Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Exertional leg pain (ELP) is a common problem encountered in recreational and competitive athletes. Although its incidence in the general population is unknown, ELP is thought to affect between 12.8% and 82.4% of athletes. Specifically, at least 45% of runners will experience such pain, with running more than 40 miles per week serving as a significant risk factor. Defined as pain distal to the knee and proximal to the talocrural joint, ELP can be a disabling condition whose specific cause can present a diagnostic challenge to even the most astute physician. One aspect of this conundrum rests in the associated broad differential, which is detailed in Table 113.1 . Another difficulty in pinpointing the cause of ELP is that the aforementioned differential components can coexist in the same athlete. Although each of these ELP etiologies is noteworthy, this chapter will focus on the musculoskeletal causes, specifically chronic exertional compartment syndrome (CECS).
| Musculoskeletal |
| Medial tibial stress syndrome (MTSS) |
| Tibial bone stress injury (previously stress fracture) |
| Chronic exertional compartment syndrome |
| Muscle strains |
| Fascial herniation |
| Tendinopathy |
| Vascular |
| Popliteal artery entrapment syndrome |
| Arterial endofibrosis |
| Intermittent claudication |
| Venous insufficiency |
| Neurologic |
| Spinal stenosis |
| Peripheral or central nerve entrapment/impingement |
| Referred pain from proximal joints (e.g., hip, knee) |
| Tumor |
| Infection |
Activity-induced compartment syndrome of the leg was first suggested in 1943 when Vogt described “march gangrene.” The description of this condition and its association with military training continued to evolve in the 1950s. Mavor was the first to detail CECS in sport when he reported the case of a professional soccer player noted to have recurrent anterior leg pain and muscle herniation. This player was treated with a fasciotomy and fascia lata grafting, resulting in complete resolution of his symptoms and a subsequent similar surgery on the other anterior leg. The athlete returned to his previous high level of function without documented complications. Through a review of the current understanding of the anatomy implicated in CECS, patient presentation highlights, optimal diagnostic evaluation, and treatment options, the goal is to return patients to activity just as Mavor reported doing more than 50 years ago.
The true incidence of ELP is unknown, with reports attempting to address this issue varying widely. This variation likely stems from the difficulty in making a firm diagnosis and the potential for symptom overlap between the numerous causes of ELP. With that said, medial tibial stress syndrome (MTSS) and CECS account for the majority of the cases of exercise-induced leg pain. MTSS is thought to represent between 13.6% and 42.0% of these cases. Meanwhile, CECS is reported to account for 14% to 33%.
Identifying the typical population affected by CECS can assist in making the diagnosis. This condition is most common in athletes and individuals involved in repetitive exertional/loading activities. It has been reported that 87% of patients with CECS are involved in sports, with 69% of these cases occurring in runners. On the other hand, it can occur in a wide variety of other sports as well, including basketball, skating, and soccer. However, nonathletes can also be affected by this condition. For instance, in one study, 90% of patients without vascular etiologies for ELP were found to have CECS. Men are thought to be affected at the same rate as women, with the mean age of presentation between 26 and 28 years old. Detmer et al. reported that in the 100 cases that they assessed the mean time to diagnosis was 22 months. In this population the diagnosis of CECS was present bilaterally in 82 patients. It is worth noting that, although CECS is present in the lower leg 95% of the time, it can also be found in the forearm, thigh, and foot.
There are four muscle compartments in the lower extremity ( Fig. 113.1 ). In addition, the deep posterior compartment may also contain a fifth compartment, which houses only the tibialis posterior. It is important to remember this potential anatomic variation because it can serve as a cause for a delayed diagnosis and/or a failed surgical intervention. Regardless, each compartment is bound by bone and sits within its own investing fascia. In CECS the most common compartment involved is the anterior compartment (45% to 60%), followed by the deep posterior compartment (32% to 60%). In a significant portion of these cases, both the anterior and posterior compartments can be symptomatic simultaneously. The lateral compartment (12% to 35%) and superficial posterior compartment (2% to 20%) are much less likely to be affected.
