Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Masses of the upper extremity are among the most common reasons for referral to a hand surgeon, with ganglions alone representing the second most frequent cause of referral. The vast majority of these lesions are benign, however the average hand surgeon will encounter a few malignant sarcomas during their career. For this reason, when evaluating any mass of the upper extremity it is imperative that the surgeon maintains a high level of suspicion and performs a thorough history and examination. With a systematic approach and strict adherence to standard principles of management, surgeons can provide optimal care to patients.
A thorough history and physical examination can provide a careful clinician with an accurate diagnosis in many cases. Targeted questions regarding an upper extremity mass should include: the length of time the mass has been present, the presence and quality of pain, any change in size/symptoms, a history of trauma in the area, and any systemic symptoms. The patient’s age, history of weight loss, personal/family history of malignancy, tobacco use, exposure to radiation/other carcinogens, and medications should all be elicited.
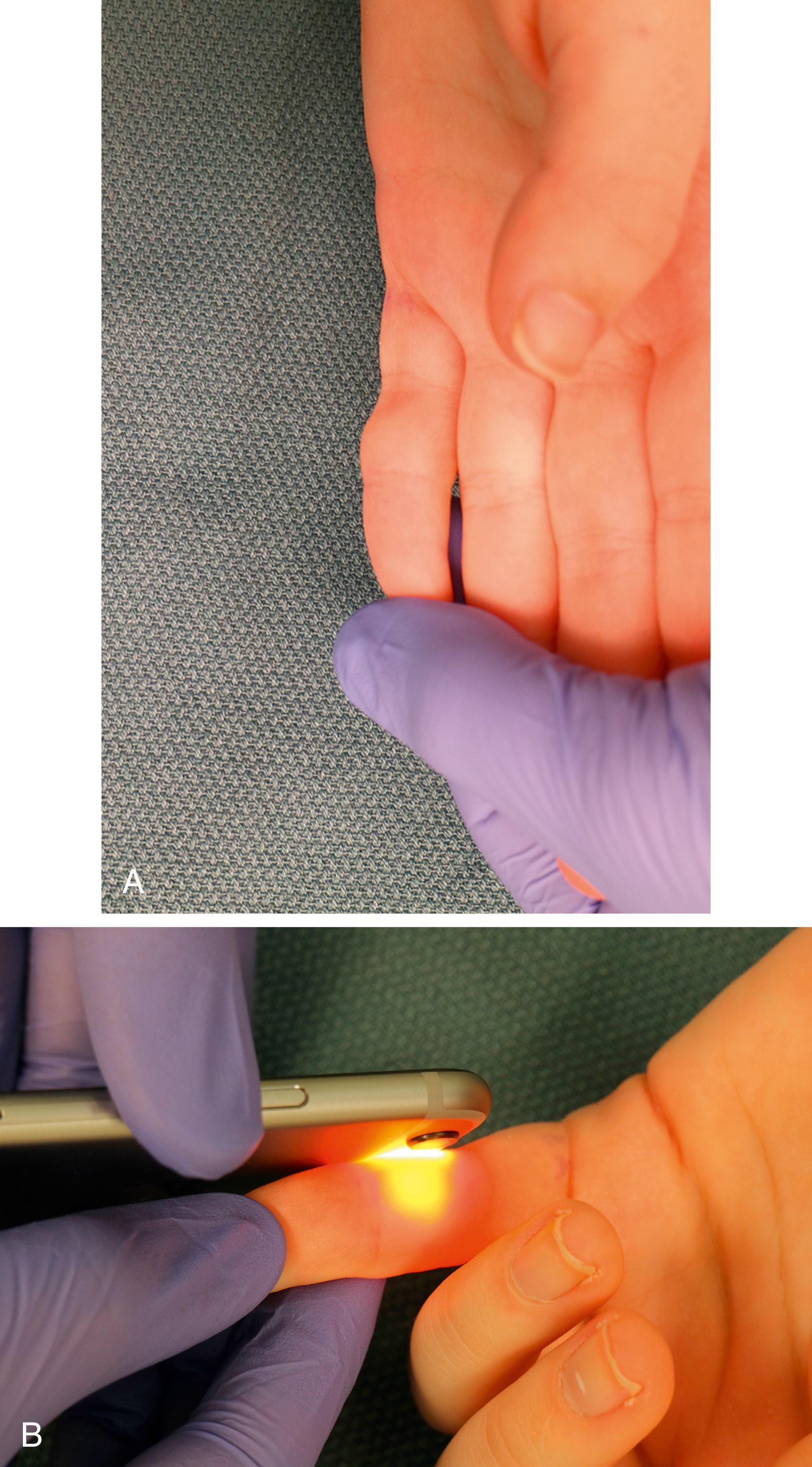
A thorough standard hand examination should be performed and documented in order to uncover any potential functional deficits due to mass involvement. This is especially important for medical-legal reasons prior to surgical intervention. When focusing on the lesion, the size, shape, color, consistency, and mobility of the lesion should be noted. Transillumination can be helpful in determining if a mass is cystic ( Fig. 60.1 ). The approximate depth of the mass relative to other tissues in the area can also frequently be assessed through palpation. Additionally, manipulating the mass in both transverse and proximal to distal directions can elucidate any adherence to the overlying skin or deeper structures (tendon, bone). Lastly, the function of adjacent structures should be carefully assessed; a Tinel’s sign in nearby nerves should be noted if present, and nearby joints should be a assessed for their range of motion. Any patient with a lesion determined to be high risk for malignancy requires a thorough pulmonary and lymphatic examination.
