Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tumescent local anesthesia using lidocaine and epinephrine allows the removal of large volumes of fat with minimal blood loss and low postoperative morbidity.
A preconsultation questionnaire standardizes the medical history and focuses the consultation on issues that are crucial to the success of the liposuction.
Most bleeding disorders and any medications that prolong bleeding time are a contraindication to liposuction.
Liposuction is not a treatment for obesity, but can create a more aesthetic figure at an individual's current weight.
Continuous blood pressure monitoring, cardiac monitoring with pulse oximetry, and the availability of supplemental oxygen should be in place for procedures removing more than 100 mL of aspirate.
Following liposuction, around 12% of patients undergo a touch-up procedure. If a patient gains weight, the liposuctioned area will resist weight gain, which may cause fat to accumulate in a new area.
Liposuction with local anesthesia had its inception in 1987 with Klein's seminal publication on tumescent technique. Before this, adipose deposits had been removed by en bloc resection in combination with skin excision or were scraped out through small incisions. Two Italian cosmetic surgeons, Drs Arpad and Georgio Fischer, introduced the suction technique for removal of fat. The Fischers also introduced the use of a blunt cannula and criss-cross tunneling. Fournier, a French general surgeon, promoted syringe rather than machine liposuction and is considered one of the main pioneers in the field. Illouz, a gynecologist, is credited with popularizing liposuction by using the Fischers' technique with the Karman cannula – a widely available, reasonably priced, soft, flexible cannula that was developed for abortion procedures. Illouz is also responsible for the original “wet technique” in which a hypotonic saline solution with hyaluronidase was injected into the fat. Wet technique liposuction was popularized in Europe; however, prior to Klein's introduction of tumescent anesthesia, the predominant form of liposuction practiced in the USA was the “dry technique.” Patients were put under general anesthesia and minimal local anesthesia was used, so significant blood loss was a common complication with the dry method. A number of American dermatologists including Asken, and Stegman and Tromovitch began utilizing local anesthesia for liposuction in the early and mid-1980s. Liposuction with local anesthesia allows removal of large volumes of fat with minimal blood loss, less postoperative morbidity, excellent cosmesis, and a remarkable safety profile. There have been no fatalities from liposuction by dermatologists who follow the American Academy of Dermatology's Guidelines of care for liposuction .
Klein's tumescent technique was adopted by dermatologists in Europe in the early 1990s. The term “tumescent local anesthesia” was first used in the title of a German text on liposuction, published in 1999. The book was published in English in 2001. Additional books on the subject have been published by American dermatologists.
The consultation starts when the receptionist books the appointment. It is important that whoever answers the phone is knowledgeable about the procedure so they can obtain some initial information to determine if the person calling is a candidate for liposuction. If their health or physical characteristics or their expectations clearly make them a poor candidate, it is best to find out before they come in for a consultation. If the receptionist is too busy to spend time with a potential liposuction candidate, the call may be transferred to the cosmetic consultant. The time spent on the phone is rewarded with the patient being prepared for the office consultation. It is not unusual for patients to tell us that they booked their consultation because our office gave them more information than other offices they called.