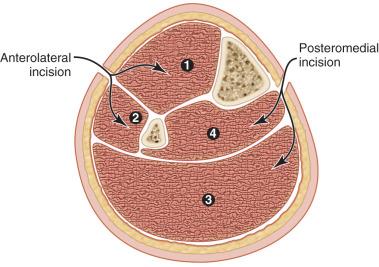
Each compartment (aside from the fifth compartment) contains one or more muscles and one major neurovascular structure ( Table 113.2 ).
There are a couple of noteworthy anatomic considerations herein. As indicated previously, the anterior compartment is most commonly implicated in CECS, likely due to its high vulnerability to injury and relatively limited compartment compliance. Meanwhile, due to the very thin, pliable fascia, the superficial posterior compartment is the least likely to be the source of CECS. Lastly, the superficial peroneal nerve exits the fascia of the lateral compartment adjacent to the intramuscular septum (IMS), approximately 11 cm proximal to the inferior aspect of the lateral malleolus. This anatomic landmark is particularly relevant because this is where herniations may occur, resulting in CECS symptoms and/or nerve entrapment.
The pathophysiology resulting in pain attributed to CECS is not known. During exercise, normal muscle will increase by a volume of up to 20%. Even in asymptomatic individuals intracompartmental pressures will increase. The increase was initially attributed to thickened compartment fascia with a subsequent decrease in fascial compliance; however, this theory is currently questioned. Other potential theories to explain the increase in compartment pressure with exertion include stiff connective tissue, vascular congestion, reduced microcirculatory capacity, and increased muscle mass within a compartment. Furthermore, the rationale for why increased intracompartmental pressures produce pain has not been elucidated. Current speculation includes muscle and/or nerve deoxygenation, direct stimulation of fascial and/or periosteal sensory nerves, or the release of local kinins being the cause. Some have even questioned if the increased pressure in CECS is a consequence of the underlying physiologic process rather than the cause of the associated pain.
There are additional factors or associations that may shed light on the pathophysiology of CECS. Anabolic steroids and eccentric exercises induce muscular hypertrophy, increase intracompartmental pressures, and decrease fascial elasticity, all of which may predispose one to developing CECS. Creatine supplements have been shown to increase anterior compartment pressure as well. Posttraumatic soft tissue inflammation, myofascial scarring, and venous hypertension all may also contribute to the pathophysiology of CECS. In addition, sympathetic blockade has been shown to reduce the pain of CECS, inferring that there may be some vascular spasm secondary to sympathetic stimulation. Regardless of the cause or mechanism for inciting pain, once the intracompartmental pressure exceeds the ability of the compartment to accommodate the change, pathologic pressure changes occur and result in CECS.
Compartment syndromes may be classified as either acute or chronic. Acute compartment syndromes represent a surgical emergency that can lead to devastating injury with loss of function and potentially the loss of a limb. Although the vast majority involve men (91%, with an average age of 32 years old), they are typically associated with trauma (36% involve tibial diaphyseal fractures) or an ischemic event. They have also been described in the setting of exercise (e.g., untrained individuals who initiate a training program), with increases or changes in a training program, or with athletic injuries. The immediate management of these injuries involves wide surgical decompression to avoid serious and long-term sequelae.
Conversely, exertional compartment syndromes are less severe. They are symptomatic only during exercise and typically slowly resolve upon stopping the associated activity. Exertional compartment syndromes generally do not require acute surgical decompression. However, they can progress or convert to an acute compartment syndrome.
No classification system has been associated with the diagnosis of CECS. In general, the specific compartments involved are simply described. Of note, there is a high incidence of bilateral involvement, which occurs in up to 82% of cases. With that said, the identical compartments may not be affected in each limb.
