Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Full range of motion (ROM) in the knee joint is critical for optimal function. A slight loss of knee motion can limit function and cause pain, and a more severe loss will lead to significant impairment and disability. For optimum function, the knee should have ROM and strength that is symmetric to the opposite, normal knee. When something causes a loss of normal knee motion, a cascade of events often follows, beginning with relative disuse of the involved lower extremity, increased pain, and subsequent loss of strength.
Loss of knee motion can occur for many reasons, including acute knee injury, lack of appropriate rehabilitation after a surgical procedure or injury, arthrofibrosis (which commonly occurs after anterior cruciate ligament [ACL] reconstruction or lower extremity fractures), relative disuse due to injury or degenerative joint disease, displaced bucket-handle meniscus tears, or mucoid degeneration of the ACL or posterior cruciate ligament (PCL). Clinicians should be vigilant about detecting loss of ROM of the knee in any patient with knee pain or injury because by restoring normal, symmetric knee motion first, followed by restoring symmetric strength, many symptoms may subside or abate, negating the need for further surgical intervention. Use of this proactive approach helps patients avoid problems in the short term after a knee injury or surgery, and some evidence indicates that it may also prevent long-term problems, including knee osteoarthritis.
Early intervention for ROM loss requires early detection. To identify loss of knee motion, the opposite, normal knee must also be examined to establish a baseline for comparison, and the examination must include an assessment of knee hyperextension. Unfortunately this step is sometimes overlooked. A recent study found that in patients who were seeking a second opinion for their knee problem, only 37% reported having their opposite, normal knee physically touched during the physical examination.
This chapter provides an overview of the diagnosis and treatment for loss of ROM of the knee. The reasons for loss of knee motion and thus the treatments are wide ranging. However, common themes regarding effective treatment remain the same regardless of the specific cause of loss of knee motion. Most cases of loss of knee motion can be effectively treated without surgery if proper rehabilitation is performed. In some cases, such as arthrofibrosis or displaced bucket-handle meniscus tears, surgical intervention is necessary to remove a mechanical block to knee ROM. The surgical treatment for arthrofibrosis after ACL reconstruction is outlined in detail in this chapter. The principles of rehabilitation for loss of knee motion remain the same whether or not surgical intervention is a part of the treatment plan, and these rehabilitation principles are also discussed.
Patients with loss of knee motion may present with varying subjective histories. It is important to determine how long the ROM loss has been present. This information can be difficult to elicit because patients are often unaware that their ROM is lacking, so we ask them how long they have felt that they had a bad knee. Generally speaking, the longer the ROM loss has been present, the more slowly it may respond to treatment. However, long-term ROM loss does not always mean that more aggressive forms of treatment are necessary; rather, it is important for both the clinician and patient to understand that progress may occur at a slower pace.
In patients who have had previous knee surgery, it is important to obtain pertinent details about the surgical procedure. When loss of motion is present, it is perhaps even more important to ascertain what, if any, pre- and postoperative rehabilitation was performed. In our experience, many patients with persistent pain after a knee arthroscopy or other knee surgery have loss of knee motion that was likely present before surgical intervention but was overlooked and not treated.
In patients who have not had a previous knee surgery, a careful subjective history can often identify a precipitating injury that may not have seemed significant at the time but may have led them to begin favoring their knee. When patients favor a knee, they stand with their weight shifted away from the involved lower extremity, holding the knee slightly bent. Over time, this habit slowly leads to increasing amounts of knee extension loss. Without full terminal knee extension, it is not comfortable to stand with the body weight shifted toward the involved knee because the ability to “lock out” the knee is lost, and therefore the quadriceps muscles cannot be relaxed during stance as it is for the opposite, normal knee. This scenario feeds the vicious cycle of disuse, increased pain, and further loss of strength.
Other times the subjective history reveals a significant injury to which the patient can attribute the ROM loss with certainty. A displaced bucket-handle meniscus tear blocks the intercondylar notch, resulting in the inability to fully extend the knee. Although this scenario may not always be caused by a specific injury, patients can usually identify exactly when this mechanism occurred and report that the involved knee feels “locked.”