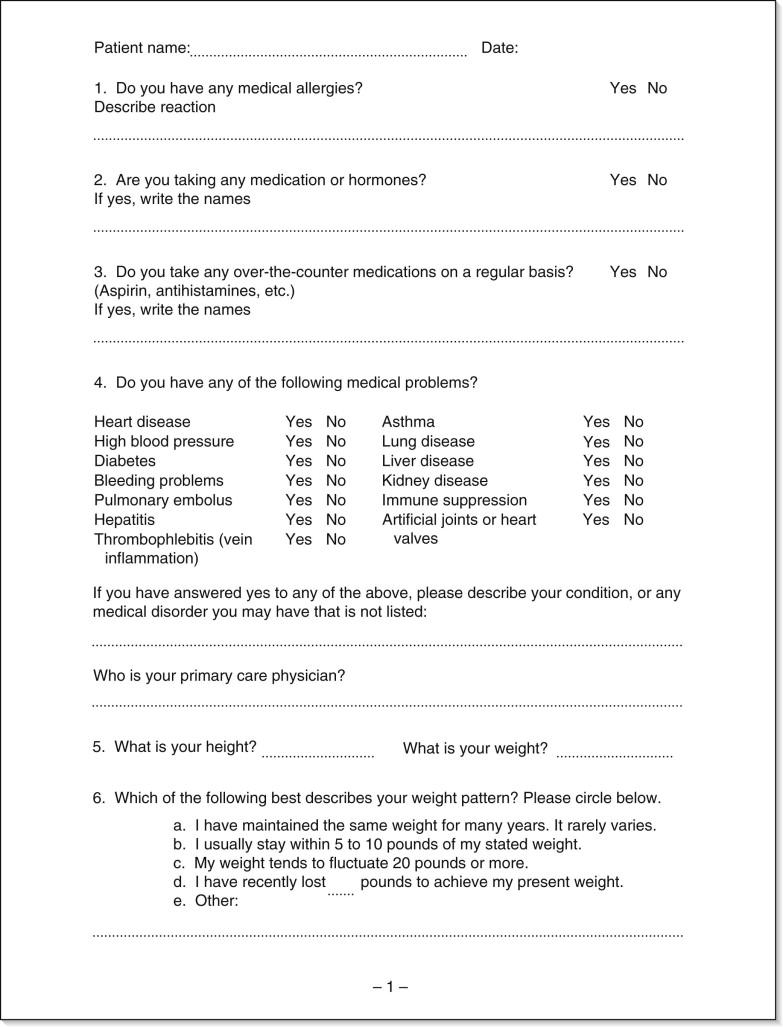
A thorough consultation takes 30–60 min. We use a preconsultation questionnaire to standardize the intake of medical history and focus the consultation on the issues that are crucial to successful liposuction ( Fig. 28.1 ).
Liposuction is an elective cosmetic procedure best done on healthy patients. Patients should be carefully screened for any medical conditions that would put them at increased risk of surgical complications. Most physicians feel that cosmetic procedures should be limited to patients who fall into the American Society of Anesthesiologists' Physical Status Classification System classes I or II (rarely class III) ( Table 28.1 ). It is important to have a low threshold to request medical clearance, as patients sometimes downplay the severity of their medical conditions because they desire the procedure. We routinely request medical clearance for all patients over 60 years old, or for those with a history of cardiovascular disease, hypertension, or diabetes. Lidocaine is metabolized by the liver, so patients with impaired liver function from hepatitis C, hepatitis B, alcoholic liver disease, previous treatment with chemotherapy or antiretroviral therapy, or other liver disease may be at increased risk for lidocaine toxicity. Immunosuppressed patients, whether due to medications or disease, are at increased risk of infection. In these patients, one must consider the risk : benefit ratio of the procedure and confer with the specialist monitoring their care.
| ASA Physical Status I | A normal healthy patient |
| ASA Physical Status II | A patient with mild systemic disease |
| ASA Physical Status III | A patient with severe systemic disease |
| ASA Physical Status IV | A patient with severe systemic disease that is a constant threat to life |
| ASA Physical Status V | A moribund patient who is not expected to survive without the operation |
| ASA Physical Status VI | A declared brain-dead patient whose organs are being removed for donor purposes |
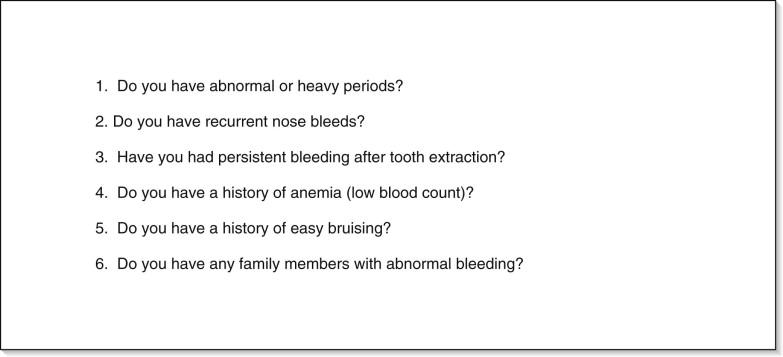
Patients are also screened for increased risk of thromboembolism as evidenced by a prior history of thrombophlebitis, deep venous thrombosis, pulmonary embolism, protein C or protein S deficiency, high-dose estrogen therapy, tobacco use, or other coagulopathy. Likewise, bleeding diatheses should also be inquired about due to the increased risk of postoperative hematoma. Most bleeding disorders are a contraindication to liposuction. We highlight five questions by putting them on a separate page of the questionnaire to identify patients with potential bleeding abnormalities ( Fig. 28.2 ). It is essential to obtain a thorough medical history as standard laboratory studies will not uncover all bleeding disorders (such as von Willebrand's disease).