A key in teasing out the diagnosis of CECS from the larger category of ELP lies in the clinical history. Patients classically describe leg pain that occurs after a specific volume of exertion (i.e., duration, distance, or intensity), often times following a change in training. It typically occurs after a stereotypic exercise duration or intensity. In addition, changes in footwear or training surface have also been implicated. Pain at rest should alert the clinician to search for other causes. And because the vast majority of cases occur bilaterally, unilateral lower leg involvement should prompt the treating physician to consider other causes of ELP and/or biomechanical abnormalities.
The pain is often described as a pressure, fullness, burning, or cramp-like sensation. Sometimes the patient will note a sharpness of the pain with continued activity. If the athlete continues to exercise at the same or an increased intensity level, the pain typically progresses. Inevitably, most athletes will not be able to continue at this level of exercise. Occasionally, decreased performance may be reported the day after the symptomatic exercise is performed.
Patients may also complain of paresthesias and in some cases weakness related to compression of the nerve passing through the affected compartment. These symptoms typically occur in a sensorimotor distribution. These key features can often help to differentiate CECS from MTSS and tibial bone stress injury, two other common causes of ELP. However, the astute physician should note that such neurologic symptoms may accompany other causes of ELP, including popliteal artery entrapment syndrome.
An important feature of CECS is that the associated pain abates with decreased intensity, or more likely cessation of the provocative activity. Athletes can often predict the point or intensity at which symptoms will occur. However, over time the necessary recovery time may increase. Symptoms typically return with subsequent exercise sessions that are of similar intensity or duration. In extreme circumstances when the athlete continues to compete through the pain, acute compartment syndrome and rhabdomyolysis can occur.
Unlike MTSS and tibial bone stress injury, the physical examination at rest in CECS is completely normal. For example, there is generally no tenderness to palpation of the lower leg. In such cases, further examination after engaging the athlete in the provocative activity is mandatory. Subsequently, diffuse tenderness to palpation of the affected compartment/muscle group may be present. After exercise, passive stretching of the involved muscle groups may precipitate pain as well. Swelling or increased tissue tension may be detectable. Muscle herniations are not uncommon, especially at the exit site of cutaneous nerves. Lastly, the patient may exhibit neurologic impairments in the sensorimotor nerve distribution of the affected compartment.
Recollection of the nerve distributions and functions can sometimes assist in the diagnosis of CECS. For instance, when the anterior compartment is involved, compression of the deep peroneal nerve can occur. This can result in dysesthesias over the dorsum of the foot (particularly the web space of the great toe), a foot drop, or the sensation of loss of ankle control. When the lateral compartment is affected, there may be weakness of foot eversion and/or loss of sensation over the anterolateral shin and dorsum of the foot. With deep posterior compartment involvement, there may be weakness of the foot muscles and loss or abnormal sensation along the plantar aspect of the foot.
If the patient's presentation and physical examination do not clearly point toward CECS, further imaging may be beneficial. One might consider plain films, bone scans, and/or magnetic resonance imaging (MRI) modalities. Because they should be normal in the setting of CECS, the value of these images lies in identifying or excluding other etiologies of ELP (e.g., tibial bone stress injury). In addition, vascular studies may be valuable. An example is ankle-brachial index (ABI) testing with ankle provocation maneuvers, which can assist in ruling in or out popliteal artery entrapment syndrome. Computed tomography (CT) scans with angiography and MRI with or without angiography may be similarly beneficial in this context.