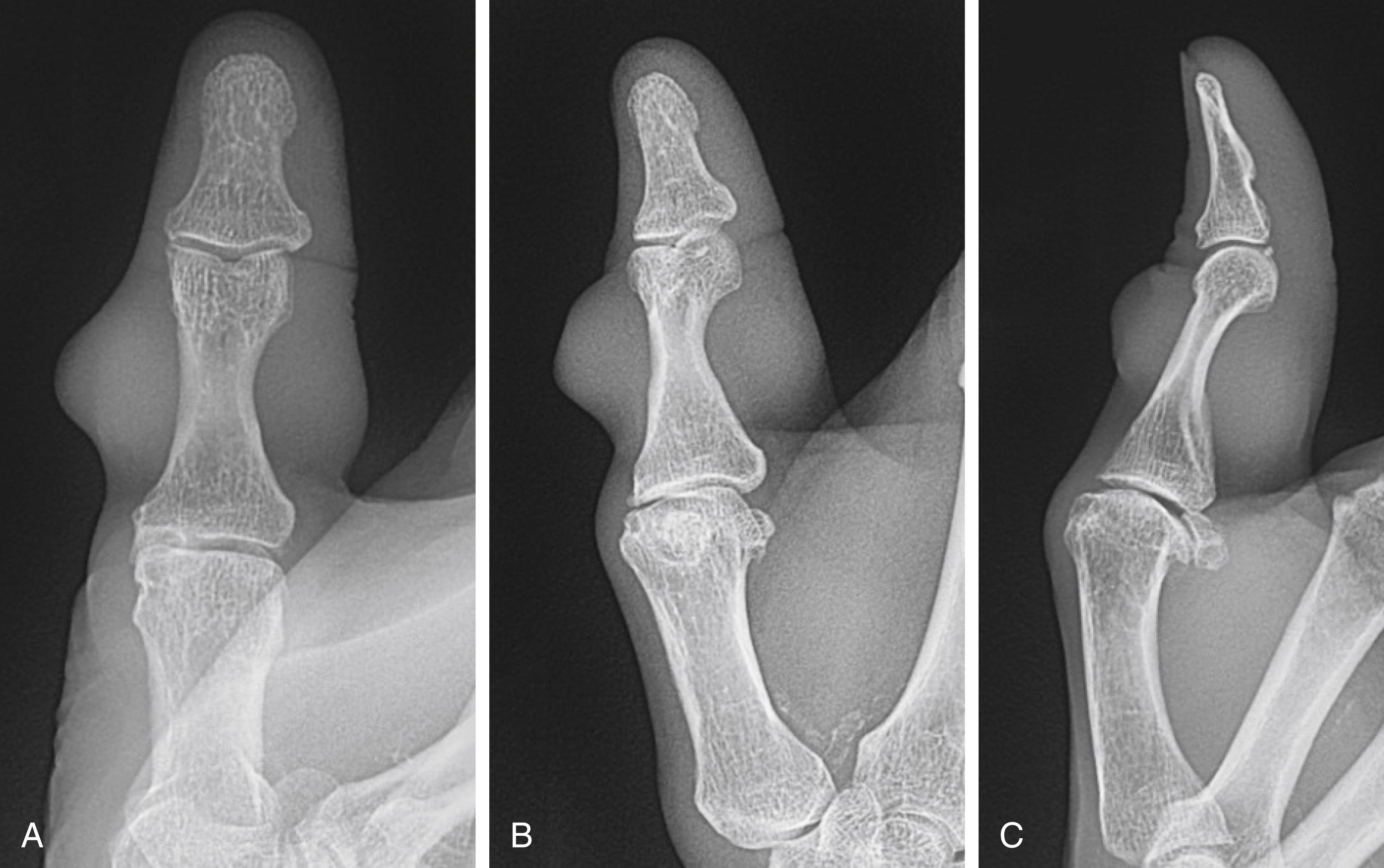
Plain radiographs are the mainstay of work-up for hand masses. The majority of soft tissue lesions will not be directly visualized, however radiographs can help diagnose underlying pathology causing soft tissue manifestations or demonstrate soft tissue calcification as well as distortion or erosion into the bone ( Fig. 60.2 ). Plain radiographs will demonstrate any primary osseous tumor. Well-circumscribed lesions are generally benign and slow-growing, while those that demonstrate periosteal reaction without signs of infection or trauma are worrisome for malignancy.