Preoperative screening studies are performed on all patients including a complete blood count with platelet count, chemistry profile with liver function tests, and prothrombin/partial thromboplastin time. In addition, the surgeon may wish to order screening studies for HIV and hepatitis B and C based on local standards of care. On the day of the procedure, we also perform a urine pregnancy test on all premenopausal women.
The patient's history of abdominal surgeries is important if they are being evaluated for abdominal liposuction. Special attention should be paid to any surgery complicated by dehiscence, hernia, infection, or subsequent adhesions that might leave an incomplete rectus abdominus muscle layer over the peritoneum. Careful examination of surgical scars should be performed to evaluate for the presence of underlying hernias and fibrous adhesions. If the history or exam is suspicious for hernias, adhesions or scars, one should obtain medical records, reports, or radiologic studies, or discuss the matter with the patient's surgeon. It is important to document the age of any scars, as older scars are soft and pliable and can be suctioned through, but newer scars should be suctioned around. Any history of keloids or hypertrophic scars should be discussed thoroughly with the patient as multiple incisions are necessary for cannula insertion.
The medication history must be complete. The patient should be queried about hormone replacement, herbal supplements, and over-the-counter medications, as well as prescription drugs. High-dose estrogen can put a woman in a higher risk category for thromboembolism, particularly if she is a smoker, or is within the first year of therapy with high-dose estrogen. Butterwick concluded that the current standard of care is to allow patients to remain on low-dose oral contraceptives as the risk of thrombosis from these agents is extremely low.
Any medications that prolong bleeding time are contraindicated in liposuction. These include prescription medications such as warfarin or clopidogrel bisulfate, and over-the-counter medications such as aspirin and non-steroidal anti-inflammatory drugs (NSAIDs). The antiplatelet effects of aspirin are irreversible and last 10–14 days and 7–10 days for NSAIDs. Patients should be instructed to check all over-the-counter medications with the physician's office at least 2 weeks prior to surgery as many have “hidden” aspirin or NSAID ingredients. Patients are given a full list of herbal supplements that can affect coagulation, and they are instructed to refrain from taking them for 2 weeks before surgery ( Table 28.2 ). If the patient takes one of these medications, the liposuction is postponed.
| Herbal compound | Effect | Constituent(s) |
|---|---|---|
| Anticoagulants | ||
| Alfalfa | Anticoagulant, coagulant | Coumarin, vitamin K |
| Angelica | Anticoagulant, antiplatelet | Coumarin |
| Anise (excessive doses) | Anticoagulant | Coumarin |
| Arnica | Anticoagulant | Coumarin |
| Asafoetida | Anticoagulant | Coumarin |
| Aspen | Antiplatelet | – |
| Bilberry | Antiplatelet | – |
| Black cohosh | Antiplatelet | Salicylate |
| Blackcurrant | Antiplatelet | Linolenic acid |
| Bladderwrack | Antiplatelet | – |
| Bogbean | Bleeding risk | Unknown |
| Boldo | Anticoagulant | Coumarin |
| Borage seed oil | Anticoagulant | Enzyme |
| Bromelain | Anticoagulant | Enzyme |
| Capsicum | Antiplatelet | Capsaicinoid |
| Cayenne fruit | Antiplatelet | – |
| Celery | Antiplatelet | Apigenin (coumarin) |
| Clove | Antiplatelet | Eugenol |
| Danshen | Anticoagulant | Protocatechuic aldehyde 3,4-dihydroxyphenyl-lactic acid |
| Da huang | Antiplatelet | – |
| Devil's claw | Antiplatelet | Coumarin |
| Dong Quai | Anticoagulant, antiplatelet | Coumarin |
| Evening primrose seed oil | Antiplatelet | – |
| Fenugreek | Anticoagulant | Coumarin |
| Feverfew | Antiplatelet (crude extract) | – |
| Fish oil (omega-3) | Antiplatelet, prostacyclin synthesis, vasodilatation, reduced platelets and adhesiveness, prolonged bleeding time | – |
| Fucus | Anticoagulant, increased risk of bleeding | – |
| Garlic (excessive doses) | Inhibition of platelet aggregation, increased risk of bleeding | – |
| German chamomile | Antiplatelet | Coumarin |
| Ginger | Anticoagulant, increased risk of bleeding | – |
| Ginkgo | Inhibition of platelet aggregation, decrease in blood viscosity | – |
| Ginseng | Anticoagulant, antiplatelet | – |
| Horse chestnut | Anticoagulant | Aesculin (coumarin) |
| Horseradish | Anticoagulant | Coumarin |
| Kava kava root | Antiplatelet | – |
| Licorice | Antiplatelet | Coumarin |
| Meadowsweet | Anticoagulant | Salicylate |