When a patient does not have a history of a specific injury, the ROM loss may be associated with degenerative joint disease. Another potential cause of ROM loss is mucoid degeneration of the cruciate ligaments, most commonly the ACL. This pathology presents as a gradual loss of knee flexion combined with posterolateral knee pain. An effusion is usually not present.
The physical examination for any knee problem should include a careful assessment of the knee ROM of both knees, including an assessment of knee hyperextension. The uninvolved knee should always be examined before the involved knee; this examination is important to establish a baseline of what the ROM should be for the involved knee. It is also important that both knees be fully exposed (to the level of the midthigh) for the examination.
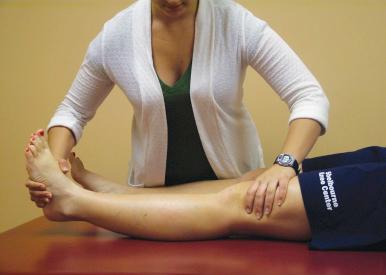
Knee extension (including hyperextension) is assessed in two ways. First, the examiner performs a passive assessment of hyperextension ( Fig. 108.1 ). The examiner stabilizes the thigh on the examination table with one hand while the other hand passively lifts the heel off the table, assessing the amount of movement available and the quality of the end feel. When ROM is limited, the patient should be asked if the discomfort is perceived posteriorly or anteriorly when a stretch is applied. Posterior discomfort indicates capsular and soft tissue tightness, whereas anterior discomfort may indicate an intra-articular mechanical blockage. Second, knee extension should be measured with the patient lying supine, with both heels propped up on a 6- to 8-inch bolster, allowing the knees to fall into hyperextension. This position allows for visual assessment of knee extension symmetry as well as goniometric measurement of knee extension.
It is important to note that knee hyperextension is normal. DeCarlo and Sell studied a group of healthy young athletes and found that 95% of males and 96% of females have some degree of knee hyperextension. The mean knee hyperextension was 5 degrees for males and 6 degrees for females. Therefore treatment to restore normal knee ROM should include restoration of hyperextension when it is present in the opposite knee.
Knee flexion is assessed with the patient lying supine or in a long-sitting position. The patient should be asked to grasp the front of his or her ankle with both hands (or use a towel looped around this area if necessary) and to pull the heel as far as possible toward the buttocks. Goniometric measurement can be made once maximal flexion is reached. Another method for assessing knee flexion is to ask the patient to sit on his or her heels ( Fig. 108.2 ). Patients with full flexion of both knees are able to comfortably sit back onto their heels without any pelvic tilt. Knee flexion loss leads to minor to severe tilting of the pelvis away from the involved extremity. This method of assessing flexion is also very helpful for patients in self-assessing their knee flexion and adjusting their activity levels accordingly.

For the purposes of this chapter, we focus on the examination for ROM deficits, but a full knee examination should also be performed, including observation of gait, observation for disuse of the lower extremity in arising from a chair or with habitual standing postures, observation of patella alignment and mobility, palpation for crepitus, assessment for a joint effusion, and special testing for meniscal pathology and ligamentous laxity.
Bilateral radiographs—including weight-bearing posteroanterior, lateral, and Merchant views—are routinely obtained. Again, even in the absence of bilateral symptoms, it is important to obtain bilateral radiographs to provide a baseline for comparison with the involved knee.
When osteoarthritis is suspected, we also recommend obtaining an anteroposterior view. A study by Rosenberg and colleagues showed that the posteroanterior view is more sensitive for detecting joint space narrowing of the tibiofemoral joint. This view is more sensitive because it is taken with the knees bent to a 45-degree angle, allowing for weight bearing with the tibiofemoral joint aligned in a position where more cartilage degeneration is likely. The anteroposterior view is not as sensitive for detecting joint space narrowing but provides information regarding the amount of joint space remaining when the knee is in a fully extended position.
In cases of long-standing ROM loss, the Merchant view radiograph can provide useful information through a visual comparison of the bone density of the patellae. When a patient has been favoring one knee for any considerable length of time, disuse osteopenia is evident on the Merchant view ( Fig. 108.3 ).