Magnetic resonance imaging (MRI) provides the highest definition of soft tissue lesions and provides the best information regarding soft tissue planes. MRI’s utility is greatest prior to biopsy, as surgical changes will distort borders of the structures. Generally, intravenous contrast is required in order to truly characterize masses; this is especially true in vascular malformations.
Computerized tomography (CT) is helpful in assessing extent of involvement of masses as well as providing multiplane information for assessment of smaller lesions. This is especially true for lesions that involve the carpal bones, as their relatively small size requires the higher resolution provided by CT. Additional CT scans of distant areas (e.g., chest CT) may also be required to determine the presence of metastatic disease in cases of malignancy.
Ultrasound, while incredibly helpful in imaging soft tissue, is limited by the availability of a skilled technologist and radiologist. Newer ultrasonography machines can provide high-resolution images when available.
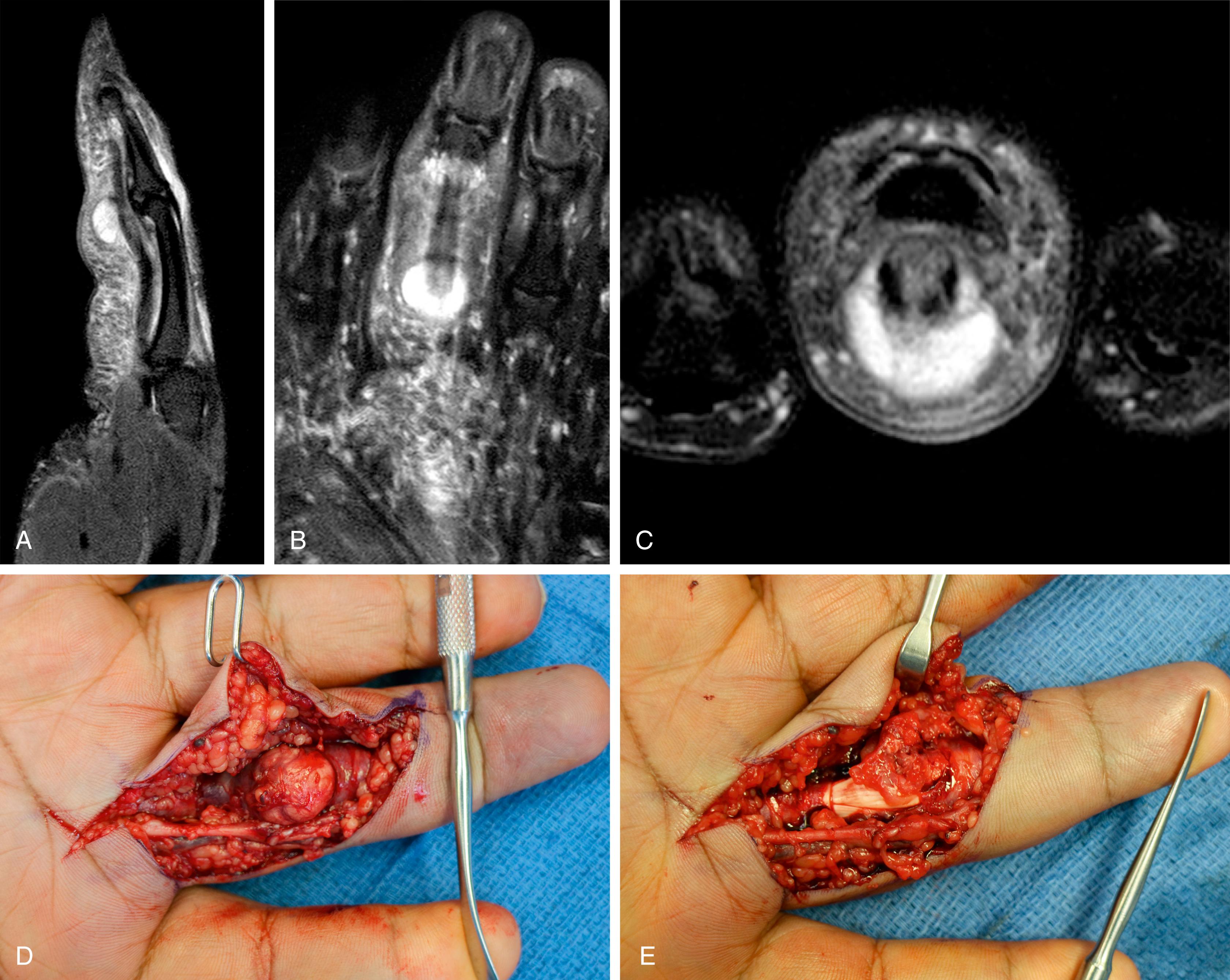
Once a lesion has been thoroughly evaluated, the majority of lesions of the hand are definitively managed with excisional biopsy. In the case of suspected malignancy, the preferred method of tissue diagnosis is incisional biopsy. The possibility of malignancy should be considered whenever performing a ="pg933"/>biopsy, and planning should be done so that any biopsy performed does not hinder the definitive surgery. The incision should be placed longitudinally in a way that it can be excised in the definitive surgery and should be directly over the lesion to prevent creation of a contaminated tunnel. Exsanguination should be through elevation not with the use of an Esmarch bandage. Spreading should be avoided to avoid nearby contamination; infection and gouty tophi ( Fig. 60.3 ) should always be considered as part of the differential, and cultures and cell count should be collected when indicated.