| Northern prickly ash | Anticoagulant | Coumarin |
| Onion | Antiplatelet | Unknown |
| Papain | Bleeding risk | Unknown |
| Papaya | Antiplatelet | – |
| Passionflower | Anticoagulant | Coumarin |
| Pau D'Arco | Anticoagulant | Lapachol |
| Poplar | Antiplatelet | Salicin |
| Quassia | Anticoagulant | Coumarin |
| Red clover | Anticoagulant | Coumarin |
| Roman chamomile | Anticoagulant | Coumarin |
| Safflower | Anticoagulant | Safflower yellow |
| Southern prickly ash | Anticoagulant | Coumarin |
| Sweet clover | Anticoagulant | Dicumarol |
| Sweet vernal grass | Anticoagulant | Coumarin |
| Tamarind | Increased bioavailability of aspirin and ibuprofen | |
| Tonka bean | Anticoagulant | Coumarin |
| Turmeric | Antiplatelet | Curcumin |
| Vitamin E | Inhibition of platelet aggregation and adhesion, interference with vitamin K-dependent clotting factor (large doses) | |
| Wild carrot | Anticoagulant | Coumarin |
| Wild lettuce | Anticoagulant | Coumarin |
| Willow bark | Antiplatelet | Salicylate |
| Procoagulants | ||
| Agrimony | Coagulant | Vitamin K |
| Alfalfa | Anticoagulant, coagulant | Coumarin, vitamin K |
| European mistletoe | Coagulant | Coumarin |
| Goldenseal | Coagulant | Berberine |
| Green tea | Coagulant | Vitamin K |
| Plantain | Coagulant | Vitamin K |
| Stinging nettle | Coagulant | Vitamin K |
| Yarrow | Coagulant | Achilleine |
Lidocaine is metabolized by the liver enzyme cytochrome P450 (CYP450). There are a number of drugs which induce this enzyme system or act as competitive inhibitors ( Table 28.3 ). Competitive inhibition slows the metabolism of lidocaine, causing an increase in blood levels, thereby potentiating its toxicity. When a patient is taking one of these medications, the physician can either request that they discontinue the medication, or decrease the maximum dose of lidocaine used; however, there are no clear guidelines documenting how this should be done. In our practice, we typically decrease the maximum dose of lidocaine to 35 mg/kg in patients on these medications. Alternatively, we will perform the liposuction in two or more sessions. It is also important to note the half-life of any medications that interact with lidocaine. For example, the antidepressant fluoxetine (Prozac; Eli Lilly, Indianapolis, IN) has metabolites that last approximately 2 months after administration has ceased. Lidocaine can safely be given at 55 mg/kg in a patient on no such medications.
| Precipitant drug group | Examples and comments |
|---|---|
| These drugs ↑ lidocaine serum levels (and potential toxicity) – CYP3A4 inhibition b | |
| Antiarrhythmic agents | Amiodarone (an inhibitor), disopyramide, quinidine (competing substrates) |
| Antibacterial – macrolides/related | Clarithromycin, erythromycin |
| Antibacterial – other categories | Quinupristin/dalfopristin |
| Antidepressants – other | Nefazodone |
| Antidepressants – selective serotonin reuptake inhibitors | Fluoxetine (weak CYP3A4 inhibition), fluvoxamine (also CYP1A2 inhibitor) |
| Antifungal agents – azoles/triazoles | Ketoconazole > itraconazole > fluconazole |
| Calcium channel blockers | Diltiazem and verapamil (strong CYP3A4 inhibition), nicardipine (weaker) |
| Foods and nutrients | Grapefruit, grapefruit juice |
| HIV drugs – protease inhibitors | Ritonavir, indinavir > saquinavir, nelfinavir, others |
| Hormone antagonists | Danazol |
| Sedatives – benzodiazepines | Alprazolam, midazolam, triazolam (all competing substrates only) |
| These drugs ↓ levels of lidocaine due to CYP3A4 and 1A2 induction (loss of efficacy) | |
| Antibacterial – rifamycins | Rifabutin (CYP3A4); rifampin (CYP3A4 and IA2), rifapentine (CYP3A4) |
| Anticonvulsants | Carbamazepine, phenobarbital, phenytoin (phenytoin induces CYP3A4 only) |
| HIV drugs | Nevirapine (CYP3A4 inducer only) |
| These drugs ↑ lidocaine serum levels (and potential toxicity) – CYP1A2 inhibition | |
| Antiarrhythmic agents | Mexiletine |
| Antibacterial – fluoroquinolones | Ciprofloxacin, enoxacin, norfloxacin, etc. |
| H 2 antihistamines | Cimetidine |
| HIV drugs – protease inhibitors | Atazanavir |
| Leukotriene inhibitors | Zileuton |
| Miscellaneous drugs | Tacrine |
| Other interactions of importance involving lidocaine (and related amides) | |
| Antiarrhythmic agents b | Procainamide, tocainide; possibly additive cardiodepressant activity |
| β-Blockers b | Propranolol, sotalol; lidocaine levels, risk of arrhythmias |
| Neuromuscular blockers | Succinylcholine; prolongation of neuromuscular blockade |
a Lidocaine (and related amides) are predominantly CYP3A4 substrates, but are also CYP1A2 substrates to a lesser degree.