Attempts have been made to identify imaging or other modalities that might verify the diagnosis of CECS. Functional imaging modalities (e.g., thallium scintigraphy, thallium single-photon emission CT, methoxyisobutylisonitrile, 99m Tc-tetrofosmin single-photon emission CT, and functional MRI) have all been studied to assess their utility in this regard but have not been shown to be clinically useful at this juncture. Preliminarily, ultrasound may have a role in aiding with diagnosing CECS. One study showed its efficacy in detecting a significant increase in anterior compartment thickness in CECS. However, more research appears necessary to validate its use. Some studies have demonstrated promise for near-infrared spectroscopy, which can detect decreased tissue oxygenation and delayed reoxygenation postexercise in CECS. Early research indicates that this modality may approach the same diagnostic accuracy as intracompartmental pressure testing, but more studies are needed. Nerve conduction studies following provocative activity have been assessed for this purpose but are not diagnostic of CECS. However, there is a report that an absent extensor digitorum brevis F wave was identified in a patient with anterior compartment CECS. This modality requires further evaluation before it is adopted clinically.
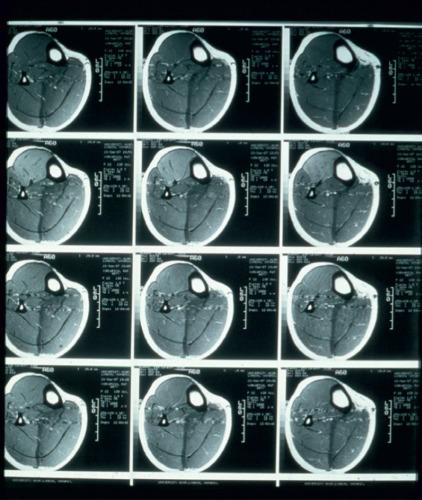
There remains current debate about the utility of the postexertion MRI in diagnosing CECS. Increased T2 signal intensity in the affected compartment that resolves with rest has been appreciated in some studies. It is thought that the increased signal is secondary to the recruitment of muscle fibers during activity that results in increased interstitial water content, independent of vascular patency ( Fig. 113.2 ). Yet, there are only two studies that have produced a validated technique for diagnosing anterior compartment CECS with MRI. Again, more research in this realm is warranted.
Ultimately, CECS, like acute compartment syndrome, continues to be a clinical diagnosis. First described in 1962, intracompartmental pressure testing remains the primary means by which to further cement a clinical suspicion for CECS. Numerous devices, techniques, and protocols have been used to this end. Studies have monitored pressures at rest and during and after exercise. However, the difficulty of measuring pressures during exercise makes it impractical in most settings. The most widely cited criterion for the diagnosis of CECS comes from Pedowitz et al. ( Table 113.3 ). Only one of the criteria is necessary to make the diagnosis of CECS. Preexercise pressures greater than 15 mm Hg and 1-minute and 5-minute postexercise pressures greater than 30 mm Hg and 20 mm Hg, respectively, are considered abnormal.
| Preexercise pressure ≥15 mm Hg |
| 1-minute postexercise pressure ≥30 mm Hg |
| 5-minute postexercise pressure ≥20 mm Hg |
a Only one abnormal measurement is needed to suggest chronic exertional compartment syndrome.
There are at least two literature reviews evaluating studies on compartment pressure testing and the referenced criteria that note important limitations. Both reviews point out a general lack of protocol standardization, an absence of validated control groups, and a significant degree of overlap in pressures recorded between control groups and symptomatic groups. Based on a systematic review, Aweid et al. propose that the only time point where there was no significant overlap between the symptomatic and control groups is 1-minute postexercise. At that point, pressures greater than 27.5 mm Hg are highly suggestive of CECS. Recently, it has been suggested that further modifying the Pedowitz criteria may improve the sensitivity and specificity of intracompartmental pressure testing for diagnosing CECS. Roberts et al. report that this could be achieved by lowering the preexercise threshold to 14 mm Hg, increasing the 1-minute postexercise cutoff to 35 mm Hg, and increasing the 5-minute postexercise diagnostic threshold to 23 mm Hg ( Table 113.4 ).
| Preexercise pressure >14 mm Hg |
| 1-minute postexercise pressure >35 mm Hg |
| 5-minute postexercise pressure >23 mm Hg |
a Only one abnormal measurement is needed to suggest chronic exertional compartment syndrome.