In patients with severe ROM loss, it is important to observe for signs of patella baja on the lateral-view radiographs. Again, comparison with the opposite knee is important to determine the height of the patella compared with Blumensaat's line and the apparent length of the patellar tendon based on measurements from the inferior pole of the patella to the tibial tubercle. Although normal ranges have been established for each of these measurements, what is normal for each patient varies and should be based on the measurements for the uninvolved knee.
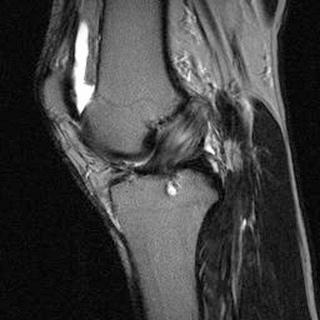
Magnetic resonance imaging (MRI) is useful when arthrofibrosis is present. In patients with arthrofibrosis types 1 or 2, the MRI can help identify the presence of a cyclops lesion, which is commonly present in patients with arthrofibrosis after ACL reconstruction. In persons with arthrofibrosis types 3 or 4, the MRI provides valuable insight about the extent of scar tissue formation in the fat pad.
Despite the wide range of pathologies that can cause limited knee ROM, a vast majority of cases of limited knee motion can be effectively treated with a directed rehabilitation program. One exception to this is in the case of a displaced bucket-handle meniscus tear, which would need to be arthroscopically reduced and removed or repaired.
Another condition to consider is arthrofibrosis, particularly in patients who have had previous knee surgeries, including ACL reconstruction, but also fractures around the knee. Arthrofibrosis is an abnormal proliferation of fibrotic tissue in the knee joint. The fibrotic tissue is commonly found in the extrasynovial space anteriorly in a fibrotic fat pad or near the intercondylar notch, presenting as a cyclops lesion at the base of the reconstructed ACL. Arthrofibrosis can cause a loss of knee extension alone, or knee extension and flexion may both be limited. Shelbourne et al. developed a classification for arthrofibrosis to help guide treatment ( Table 108.1 ). Most patients with type 1 arthrofibrosis respond to nonoperative rehabilitation and do not need surgery, but most cases of types 2, 3, or 4 require a combination of rehabilitation and operative treatment to achieve satisfactory results. In these patients, pre- and postoperative rehabilitation is a vital component of the treatment process. In nearly all other cases of knee ROM loss that were not caused by a previous surgery, a directed rehabilitation program completed under the supervision of a well-trained knee therapist can resolve significant deficits and provide a corresponding improvement in function.
| Type | Knee Flexion | Knee Extension | Other Features |
|---|---|---|---|
| 1 | Normal | ≤10-degree deficit a | Able to fully extend with overpressure |
| 2 | Normal | >10-degree deficit a | Unable to fully extend with overpressure |
| 3 | ≥25-degree deficit a | >10-degree deficit a | Decreased medial/lateral patellar mobility |
| 4 | ≥30-degree deficit a | >10-degree deficit a | Patella infera evident on radiographs |
a All range of motion (ROM) deficits are based on comparison with the ROM of the normal, uninvolved knee.
Not all rehabilitation programs are designed the same way, but the foundation of a rehabilitation program for limited knee motion should be to work on regaining symmetry in three distinct, sequential phases: (1) knee extension, (2) knee flexion, and (3) knee strength. Our experience has shown us that these phases of rehabilitation should not overlap; rather, one should focus on only extension ROM until symmetry is restored, and then shift toward working on flexion ROM while maintaining full extension. Finally, once full ROM symmetry has been achieved, unilateral strengthening exercises should be initiated until strength symmetry is restored. This rehabilitation program is described in greater detail in the “ Authors’ Preferred Technique ” and “ Postoperative Management ” sections, further on.
If ROM progress plateaus before symmetric knee extension is achieved, surgical intervention may be needed to remove a mechanical blockage to extension. When degenerative joint disease is present, the mechanical blockage may be caused by an osteophyte on the anterior tibia or near the intercondylar notch.