b Conceptually relatively high-risk drug interactions, although at conservative doses well below the maximum dose listed in this chapter, the risk is fairly low; with higher doses, be very cautious in patients concomitantly receiving these drugs.
It is important to elicit any history of medication allergies, as well as usage of medications that could potentially interact with the drugs administered during the procedure. The two major drugs in the tumescent fluid are lidocaine and epinephrine. Allergy to lidocaine is extremely rare and is a contraindication to the procedure. Most patients who claim an allergy to lidocaine are actually allergic to methylparaben, the preservative in the anesthetic. If the patient claims to be allergic to lidocaine, we refer to an allergist for provocative testing. If the allergy is only to the preservative, we use preservative-free lidocaine. People who are allergic to ester anesthetics should also have preservative-free lidocaine, because the ester metabolite, p -aminobenzoic acid (PABA), is the allergen which cross-reacts with the metabolite of methylparaben. Epinephrine, which is added to the fluid as a vasoconstrictor to decrease bleeding, is an endogenous catecholamine to which allergy is not possible. Some patients are more sensitive to its effects, particularly when it is administered in a highly vascular area such as the oral mucosa during dental work. These patients may describe episodes of palpitations in the past. However, even in this group it is rare for a patient to experience such symptoms following tumescent anesthesia because adipose is relatively less vascular than the oral mucosa. When seen, tachycardia due to the epinephrine in the tumescent infiltration is probably due to a hypersensitive conduction system in the patient. This is extremely rare for us now that we have decreased the epinephrine dose to 0.65 mg per liter bag of tumescent fluid. Some surgeons will also give clonidine 0.1 mg to every patient with a blood pressure of ≥100/70 mmHg.
Allergy to latex is also important to note so the surgeon and assistants are sure to wear latex-free gloves and use latex-free dressings. Most medical tubing is now latex free and does not pose a problem.
Although reactivation of varicella zoster virus following liposuction has been reported, we do not advocate pretreatment with antivirals.
There are several areas of concern when evaluating a patient's dieting and weight history. Weight cycling – repeated weight loss and weight gain – is a common pattern for many people who struggle with their weight. When looking at predictors of weight loss maintenance, those who diet frequently show significantly more weight regain than those who diet less frequently. Although patients who combine diet and exercise lose more weight than those who either diet or exercise, those who lose weight through exercise maintain their weight loss best.
If the potential liposuction candidate has recently lost significant weight and liposuction is done at this point in their weight cycle, subsequent weight regain can have a negative impact on the result. The type of diet of the liposuction candidate is also important information. Diets with a behavioral modification component have a higher degree of success. Diets that are very low in calories and fat have a low rate of success in maintenance as they can cause the metabolism to slow down to conserve energy, and the body enters a starvation mode. When the dieter returns to eating normally, regain of weight can be very quick.