When considering any hand lesion there are a multitude of ways to formulate a differential diagnosis. It is frequently helpful to think of the most common lesions by the location on the hand and the depth of tissue. For instance, a painful lesion under the nail bed with some erosion into the distal phalanx on X-ray is likely to be a glomus tumor. Similarly, the dorsal hand has a high exposure to the sun, consequently skin lesions such as squamous cell carcinoma or basal cell carcinoma are frequently found there. A summary of frequently encountered masses organized by their location on the hand and depth within tissue is found in Table 60.1 .
| Skin | Key Findings | Subcutaneous | Key Findings | Bone | Key Findings | Other | |
|---|---|---|---|---|---|---|---|
| Distal finger | Warts | Rough irregular papules | Mucous cyst | Nail deformity, arthritis of DIP | Glomus tumor | Pain, cold intolerance | Most common site of metastatic disease |
| Finger | Epidermal inclusion cyst | Chronic, occasional inflammation, “cheeselike” discharge | Volar: Giant cell tumor Fibroma |
Firm fixed nodule along tendon course | Enchondroma | Pathologic fracture, lytic bone lesion on radiograph | Nerve sheath tumors along course of Neurovascular bundle |
| Pyogenic granuloma | Bleeding, pedunculated lesion | ||||||
| Hand | Dorsal : Actinic keratosis |
Scaly, crusting lesions | Lipoma | Soft, compressible, freely mobile, no transillumination | Enchondroma | Pathologic fracture, lytic bone lesion on radiograph | |
| Squamous cell carcinoma | Scaly, crusting, bleeding | Volar: Giant cell tumor Fibroma |
Firm fixed nodule along tendon course | ||||
| Basal cell carcinoma | Waxy, pearly papules, Telangiectases | ||||||
| Wrist | Ganglion cyst | Transillumination | Giant cell tumor | Swelling and pain of wrist, large lytic lesion of distal radius |
This chapter aims to discuss the most common masses of the upper extremity. For simplicity, masses are categorized by tissue type and by histologic cell of origin. It is important to note that this organization is primarily pathologic. Clinically, masses of different tissue types are found at varying depths and within other tissue types. For instance, epidermal inclusions cysts, while a mass of skin origin, are most commonly found subcutaneously.
Epidermal inclusion cysts (EIC) are extremely common throughout the body, representing one of the most common lesions of the skin. EICs are also known as inclusion cysts, sebaceous cysts, epithelial cysts, or keratin cysts. However, the name sebaceous cyst implies it is from sebaceous etiology; that is a misnomer and can generate some confusion. The accepted theory of pathogenesis of EICs is the traumatic or embryologic burying of epithelial cells leading to a walled off shedding of keratin with in the affected tissue. Although human papillomavirus (HPV) and exposure to ultraviolet light have also been recently implicated. EICs represent approximately 1%–16% of masses of the hand, with the vast majority – approximately over 70% – presenting on the glabrous skin of the palm and fingers.
EICs generally present as small firm, slowly growing subcutaneous masses that do not transilluminate. The masses may be bothersome but are not generally tender, unless infected. Asymptomatic lesions require no treatment. The preferred treatment of symptomatic EICs is excision of the whole cyst including its capsule without perforating the mass. Complete excision is imperative, as cells that are left behind may continue to shed keratin and lead to recurrence. Excision of the cysts is not recommended when they are acutely infected. In this scenario, open drainage of the cyst followed by a short course of antibiotics is the recommended treatment. Once the acute inflammation has subsided (at least 4 weeks), a smaller excision can be performed with less chance of postoperative infection.
Warts represent one of the most common lesions of the hand in children and young adults. Warts represent infection of human papilloma virus (HPV), which occurs through direct inoculation of the infection from an infected individual or through self-infection. Approximately 70% of warts resolve spontaneously within 2 years, however rarely they can degenerate into a low-grade squamous cell carcinoma known as verrucous carcinoma. , Treatment options shown to decrease time to resolution include topical salicylic acid, topical dinitrochlorobenzene and intralesional immunotherapy. No strong evidence exists for use of cryotherapy despite its widespread use. Recurrent or long-lasting lesions which have been biopsy proven to not represent malignancy may be treated with excision with closure with grafts or secondary intention.
Several primary malignancies of the skin may present as masses in the upper extremity. The most common of these include actinic keratosis, squamous cell carcinoma, basal cell carcinoma, and melanoma. These are discussed in more detail separately in this text, however it is important when evaluating any hand mass that these diagnoses remain within the surgeon’s differential.
