Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Guidelines recommend echocardiography as the imaging modality of choice in the diagnosis and management guidance in patients with suspected infective endocarditis (IE). , Although echocardiographic findings lead to definitive diagnosis in the majority of patients, atypical results or results of uncertain clinical significance are not rare. The diagnostic yield and limitations of transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) depend on several factors, including (1) image quality, (2) the specific pathology associated with endocarditis (i.e., vegetations, valvular dysfunction or perivalvular extension), (3) the presence of prosthetic valve or device involvement, and (4) the index of clinical suspicion in the patient being investigated.
Early studies demonstrated that M-mode echocardiography was able to detect approximately one-third of native valve vegetations. With the advent of real-time two-dimensional and more recently three-dimensional (3D) echocardiography along with color and spectral Doppler capabilities, echocardiography is now well established as the gold standard for imaging diagnosis of IE and is incorporated into the modified Duke criteria as a major criterion. Echocardiography is capable of detecting the three major findings involving endocarditis: vegetations, valvular dysfunction and perivalvular extension, with varying accuracy, depending on both patient and imaging factors.
The clinical index of suspicion of endocarditis in a particular patient influences the specificity of TTE and TEE. Clinical index of suspicion is assessed via the Duke criteria, incorporating major (microbiological and echocardiographic) and minor (clinical and microbiological) criteria to categorize presentations into definite, possible or rejected IE. , , Current Appropriate Use Criteria guidelines for echocardiography that incorporate clinical suspicion of disease are summarized in Table 116.1 . It is recommended that any patient suspected of having IE by appropriate clinical criteria (positive blood cultures or new murmur) should be screened with TTE. If the images are of good quality and the study result is negative in a patient with a low index of clinical suspicion, an alternative diagnosis should be sought. TEE should be performed when clinical suspicion is high (staphylococcal bacteremia, fungemia, prosthetic heart valve or intracardiac device). Additionally, a repeat TEE should be performed 7 to 10 days after the initial study in cases of persisting high index of clinical suspicion and even earlier when indicated by the clinical situation such as suspected postoperative staphylococcal prosthetic valve endocarditis. The importance of applying clinical criteria to determine investigation approach cannot be overstated. Greaves and colleagues demonstrated that the absence of five clinical characteristics (embolic phenomena, central venous access, intravenous drug use, prosthetic valve, and positive blood culture) virtually ruled out that a TTE would demonstrate evidence of endocarditis.
| Transthoracic Echocardiography | Appropriate | Score |
|---|---|---|
| Initial evaluation of suspected IE with positive blood cultures or new murmur | Yes | 9 |
| Transient fever without evidence of bacteremia or a new murmur | No | 2 |
| Transient bacteremia with a pathogen not typically associated with IE and/or a documented nonendovascular source of infection | No | 3 |
| Reevaluation of IE at high risk for progression or complication or with a change in clinical status or cardiac examination | Yes | 9 |
| Routine surveillance of uncomplicated IE when no change in management is contemplated | No | 2 |
| Transesophageal Echocardiography | Appropriate | Score |
|---|---|---|
| To diagnose IE with a low pretest probability (e.g., transient fever, known alternative source of infection, or negative blood cultures or atypical pathogen for IE) | No | 3 |
| To diagnose IE with moderate or high pretest probability (e.g., staphylococcal bacteremia, fungemia, prosthetic heart valve or intracardiac device) | Yes | 9 |
It is essential that the clinician is aware that both TTE and TEE are not 100% sensitive and specific. Depending on the patient population studied, the sensitivity of TTE for detection of native valvular vegetations has been reported to be between 21% and 87% ( Table 116.2 ). Echocardiographic diagnosis of IE on TTE is limited by generally accepted limitations of image quality, including patient body habitus, mechanical ventilation, presence of chest wall deformities, and interposing lung tissue. In contrast, TEE is not limited by the aforementioned issues. TEE’s superior image quality is the main reason it demonstrates greater diagnostic accuracy compared with TTE, with studies reporting sensitivity ranges between 86% and 100% , for native valvular vegetations ( Fig. 116.1 ).
