surgical procedures are typically performed to improve tracheal patency or repair loss of tracheal integrity. Anesthetic challenges include abnormal airway anatomy and physiology, likely requirements for specialized endotracheal tubes for initial airway management and additional airway devices to meet evolving intraoperative needs, and changes to alternative modes of ventilation if the trachea is open or obstructed.
General inhalational anesthesia is used, and induction may take a long time if the stenosis is tight. The patient should be maintained spontaneously breathing if possible. If the stenosis is less than 5 to 6 mm, dilation may be required before passing the endotracheal tube; the dilation may be performed with rigid bronchoscopy. If the stenosis is greater than 5 to 6 mm, the endotracheal tube may be positioned to a point above the stricture for induction. Stenoses that are subglottic must be dilated for intubation. The endotracheal tube often goes alongside tumors.
The cervical approach for tracheal resection is usually used for tumors of the upper half of the trachea plus all benign tracheal stenoses (because these usually occur as a result of endotracheal tube placement). Occasionally, an upper sternal split may be needed ( Fig. 58.21 ). The posterolateral thoracotomy (fourth interspace) is used for tumors of the lower half of the trachea plus carinal reconstruction. Rigid bronchoscopy for diagnosis, biopsy, dilation, or morcellation of tumor or other treatment may be required if the tumor cannot be immediately resected ( Fig. 58.22 ).


In general, the maximal amount of trachea that can be resected is approximately 5 cm, but this varies from person to person. Various techniques are used to mobilize the trachea to create a repair without undue tension on the anastomosis. The anterior cervical approach plus mobilization of the trachea and neck flexion can allow for 4 to 5 cm of trachea resection. A suprahyoid release may achieve 1 cm of additional length. Mobilization of the right hilum, together with division of the pericardium around the right hilum, may achieve an additional length.
Procedures to repair subglottic larynx or cricoid stenosis are technically challenging. The recurrent nerves innervate the larynx just superior to the posterolateral cricoid on each side. If the tracheal lesions involve only the anterior surface, the anterior cricoid can be removed and the distal trachea beveled to match the defect. This maneuver spares the recurrent laryngeal nerves. With circumferential involvement, it may be necessary to perform a laryngectomy.
Reconstruction of the lower trachea is performed in the right fourth intercostal space. Intubation of the distal trachea or the left main stem bronchus is performed. Carinal reconstruction is usually performed for tumor and is the most feasible of alternative reconstructions chosen.
Contraindications to trachea repair include (1) inadequately treated laryngeal problem (which does not include single vocal cord paralysis); (2) need for ventilatory support or permanent tracheostomy for patients with amyotrophic lateral sclerosis, myasthenia gravis, or quadriplegia; (3) use of high-dose steroids; and (4) inflamed or recent tracheostomy. Poor pulmonary reserve is not a contraindication for repair in patients who have been weaned from the ventilator.
Pulmonary infections requiring surgical interventions are infrequent compared with pleural space infections. Clinical features are similar to pneumonia, including fever, cough, leukocytosis, pleuritic pain, and sputum production. The patient is specifically questioned about aspiration of a foreign body. Evaluation includes CXR and CT scan of the chest and upper abdomen. Bronchoscopy can be performed to clear secretions and, when the diagnosis is suspected, to rule out cancer, foreign body, bronchial stenosis, or stricture. Cultures may be obtained to facilitate antibiotic treatment. Medical treatment is optimized; this includes discontinuation of smoking and institution of postural drainage, bronchodilator medications, and oral antibiotics.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here