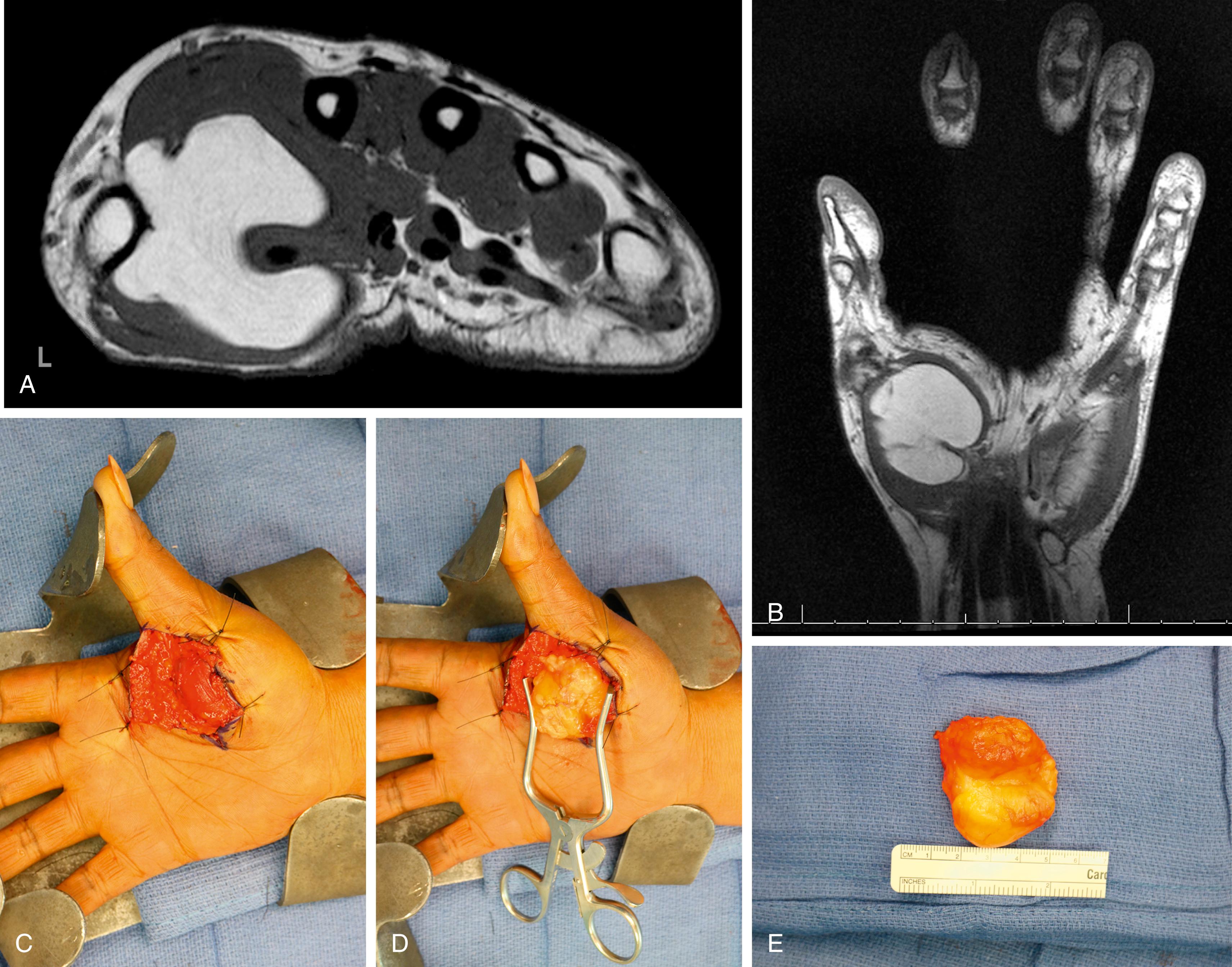
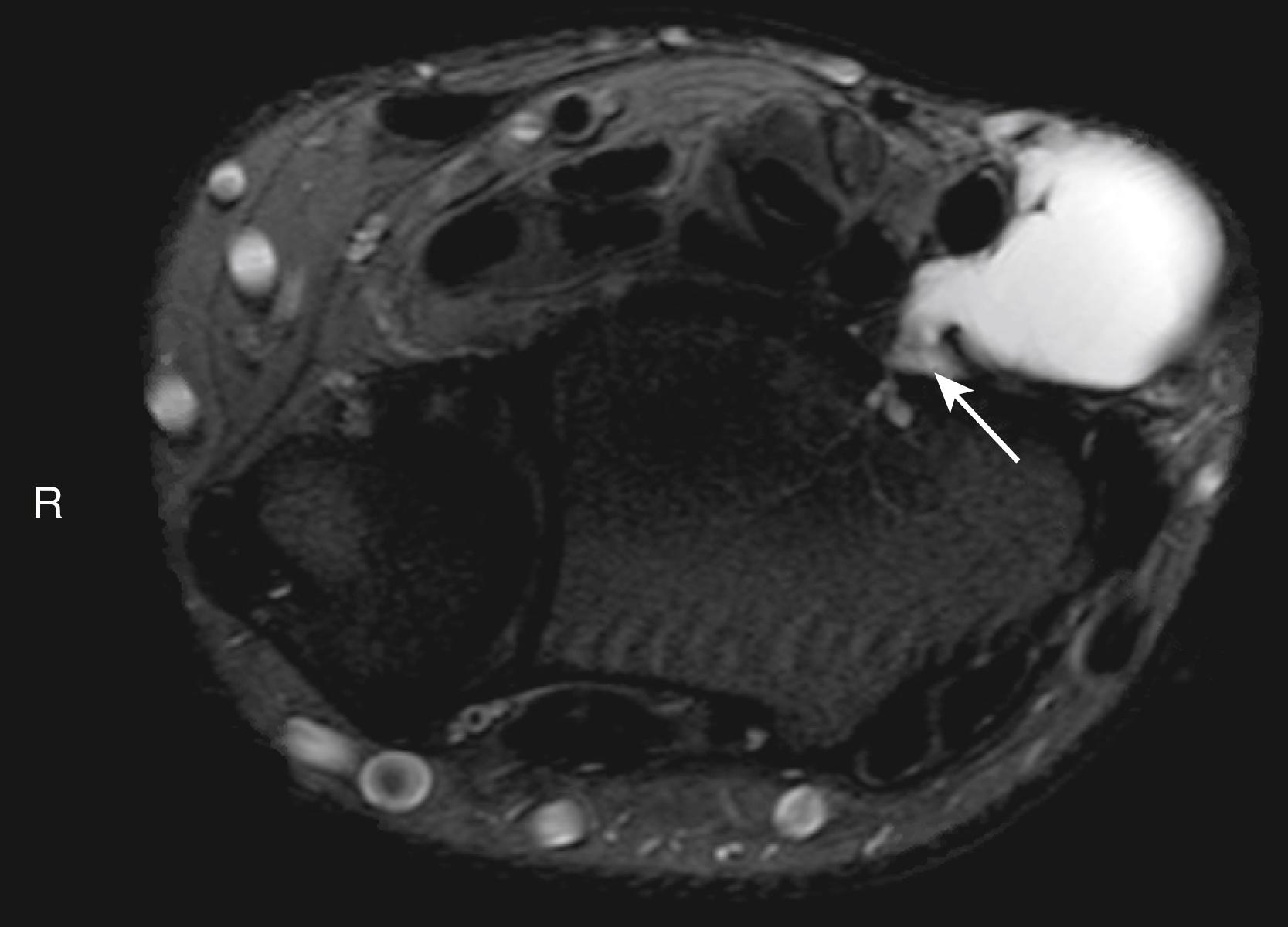
Lipomas represent the most common soft tissue tumor of fat origin, representing approximately 3%–5% of all hand tumors. , While they are most commonly found in other more fatty parts of the body, lipomas can occur anywhere in the hand, including within muscle, nerve, bone or within the deep spaces ( Fig. 60.4 ). Clinically, lipomas present as a slow-growing painless mass that is homogenous, freely mobile, and soft. It does not transilluminate. Generally, they are asymptomatic unless their size causes irritation, or if their location causes compression/irritation of nerves or tendons in the area. Radiographically, lipomas represent a homogenous radiolucent area on plain radiographs. MRI is the preferred imaging modality in order to determine extent of involvement and to rule out malignancy. Heterogeneity or ill-defined borders on MRI suggests possible presence of malignancy. If symptomatic, surgical excision of the lipoma is the preferred treatment method. Generally, lipomas are well encapsulated and surrounded by a layer of loose areolar tissue, allowing them to be easily bluntly excised. Sarcomatous degeneration of lipomas is extremely rare.
Lipoblastomas are rare benign lipomatous tumors found in children less than 7 years of age. They are generally found in the extremities and present similarly to lipomas; however, they are frequently lobulated and histologically are characterized by the presence of a varying range of immature adipose tissue. Excision is generally curative and is recommended in order to definitively rule out the presence of a liposarcoma. Another variant of this condition, known as lipoblastomatosis, is characterized by lack of encapsulation and local infiltration; recurrence is more common in this variant.
Angiolipomas are another tumor of adipose origin, however as the name implies they also contain vascular sinuses. Angiolipomas are benign masses, however they may be locally infiltrative and generally are painful. Lipofibromatous hamartomas or fibrolipomas are rare benign fatty tumors closely associated with a nerve. They have been reported in close association with the radial, ulnar, and median nerves. Given their close association and infiltration of nerves, they frequently cause symptoms of nerve compression. Treatment involves decompression of the nerve without resection, as resection is frequently impossible without sacrifice of the nerve itself. If the diagnosis is not clear, biopsy should performed to confirm the etiology before the tumor is left in situ.