Mucoid degeneration of the ACL is a rare condition but presents with a classic history. Patients with this condition are typically middle aged and report an insidious onset of gradual loss of knee flexion accompanied by posterolateral knee pain. Some loss of knee extension may be present, but it is usually mild and easily resolves with rehabilitation using either a towel stretch or a passive knee stretch device (Ideal Stretch, Park City, UT) ( Fig. 108.4 ). The appearance on MRI is often described as a “celery stalk” feature, with a striated appearance on T2-saturated images indicating fluid between the ACL fibers. An enlarged, bulbous area is usually present proximally ( Fig. 108.5 ). Literature on this topic is sparse and mostly includes case reports regarding débridement or resection of the ACL, but residual instability has been an undesirable aftereffect of this procedure. We have found that this condition responds favorably to oral or injected steroids and rehabilitation using the principles described in detail later in this chapter.

Nonsurgical treatment with a carefully planned rehabilitation program is the first line of treatment for most patients with loss of knee ROM. As discussed in the previous section, surgery may be necessary in some cases to allow full, symmetric ROM to be regained, particularly in cases of type 2, 3, or 4 arthrofibrosis after an ACL reconstruction or when a bucket-handle meniscus tear becomes displaced and is blocking the intercondylar notch.
The following surgical interventions have been described for loss of knee motion: anterior interval release, notchplasty and/or removal of a cyclops lesion, posterior capsular release, peripatellar release, and manipulation with the patient under anesthesia.
The anterior interval is defined as the space posterior to the patellar tendon and extending to the anterior tibia and transverse meniscal ligament. Trauma to the infrapatellar fat pad can lead to fibrotic formation in this area of the knee, limiting both knee extension and flexion. This presentation is most commonly seen in patients who have undergone arthroscopic ACL surgery, with fat pad trauma occurring as a result of repeatedly passing instruments through the fat pad. Although arthroscopic ACL surgery is believed to be less traumatic for the patient, the trauma to the fat pad is underestimated. Fat pad trauma can lead to fat pad fibrosis; in its most severe form, fibrosis in this area can lead to infrapatellar contracture syndrome, which further limits patellar mobility and knee flexion. If full knee flexion is not emphasized immediately after surgery, patellar mobility decreases and permanent flexion deficits may occur. Anterior interval release can be performed arthroscopically with use of a 30-degree scope and portals that are slightly farther away from midline than usual to allow for better visualization of this area. Abnormal tissue may be removed with a basket forceps, meniscal shaver, or electrothermal probe.
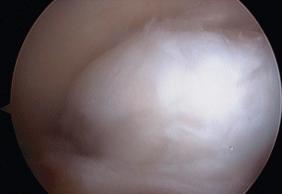
Under normal circumstances, the ACL and PCL fit perfectly within the intercondylar notch, completely occupying this space when the knee is in terminal extension. Occasionally after ACL reconstruction, a mismatch occurs between the size of the graft and the width of the intercondylar notch, or a cyclops lesion forms, blocking full knee extension. A cyclops lesion is a fibrous nodule that forms on the anterior aspect of the ACL graft ( Fig. 108.6 ). We theorize that this complication can be prevented after ACL reconstruction by ensuring that full, symmetric knee extension is restored prior to and immediately after surgery. These lesions can be carefully excised during arthroscopy until terminal extension is regained. If the intercondylar notch width is not adequate to handle the size of the ACL graft and the PCL, a notchplasty can also be performed.
When knee extension has been lacking for a longer duration of time, the posterior capsule becomes tight. Arthroscopic release of the posterior capsule has been described by LaPrade et al. and Mariani. Another option is to use a more aggressive approach to rehabilitation that focuses on knee extension by using a passive knee extension device (Elite Seat, AKT Medical, Inc., Noblesville, IN) ( Fig. 108.7 ). Use of a long-duration stretch of 10 to 15 minutes per session several times each day can eventually improve posterior capsular mobility and restore full knee extension compared with the opposite knee.

Decreased patellar mobility has been treated with release of the medial and/or lateral retinaculum and the suprapatellar pouch. Care must be taken to provide adequate release without overreleasing these structures and inducing patellar instability.
Manipulation with the patient under anesthesia has been described to regain knee extension and/or knee flexion. Manipulation of the knee can effectively improve knee motion, but it does not directly approach the knee problem selectively, and there is a risk of supracondylar femur fracture, patellar tendon rupture, and neurologic or vascular injury.