An important related issue with intracompartmental pressure testing is the specific exercise protocol used to secure these values. At this time there is no clear exercise protocol for intracompartmental pressure testing. Some have suggested that patients exercise until the symptoms can no longer be tolerated, at which point postexercise testing should be performed. The lack of standardization of this aspect of the assessment for CECS has called into question the applicability of the criteria established by Pedowitz and colleagues. Specifically, if a patient does not exercise similarly to the participants in the study that generated the criteria it may invalidate the subsequent results. More research into this issue is needed moving forward.
Compartment pressures can be reliably measured using the Stryker Intra-Compartmental Pressure Monitor (STIC; Stryker Orthopaedics, Mawah, NJ). This device has been validated with in vitro models possessing known pressures. The STIC can be used for continuous monitoring but is more commonly used for intermittent monitoring with percutaneous needle penetration into the compartment. Various types of catheters or needles can be used (e.g., wick catheters, slit catheters, side port needles, and straight needles). Although there has been debate as to which of these options provide the most accurate results, evidence suggests that the slit catheter, side port needle, and straight needle all function with similar accuracy. Practically, an international survey found that the side port needle was most commonly used for intracompartmental pressure testing.
Currently there is no validated protocol regarding intracompartmental pressure testing, specifically as it pertains to the position, depth, and angle of the needle or catheter used. The following protocol recommendations stem from a combination of the current available evidence on the topic and the authors’ preferences.
The patient should be placed supine on a table for the pressure measurements (except the superficial posterior compartment, which should be measured with the patient prone). Positioning the knee at 10 degrees of flexion with the ankle at neutral or slight plantar flexion can help to avoid artificially raising or lowering the compartment pressures. The location for the measurements to be taken should be marked on the skin with indelible ink. To identify the optimal sites of entry, visualize or draw a line around the junction of the proximal and middle thirds of the lower leg. The needle placement can then occur within 3 cm of this line in the appropriate compartment. Further recommendations regarding the optimal entry site, depth of insertion, and means to confirm proper placement can be found in Table 113.5 .
| Compartment | Entry Site | Depth | Confirmed By |
|---|---|---|---|
| Anterior | 1 cm lateral to the anterior tibia border | 1–3 cm | Plantarflexion or dorsiflexion of the foot |
| Deep posterior | Posterior to the medial tibia border | 2–4 cm | Toe extension Ankle eversion |
| Lateral | Anterior to the posterior border of the fibula | 1–1.5 cm | Foot/ankle inversion |
| Superficial posterior | 3–5 cm on either side of the vertical middle of the calf | 2–4 cm | Dorsiflexion of the foot |
a All points of entry should occur at the junction of the proximal and middle thirds of the lower leg.
Prior to measuring the intracompartmental pressures, the skin should be anesthetized with local anesthetic and prepped in an aseptic fashion. The monitor device should be held horizontally and zeroed before each pressure reading. No standard angle of entry has been agreed upon, but an angle of 45 degrees to the skin is reproducible, minimizes discomfort, and permits a reasonable depth. The compartments can then be tested individually at a needle/catheter insertion depth as suggested previously (see Table 113.5 ). With each pressure measurement a small amount of fluid is injected and the reading is recorded. Care should be taken not to depress the syringe too quickly because this may create an artificially elevated reading. In addition, avoid pulling back on the syringe while it is inserted, as this may result in a piece of tissue becoming lodged in the needle/catheter. To further verify the placement of the needle in a given compartment, certain movements can be performed that should increase the pressure reading (see Table 113.5 ). Consideration should be given to testing both lower legs given the high incidence of bilateral involvement in CECS.
As a related aside, the role and impact of ultrasound guidance in intracompartmental testing has been analyzed. Wiley and colleagues have shown that ultrasound-guided insertion allows for a safe, reliable, and reproducible method for proper needle placement in the deep tibialis posterior compartment. Despite this evidence, it does not appear that ultrasound guidance is necessary for routine deep and superficial posterior leg compartment pressure testing. The accuracy in testing both types of compartments is similar, regardless of the experience of the investigator.