Ganglion cysts represent the most common mass of the hand and wrist. Ganglion is both a general term and the name of a cyst occurring on the dorsum of the wrist. However, ganglion cysts may also be known as mucous cyst when found near the distal interphalangeal (DIP) joint or retinacular cyst when found along the flexor tendon sheath. Despite their high incidence, the pathogenesis of ganglions remains unconfirmed. The name ganglion cyst itself is a misnomer as ganglions lack an epithelial lining and therefore are not true cysts. Ganglions are collagen-lined sacks filled with mucinous material. In the past it was thought ganglion cysts represented synovial herniation from the associated joint, however the lack of synovial lining weakens this theory. Currently, the most accepted theory is that repetitive damage and stretching to the joint capsule creates a one-way valve, which allows synovial fluid to leak. As this leak becomes sealed off, the water component of the fluid is reabsorbed leaving the gelatinous substance that fills the cysts. The fact that ganglions frequently appear at sites of microtrauma such as the scapholunate ligament, the ability to treat ganglions arthroscopically and the need to excise the stalk to prevent recurrence all give credence to this theory.
The vast majority of wrist ganglions present as atraumatic, slow-growing, painless masses, with over 70% located on the dorsal wrist ( Fig. 60.5 ) and approximately 20% located on the volar wrist. Typically, ganglions are asymptomatic, although dorsal ganglions may cause discomfort when extending the wrist. Patients frequently describe the mass swelling with activity and decreasing in size with rest. On examination ganglion cysts typically are firm, round lesions