| Study | Patients ( n ) | Valve | TTE | TEE | ||
|---|---|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |||
| Erbel et al (1988) | 96 | 63 | 98 | 100 | 98 | |
| Shively et al (1991) | 62 | 44 | 98 | 94 | 100 | |
| Pedersen et al (1991) | 24 | 50 | 100 | |||
| Birmingham et al (1992) | 61 | Aortic | 25 | 88 | ||
| Mitral | 50 | 100 | ||||
| Sochowski et al (1993) | 105 | 91 | ||||
| Shapiro et al (1994) | 64 | 60 | 91 | 87 | 91 | |
| De Castro et al (1997) | 57 | 80 | 95 | |||
| Reynolds et al (2003) | 50 | All | 55 | N/A (TEE as standard) | ||
| Aortic | 50 | |||||
| Mitral | 62 | |||||
| Jassal et al (2007) | 36 | 84 | 88 | N/A (TEE as standard) | ||
| Casella et al (2009) | 75 | All | 87 | 86 | N/A (TEE as standard) | |
| Aortic | 71 | |||||
| Mitral | 87 | |||||
| Kini et al (2010) | 511 | 45 | 79 | N/A (TEE as standard) | ||
| Sekar et al (2017) | 119 | 21 | 100 | 86 | 97 | |
| Range | 21–87 | 79–100 | 86–100 | 91–100 | ||
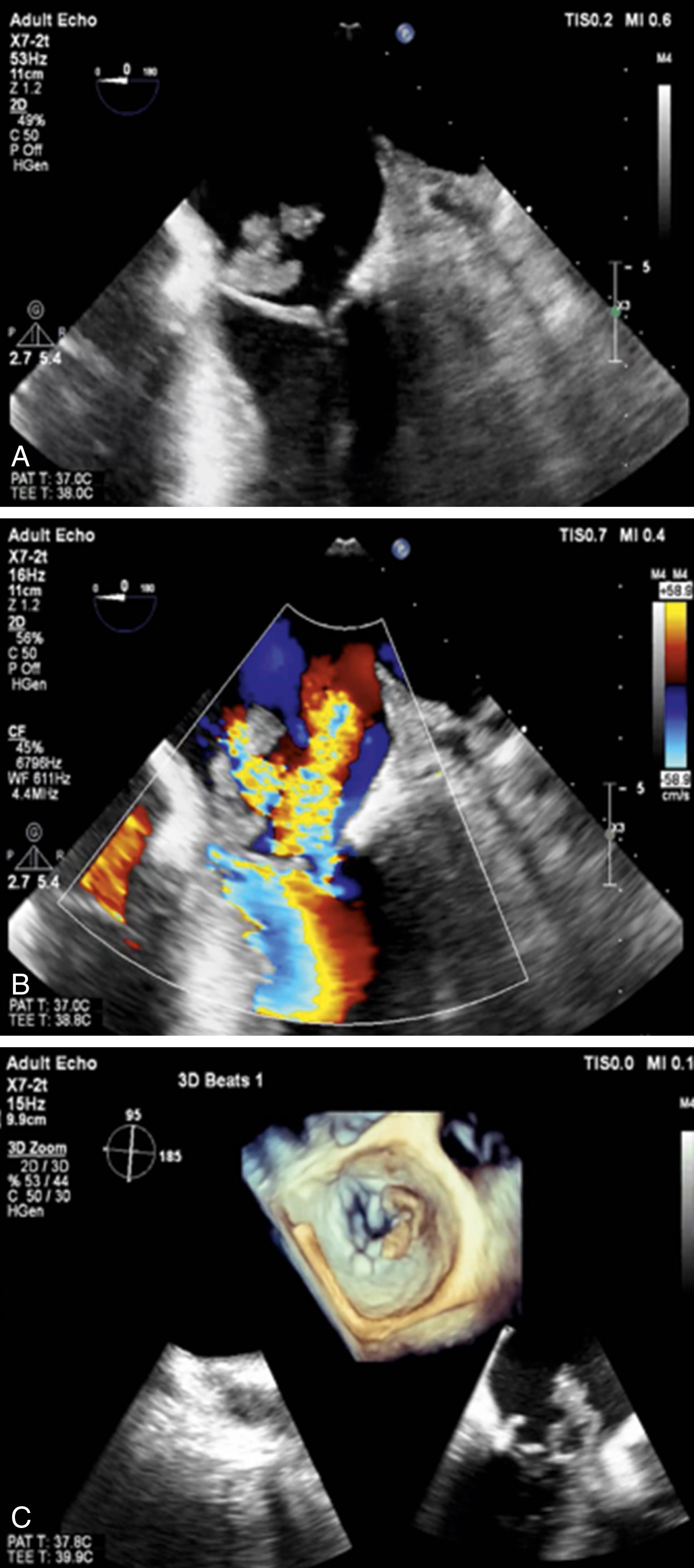
The use of harmonic imaging improves image quality of TTE compared with fundamental imaging, leading to improved sensitivity; however, it is suboptimal for the assessment of certain complications such as annular abscesses, which are superiorly defined with TEE, particularly in this era of high-frequency, multiplanar probes. The use of 3D echocardiography may further improve the detection of vegetations on transthoracic studies (see Fig. 116.1 ).
Near-field windows provided by TEE for left-sided aortic and semilunar valves ensure diagnostic superiority of TEE for the assessment of left-sided structures; however, comparatively, the anterior positioning of right-sided aortic and semilunar valves often lends itself to better visualization with TTE.