The treatment of CECS can include either conservative or surgical measures. Among the conservative treatment options is the avoidance of the offending activity or activities that cause pain. Understandably, this option may not be satisfactory for some patients, and in those instances other options should be considered.
The modification of extrinsic factors may be of some benefit. Assessing for possible changes to the training surface, choice of footwear, and/or the training program itself could lead to a decrease in ELP. In addition, nonoperative treatments such as physical therapy, antiinflammatory medications, stretching, and orthotics can be used in the initial management of suspected CECS. Physical therapy, focusing on stretching and strengthening programs, can address potential mechanical factors related to the lower limb and core.
One may also pursue gait modifications to alter the biomechanical forces traveling through the affected compartment. A specific gait modification that has shown some promise is forefoot running. Diebal and colleagues found that such a running technique was effective in treating anterior compartment syndrome. Patients in these studies experienced decreased symptoms and decreased intracompartmental pressures. Also of note, surgical intervention was avoided in these patients.
Other nonoperative methods used have included deep tissue massage, myofascial release, and ultrasound. A newer treatment option features the injection botulinum toxin A into the musculature of the involved compartment(s). Reported in two case series, this treatment was shown to be effective in the treatment of anterior and lateral compartment CECS. There are (at least) two noteworthy considerations for this potential treatment. First, a reduction of strength was reported in one study, which may limit its applicability in some patients. Second, repeat injections may be necessary because reinnervation takes place over 6 to 9 months following such a treatment.
If the response to the aforementioned conservative measures does not allow the athlete to return to the desired level of activity, operative treatment should be considered. An adequate trial of conservative measures is generally considered to be in the range of 3 to 6 months.
Surgical treatment entails an open or endoscopic fasciotomy, with or without fasciectomy, and resection of any fascial bands. No direct comparison with fasciotomy or between open and endoscopic procedures exists. When a fascial herniation is present it must be included in the release to avoid recurrent symptoms that can occur if neglected. When surgery is pursued, all symptomatic compartments should be addressed with surgical release. Previously, those individuals with anterior symptoms had anterior and lateral compartments released. Schepsis and colleagues found that, in patients with complaints isolated to the anterior compartment, isolated release of the anterior compartment produced results equal to a combined anterior and lateral compartment release. It is now generally accepted that surgical release should be performed only on the symptomatic compartments.
The current trend is for limited incision techniques with a rapid return to weight bearing, motion, and resumption of activity. Initially, success rates were reported to be in the 80% to 90% range. However, the success for deep posterior compartment surgical release has been shown to be between 30% and 65%, possibly due to the presence of the fifth compartment and/or the complex nature of this particular surgery. In addition, a more recent study in a military population was less optimistic on the success of surgical fasciotomies for CECS. In this study, 44.7% of patients experienced symptom recurrence and 27.7% of patients were unable to return to full activity. It is worth noting that surgical complication rates have been reported to be as high as 16%.