Many surgeons use more than one of these techniques in combination based on the location of the adhesions and the degree of ROM limitation that is present.
It is important to emphasize that surgical treatment is only one part of the process for treating loss of knee ROM and that surgical intervention is not always needed. For optimal results, patients must first maximize their knee ROM with a directed rehabilitation program. Then, if surgery is needed, a focused postoperative rehabilitation program is used to further maximize knee motion. In fact, we now require all patients undergoing surgery for arthrofibrosis to use a passive knee extension device (see Fig. 108.4 ) several times daily before and after surgery to maximize results. In past years, extension casting was used on the operating room table and followed by serial extension casting on an outpatient basis to provide a low-load, long-duration stretch; however, this treatment was difficult to implement because of the postoperative hemarthrosis that developed and the frequency of outpatient visits required for serial casting. Instead, we now have the patient perform several stretching sessions each day in the passive knee extension device and have found that this technique is highly effective and more cost- and time-efficient.
When surgical intervention is needed to treat arthrofibrosis, the lead author uses a stepwise process to address the specific areas of fibrosis that have developed in the knee. This section addresses the surgical treatment of arthrofibrosis, specifically arthrofibrosis that develops after ACL reconstruction. This approach is based on the classification of arthrofibrosis shown in Table 108.1 and has been previously described.
Arthroscopy is performed after general anesthesia is induced and after the knee is injected with 20 mL of 0.25% bupivacaine and epinephrine. Knee ROM and patellar mobility are evaluated once general anesthesia is achieved and are reassessed throughout the surgical procedure to determine if additional surgical steps are needed to remove mechanical blockages to knee extension and flexion.
To improve visibility of the anterior aspect of the knee joint, standard medial, and lateral portals are used, but the position of the portals is adjusted to be more proximal and slightly farther medial and lateral, respectively.
The first step is to examine the area anterior to the proximal tibia. If extrasynovial scar tissue has formed in this area, a blunt trocar is used to loosen the scar between the posterior aspect of the patellar tendon and the anterior aspect of the tibia. A basket forceps and meniscal shaver may be used to excise scar tissue in this area. One should ensure that the entire area from the anterior horns of the medial and lateral menisci down to the upper tibia is free of extrasynovial scar tissue. Patients with type 2, 3, or 4 arthrofibrosis often have scar formation in this area of the knee ( Fig. 108.8 ).

Second, the intercondylar notch is examined for signs of impingement, including the base of the ACL where a cyclops lesion may form (see Fig. 108.6 ). In patients with type 1 arthrofibrosis, this area is typically the only area of mechanical blockage causing ROM loss; this lesion is located inside the synovium and is not part of the fat pad ( Fig. 108.9 ). The knee must be placed through a ROM into full terminal extension to determine if the ACL fits into the intercondylar notch without any sign of impingement ( Fig. 108.10 ). Excision or ablation can be used to remove scar tissue that has formed in this area. If needed, a notchplasty may be performed to allow the ACL to fit within the intercondylar notch; thus the remaining knee extension that needs to be regained after surgery can be achieved with the passive knee extension device.

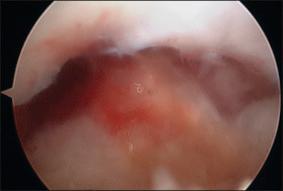
Fibrosis of the infrapatellar fat pad and/or the joint capsule is usually associated with type 3 or 4 arthrofibrosis. After using a blunt probe to establish a plane between the patellar tendon and the scar tissue, the scar tissue should be removed distally to the level of the upper tibia and anteriorly to the horns of the menisci. When the joint capsule is fibrotic, excision of the fibrotic capsule can be performed up to the insertion of the vastus medialis oblique and vastus lateralis muscles, which improves mobility of the patella and patellar tendon.
Patients with type 4 arthrofibrosis are not likely to regain full, symmetric knee flexion because of the shortening of the patellar tendon. However, in patients with type 3 or 4 arthrofibrosis, a manipulation is performed to maximize knee flexion. We do not recommend forceful manipulation for knee extension because most of the knee extension loss is due to either mechanical blocks that can be selectively removed and/or posterior capsular tightness that can be slowly stretched out during the course of postoperative rehabilitation.