Although conventional wisdom has been that the best candidates for liposuction are those patients at or near their ideal weight, patients with body mass indices (BMIs) in the obese range ( Table 28.4 ) frequently undergo this procedure. These patients can be good candidates if they are truly looking for reshaping and not weight loss. It is well documented that obesity is a risk factor for cardiovascular disease and type II diabetes mellitus. It has been hypothesized that removal of subcutaneous fat with liposuction may decrease a patient's risk of these conditions by decreasing their overall adiposity. Several groups have demonstrated short-term improvements in insulin resistance, inflammatory markers associated with cardiovascular risk, and glucose levels in patients undergoing large-volume liposuction. Others have reported no improvement in these parameters. Although follow-up in all of these studies did not exceed 6 months, in the early postoperative period, liposuction does not appear to be detrimental to the patient's metabolic health, and they may even experience some health benefits.
| BMI | Weight status |
|---|---|
| Below 18.5 | Underweight |
| 18.5–24.9 | Normal |
| 25.0–29.9 | Overweight |
| 30.0 and above | Obese |
The exercise history is important as it affects basal metabolic rate, maintenance of weight loss, and overall health of the patient. Additionally, muscle tone impacts the body contour in a number of areas where liposuction is commonly performed. A good physical exam enables the physician to identify which areas could be improved by increasing muscle tone. For example, a woman's dissatisfaction with her upper arm contour can be the result of excess adipose, skin laxity, and poor muscle tone. Some women have good muscle tone in the upper arms, but are looking for individual muscle definition, as is common in men. Because even the thinnest women have a higher body fat percentage than men, this look is usually only attainable if women bring their body fat percentage to an extremely low level. This can also give them a cachectic appearance in the face, upper chest, and neck.
The buttocks and abdomen are other areas where improved muscle tone positively impacts overall contour, because muscle tone and extramuscular fat are the primary predictors of buttock contour. In contrast, abdominal fullness may also involve intra-abdominal fat, rectus abdominus diastasis (usually in multiparous women), and ventral hernias.
During the consultation, the patient's goals are explored to ensure that they are congruent with what liposuction can accomplish ( Fig. 28.1 ). An elegant study by Ozgur and colleagues looked at three groups: patients seeking aesthetic surgery (AG), patients seeking reconstructive surgery (RG), and a control group (CG) of non-surgery seekers from the normal population. Each group consisted of 100 people, and all 300 were asked to complete a sociodemographic questionnaire, the life-satisfaction index (LSI), a self-esteem inventory (SEI), and a body-image inventory (BII). The LSI and BII were not significantly different between the three groups. The SEI was significantly better in the AG than the RG. This confirms what is seen in practice – that patients seeking cosmetic procedures generally do not have low satisfaction with their life or distorted body images. Another survey of patients who had undergone liposuction during a 5-year period revealed that the majority of patients (80%) were satisfied with their results. Based on this survey, patients who coupled body contouring with eating a healthy diet and exercising regularly had higher long-term satisfaction than patients who did not.
Ten years ago, the ideal candidate was described as a person at their ideal body weight but with disproportionate adiposity causing a contour deformity. Most liposuction surgeons now have a broader definition of “ideal” because we have seen overweight patients (not morbidly obese) with disproportionate adipose distribution who benefit from liposuction. Liposuction is not a weight-loss procedure or substitute for bariatric surgery. Good candidates are not seeking to lose weight, but to create a more aesthetic figure at their current weight. Often, this group of patients is so inspired by the results of liposuction that they go on to lose weight through diet and exercise.
During the consultation it is very important to set patient expectations of the results of liposuction. In all body areas, this result is limited by the pre-existing bony structure, skin quality and texture, the tone and build of muscle, and adipose in the area that is not amenable to liposuction. It is important that patients understand the components that will not be corrected by liposuction alone. Patients are usually very accepting of the imperfections remaining after liposuction if they are counseled about them in advance of the procedure.
Body dysmorphic disorder (BDD) has become an increasingly recognized condition among dermatology and cosmetic surgery patients, affecting up to 7–15% of patients in these practices. A diagnosis of BDD is based on the following three criteria from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders , 4th ed. (DSM-IV) ( Table 28.5 ). If a surgeon suspects BDD, it is prudent not to perform liposuction even if the patient is a good candidate physiologically. Even if they experience an excellent result from liposuction, they will likely shift their focus on imperfection to another body site. It is important when these patients are identified to refer them to a psychiatrist for treatment.
| 1 | Repetitive behaviors or mental acts in response to preoccupation with an imagined defect in appearance. If a slight physical anomaly is present, the person's concern is markedly excessive. |
| 2 | The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| 3 | The preoccupation is not better accounted for by another mental disorder (e.g., dissatisfaction with body shape and size in anorexia nervosa). |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here