Single- and double-incision techniques are available to release the anterior and lateral compartments of the leg. We prefer to use a single-incision technique because it is simple. The IMS is usually palpable digitally by placing firm pressure over the anterior lateral leg and moving in a horizontal motion midway between the anterior crest of the tibia and the fibula. A vertical incision is based over the palpated IMS or centered between the anterior tibial crest and the fibula if the IMS is not easily found. This incision should be centered vertically between the fibular head and the lateral malleolus and should extend approximately 3 cm. Soft tissue dissection should then be completed carefully until the fascia is identified and exposed. Once the fascia is exposed, the IMS is usually easily visually and palpably identifiable. After the IMS is identified, the fascia should be bluntly separated from the subcutaneous tissue in the superior and inferior directions. We prefer doing this with blunt mayo or Metzenbaum scissors with the tips pointed toward the fascia and pressure placed downward on the fascia. Run the tips of the scissors along the fascia away from the incision, with the blades closed, and then open them and bring them back toward the incision. After this is completed both superiorly and inferiorly, a small rent should be created in the fascia approximately 5 mm anterior to the IMS. The fascia is then separated from the underlying muscle in a similar fashion but with the tips of the scissors inside the fascia, with the tips facing anterior and with pressure anterior against the fascia. The scissors are advanced along the fascia with the tips closed. The tips are then opened at the end of the desired fasciotomy and brought back towards the opened rent. Once the fascia has been separated from the overlying subcutaneous tissue and the underlying muscle, it is divided superiorly and inferiorly. This is done by opening the tips of the scissors creating a 2 mm gap between the tips. The fascia is placed between the tips at the superior end of the previously created rent in the fascia, and the scissors are pushed proximally to the desired extent of the fasciotomy and then withdrawn. The inferior fascia is opened in a similar fashion, and then the lateral compartment is addressed using the previous steps through a rent created 5 mm posterior to the IMS. It is strongly urged to thoroughly separate the fascia from the underlying and overlying tissue prior to dividing it and to remove the scissors after the fasciotomy without closing the blades. Digital palpation after the fasciotomy can ensure that it was done in a complete fashion. The fasciotomy should extend distally to the superficial extensor retinaculum but not beyond. Superiorly, the lateral compartment release should stop well before the peroneal nerve (if palpable) or 4–5 cm distal to the fibular head (if the nerve is not palpable).
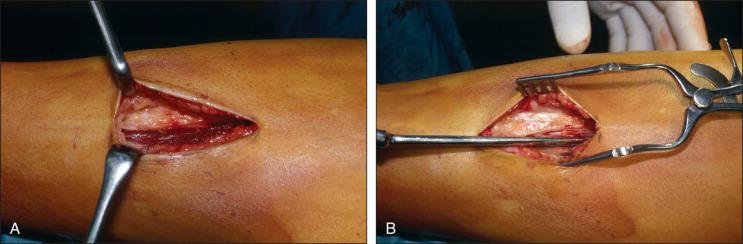
We use a single-incision technique for the release of the superficial and deep posterior compartments as well. The incision is located 1–2 cm posterior to the posterior subcutaneous border of the tibia. It is centered at the level of the gastrocnemius musculocutaneous junction and is 3–4 cm long ( Fig. 113.3A ). The long saphenous nerve and vein are usually in the center of the field and are identified on the posteromedial border of the tibia during soft tissue dissection, which is carefully undertaken down to the level of the fascia. A small vertical incision is created in the fascia adjacent to the tibia after the fascia is separated from the subcutaneous tissue proximally and distally as outlined previously for the anterior and lateral releases. A small incision is made just posterior to the tibia, and the posterior compartment is entered. Separate the fascia from the underlying muscle as outlined previously, and then release the fascia in a similar fashion to what was described for the anterior and lateral compartments. The soleus will be encountered in the proximal one-third of the tibia at the soleus bridge. Complete release of this structure is necessary because it also represents the proximal confluence of the flexor hallucis longus (FHL) and flexor digitorum longus (FDL) fascia. This releases the deep posterior compartment. An elevator can then be used to release the tibialis posterior muscle off the tibia, completing the release of the tibialis posterior from the tibia (see Fig. 113.3B ). Remaining on the posterior aspect of the tibia throughout the release ensures safety of the posterior tibial neurovascular bundle, which is posterior to the tibialis posterior and FDL. Digitally palpate the entire compartment to ensure that the release is completed adequately. The gastrocnemius can be identified through the medial incision and proximal to it. This muscle can be released in a similar fashion. Following the releases, the tourniquet is relaxed, if used, and hemostasis is obtained. The subcutaneous tissues and skin are closed and dressed in the preferred fashion, and a compressive dressing is applied.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here