The primary goals of postoperative treatment are to prevent a hemarthrosis and achieve/maintain full terminal extension symmetric to the opposite knee. Once the mechanical block to extension has been removed, immediate emphasis on full knee extension is needed to stretch the posterior capsule and allow the patient to regain full symmetric knee extension. To regain knee ROM, we have found that it is best to work only on knee extension first until symmetry is restored and then switch the focus of rehabilitation to knee flexion exercises during the next phase.
Patients remain in the hospital overnight as a 23-hour stay after surgery. Continuous intravenous administration of ketorolac is used for pain control and prevention of swelling. Antiembolism stockings and a cold/compression device (Cryo/Cuff, DJO Inc., Vista, CA) are used at all times starting immediately after surgery to prevent a hemarthrosis. The knee is placed in a continuous passive motion (CPM) machine set from 0 to 30 degrees, but the primary purpose of the CPM is to elevate the knee above the level of the heart ( Fig. 108.11 ).

Knee extension exercises are performed three to four times per day to ensure that full terminal knee extension is maintained. When the knee is in full terminal extension, the intercondylar notch is completely filled by the ACL and PCL, which prevents formation of fibrotic tissue near this notch. Knee extension exercises consist of using either the passive knee stretch device (see Fig. 108.4 ) or the passive knee extension device (see Fig. 108.7 ), towel stretch ( Fig. 108.12 ), active heel lift ( Fig. 108.13 ), heel prop stretch, and straight-leg raises. The active heel lift and straight-leg raise exercises are used to improve quadriceps muscle control and active terminal knee extension, which is important for long-term maintenance of full, symmetric knee extension.


Patients are discharged home but continue to follow the previously outlined protocol for the first 5 postoperative days. Patients are instructed to remain lying down with the knee elevated in the CPM machine and to use the cold/compression device at all times except when ambulating to and from the bathroom. This component of the protocol is vital to prevent the development of a hemarthrosis. Prevention of a hemarthrosis allows good quadriceps muscle control, which helps regain/maintain full knee extension and consequently allows for knee flexion deficits to be addressed sooner.
After the first postoperative week, patients continue to focus on the same rehabilitation goals but may gradually begin to return to normal daily activities. They are encouraged to use the cold/compression device at least three times a day for 30 minutes or more frequently if necessary to control swelling. During this phase of rehabilitation, it is important to educate patients about habits they need to work on to use the involved knee normally throughout the day and encourage full knee extension during daily activities. We call these extension habits . For the sitting extension habit, patients are advised to sit with the knee fully extended and the heel propped up on their other foot, allowing the knee to fall into full extension. The standing extension habit involves having the patient shift his or her weight onto the involved lower extremity, locking the knee out straight. This exercise encourages full knee extension and normal use of the involved lower extremity during activities of daily living. In addition, it maintains the newly achieved posterior capsular stretch and full contact of the femur, tibia, and ACL in terminal extension.
The speed at which each patient is ready to progress to the next phase of rehabilitation varies considerably based on the chronicity and extent of knee motion loss present. Once full, symmetric knee extension is regained and the patient can easily perform an active heel lift, knee flexion exercises are begun. In cases of more severe knee flexion loss, we begin with a wall slide exercise ( Fig. 108.14 ). Heel-slide exercises are the primary exercise used to improve knee flexion, with a 5-second hold and 10 to 15 repetitions performed per exercise session. Full knee flexion is achieved when the patient can sit on his or her heels without tilting the pelvis laterally (see Fig. 108.2 ). Patients must be instructed regarding ways to monitor knee extension closely, and knee flexion exercises should be put on hold if any loss of knee extension occurs.

Low-impact exercise using a bike or elliptical machine may be slowly introduced at this point. We recommend starting without any resistance and gradually increasing the time of the workout by 2 to 3 minutes according to the ability of the patient. ROM must be closely monitored and low-impact exercise should be stopped if the patient begins to lose motion.