that transilluminate. Dorsally, ganglion cysts most frequently arise from the scapholunate ligament; volarly they commonly originate from the scaphotrapezium–trapezoid joint. Asymptomatic ganglion cysts require no treatment, however when treatment is indicated, management is through direct surgical excision. Aspiration of the cyst has a high recurrence rate. During surgical excision, it is essential to locate and remove the stalk of the lesion to prevent recurrence; cauterizing the base of the lesion is also recommended to devitalize any microscopic remnants left behind. When treating volar ganglions, care must be taken to avoid the radial artery, as the lesions are frequently intimately associated with the artery ( Fig. 60.6 ). For this reason, we routinely obtain MRI on volar ganglions to assist with surgical planning.
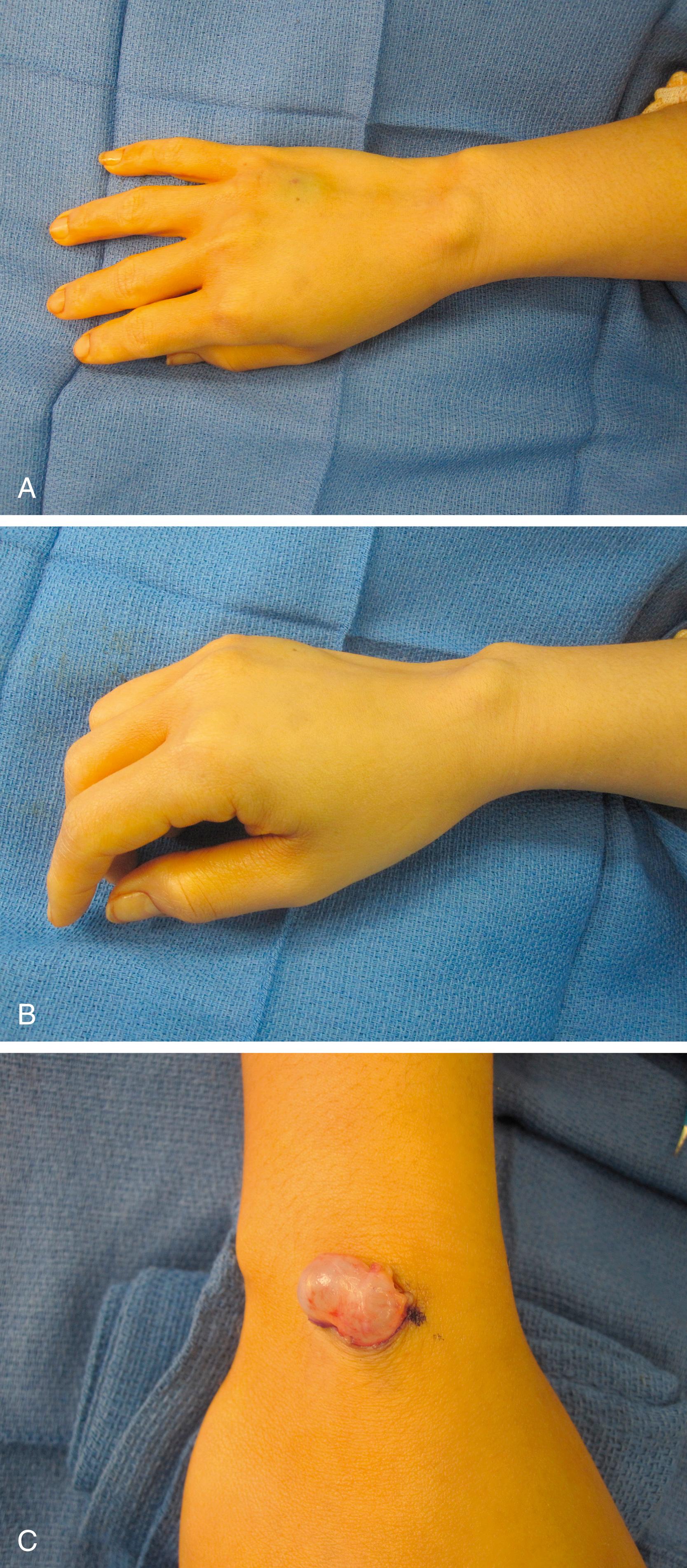
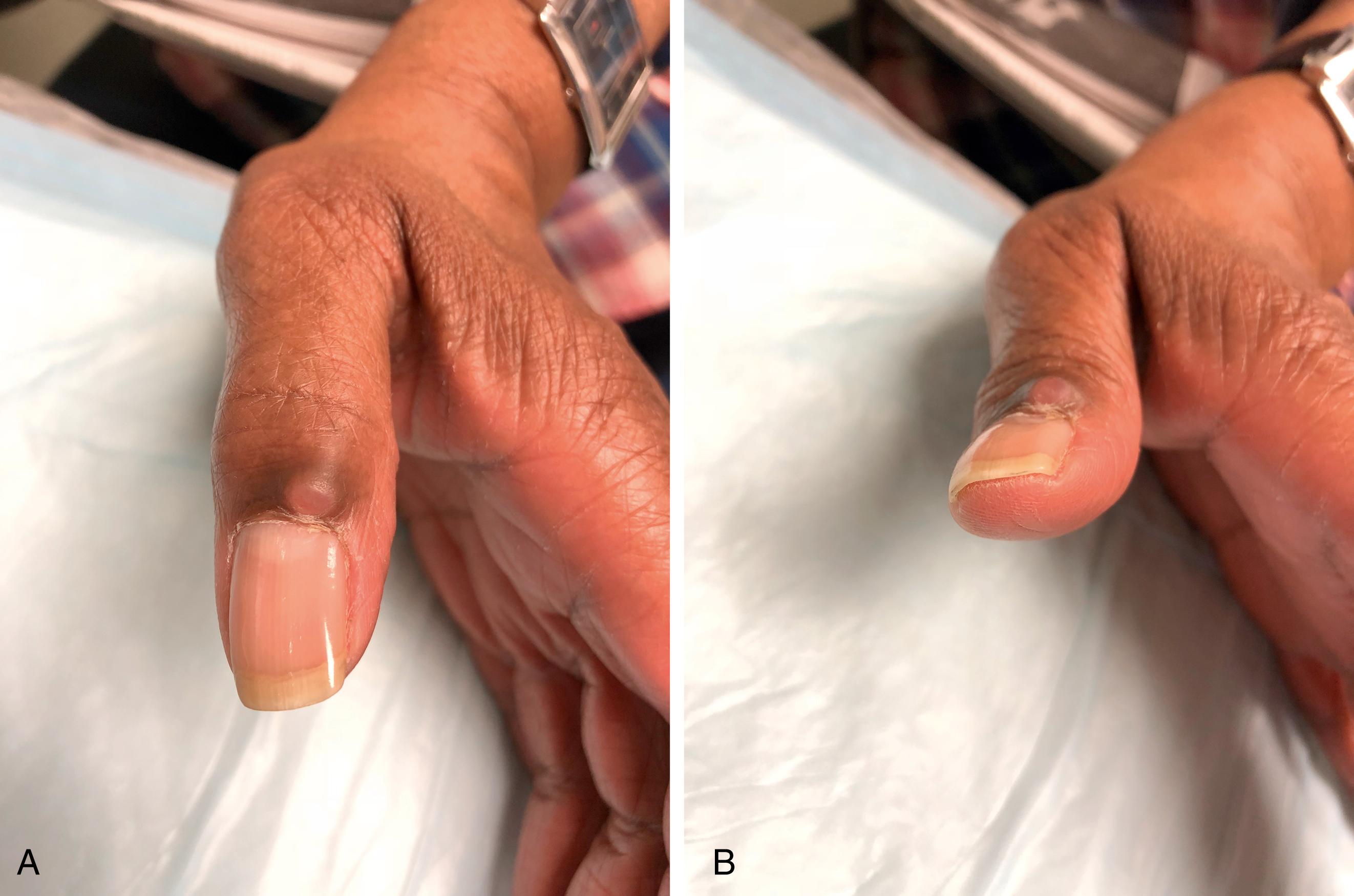
Mucous cysts typically present as a lesion on the dorsal distal phalanx proximal to the nail fold. Patients may complain of pain in the DIP joint as mucous cysts are associated with DIP joint arthritis. X-rays of the finger will often demonstrate dorsal osteophytes of the joint. Occasionally the only presenting symptom may be an abnormal nail plate when the cyst is located over the germinal matrix ( Fig. 60.7 ). When removing mucous cysts, excision of any associated osteophytes should be performed to prevent recurrence.
Retinacular cysts occur volarly along the flexor tendon sheath (see Fig. 60.1 ). Diagnosis can often be made by transillumination. Repeated aspiration of retinacular cysts has an approximately 80% cure rate. Surgical excision is reserved for cases of recurrence.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here