Echocardiographic studies are more likely to be falsely negative in the setting of small vegetations. The limits of image resolution allow for the detection of vegetations as small as 3 to 4 mm for TTE; however, only 25% of vegetations smaller than 5 mm and 70% between 6 and 10 mm are identified. Although the higher resolution of TEE detects smaller vegetations, Sochowski and colleagues reported that 5 of 65 (7.6%) patients with an initially negative TEE result were eventually diagnosed with IE on a repeat TEE study 1 to 2 weeks later. This reiterates the importance of repeating TEE at 7 to 10 days when clinical index of suspicion remains high because early on, vegetations may be too small to be detected. Atypically located or nonoscillating vegetations are also more likely to be missed because vegetations have a similar echogenicity to normal myocardium.
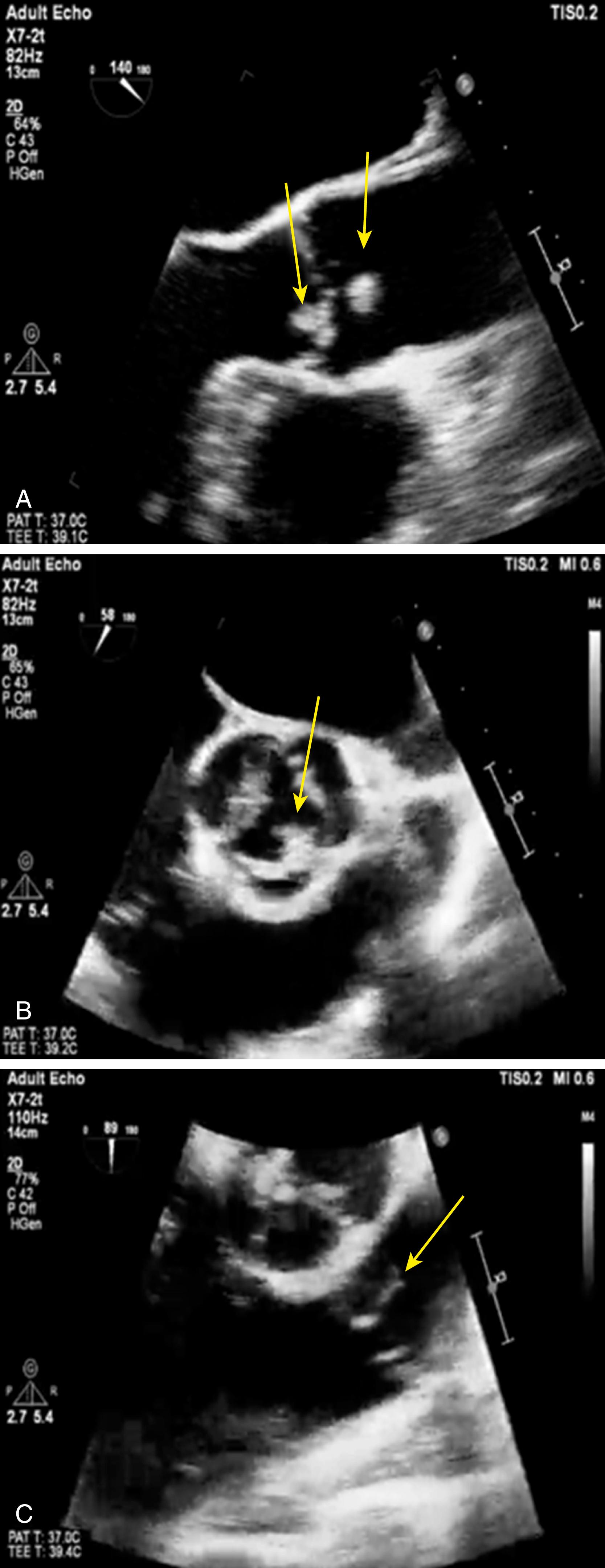
The presence of preexisting significant valvular lesions such as mitral valve prolapse or valvular degenerative disease makes identification of vegetations challenging and can lead to false-negative results ( Fig. 116.2 ). Acoustic shadowing from prosthetic material or valvular calcification, leading to incomplete visualization of the entire valve apparatus, affects the diagnostic accuracy of TTE.

False-positive echocardiographic results leading to an incorrect diagnosis of IE can also occur. Vegetations can be difficult to differentiate from thrombi, cusp prolapse, flail chords, cardiac tumors, myxomatous changes, Lambl excrescences, and prominent Eustachian valves (see Fig. 116.2 ). Thin linear strands can be seen commonly on native valves along the leaflet coaptation zone and may be misidentified as vegetation. Noninfective vegetations (marantic endocarditis) are impossible to differentiate from infective vegetations ( Fig. 116.3 ) but can be suspected in the setting of multiple small vegetations without associated valvular destruction or perivalvular abscess.
Owing to the possibility of both false-positive and false-negative echocardiographic study results, an individualized approach to each case is essential, incorporating echocardiographic data in combination with supportive clinical and microbiological evidence in making a definitive diagnosis of IE.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here