Once full, symmetric knee flexion and extension are achieved and maintained, the rehabilitation focus shifts to a unilateral strengthening program to restore strength symmetry. We have found that trying to work on strength in the knee before full extension and flexion have been achieved is difficult because strengthening exercises frequently cause swelling and loss of ROM when they are performed on a stiff knee, thus defeating the purpose of the early phases of rehabilitation.
Loss of knee motion is often associated with significant strength deficits as a result of disuse. We recommend performing isokinetic testing of the quadriceps muscle group to quantify the amount of strength loss compared with the noninvolved knee. We consider strength to be symmetric when it is within 10% of the opposite, normal knee. We recommend using a high number of repetitions and low resistance for single leg press, single knee extension, and step-down exercises to achieve this goal. As with the other phases of the rehabilitation program, care must be taken to ensure that ROM loss does not occur once strengthening exercises commence. If the patient begins to lose knee motion, one should back off from the strengthening exercises until full ROM is restored and then slowly introduce strengthening exercises again.
Patients who are treated nonoperatively for knee ROM loss follow the same rehabilitation program and progression except for the surgery-specific measures such as the use of a CPM, antiembolism stockings, and a period of relative bed rest. We are finding that in a large number of patients who come to us for a second opinion, their knee ROM loss was overlooked and not treated by the previous physician and/or therapist. By carefully examining both knees and using the previously outlined treatment principles, many cases of anterior knee pain or generalized knee pain can be addressed effectively without surgery.
Participation in impact activities, such as running and jumping, is not encouraged until full ROM and strength symmetry are restored. Once these goals are reached, impact activities may be gradually introduced on an every-other-day basis. We recommend using a functional sports progression in which speed and change of direction are gradually increased based on the patient's tolerance. After the patient is comfortable performing individual speed and agility drills, individual sport-specific drills are introduced, followed by drills against a defender, and finally scrimmage and game situations are permitted. Close monitoring of knee extension and knee flexion must be performed on a daily basis to detect any loss of motion early and adjust activity levels accordingly. Patients should be instructed to monitor their own ROM by assessing end feel of the towel stretch exercise and sitting on their heels.
Because arthrofibrosis is a difficult complication to treat, prevention of this problem is the best treatment. The lead author coauthored a published series of 33 patients treated with the previously outlined protocol for arthrofibrosis. The study group included 19 women and 14 men, with a mean age of 31 years. All of these patients were seen in our center after arthrofibrosis developed following knee surgery performed elsewhere, and 27 of these patients experienced arthrofibrosis after an ACL reconstruction. The mean preoperative ROM was 0-8-117 degrees (hyperextension-extension-flexion) for the involved knee compared with 5-0-147 degrees for the uninvolved knee. At a mean of 8.6 months after surgery, the mean involved knee ROM improved to 3-0-134 degrees. The mean subjective scores on the International Knee Documentation Committee (IKDC) survey improved from 45.3 to 67.1 ( P < .01), and the patients who achieved normal ROM according to IKDC criteria (knee extension within 2 degrees and knee flexion within 5 degrees of the opposite knee) also had the highest subjective scores. Although these patients showed significant improvement after treatment, the results were still not nearly as good as they could have been if this ROM problem had been prevented and arthrofibrosis had not developed.
Another study looked at patients who did not have arthrofibrosis but were diagnosed with a deconditioned knee, including at least 5 degrees of extension loss compared with the opposite knee. This group included 25 men and 25 women with a mean age of 53.2 years. Osteoarthritis was the underlying pathology in 41 of the 50 patients, and 7 had undergone previous arthroscopy without rehabilitation. All patients were treated nonoperatively with the previously described rehabilitation program. After 3 months of rehabilitation and a guided home exercise program, the mean side-to-side deficit in knee extension improved from 10 to 3 degrees ( P < .01), and the mean side-to-side deficit in knee flexion improved from 19 to 9 degrees. Correspondingly, the IKDC subjective scores increased as ROM improved, with a mean at initial evaluation of 34.5 points, improving to 70.5 points 12 months later. This study shows that severe loss of ROM in nonoperative patients can be improved greatly with rehabilitation; correspondingly, subjective scores and function also improve. Without carefully examining each patient with knee pain, slight ROM loss that is contributing to the patient's knee symptoms can be overlooked, and unnecessary knee surgery may be performed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here