Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The latissimus dorsi flap was introduced by Tansini in 1906 for the coverage of extensive mastectomy defects. Subsequently forgotten, it was re-described by Olivari in 1976 for the coverage of large radiation ulcers of the chest wall. Boswick, in 1978, adopted Olivari's idea and developed a latissimus island flap for breast reconstruction. A further development, together with the technical progress of microsurgery, was its use as a free musculocutaneous flap.
The latissimus dorsi flap, either as pedicled or as microvascular free tissue transfer, is one of the most commonly used flaps in reconstructive surgery, with large vessel diameters and a long reliable pedicle. Its size and versatility make it an extraordinary graft that has been a workhorse in reconstructive surgery for more than two decades.
It can be elevated as a muscle, a musculocutaneous or an osteomyocutaneous flap. As a composite graft including variable amounts of muscle, skin, and subcutaneous tissue, it can be used in any variety for reconstruction in every area of the body. The harvested flap can be as large as 20 × 35 cm, but numerous combinations with other flaps nourished by the subscapular system are possible to simultaneously reconstruct more complex defects with several flaps, based on a single pedicle.
The latissimus dorsi muscle is the mirror image of the pectoralis major muscle. Its aponeurotic origin arises from a broad front, extending from the seventh and lower thoracic vertebrae, the lumbar and sacral spinal processes, to the posterior and middle outer rim of the iliac crest via the thoracodorsal fascia. The superior portion of the medial aspect of the latissimus muscle is covered by the trapezius muscle; otherwise, the latissimus muscle is superficial to all other muscles in the back. The latissimus muscle covers a portion of the paraspinal muscle and the majority of the serratus anterior muscle. In the middle portion there is a rather tight attachment to the 10th, 11th, and 12th ribs and to the fibers that interdigitate with fibers of the serratus anterior muscles. Superiorly it is adherent to the inferior border of the teres major muscle. Its triangular large and flat muscle belly converges into a flat, broad tendon. Near its insertion into the lesser tubercle and the medial lip of the intertubercular groove of the humerus ( Figure 41.2 ) it spirals 180° around and travels anterior to the tendon of the teres major muscle.
There are numerous important functions of the latissimus dorsi muscle. Primarily it acts as an extender, adductor, and medial rotator of the humerus. It holds the inferior angle of the scapula against the chest wall and stabilizes and elevates the pelvis when bringing the lower extremity forward. It aids in coughing and, unduplicated by other muscles, it pulls the arm posteriorly, directly behind the back, a motion that is best described by the terminal action of pushing off with a ski pole.
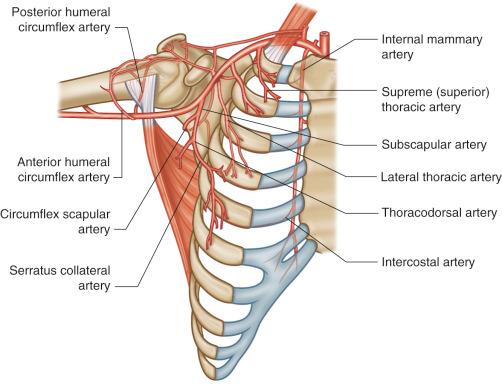
The latissimus dorsi muscle has a dual blood supply from the subscapular artery and the posterior paraspinous perforators. Both circulatory systems are diffusely interconnected so that the muscle can survive in its entirety if either pedicle is interrupted.
thoracodorsal artery, a branch of the subscapular artery
Length: 8.5 cm (range 6.5–12 cm)
Diameter: 3 mm (range 2–4 mm)
The thoracodorsal artery courses from the axilla along the anterior border of the latissimus dorsi muscle, enters the muscle from underneath, and spreads into two or three major branches at the undersurface of the muscle. Anatomic variations can be seen where the thoracodorsal artery can arise directly from the axillary artery or even from the lateral thoracic artery in 3–5% of patients.
Heitmann et al. revisited the latissimus dorsi muscle to provide a comprehensive synopsis of its anatomy. The neurovascular hilus was found on the deep surface of the latissimus dorsi muscle approximately 4 cm distal to the inferior scapular border and 2.5 cm lateral to the medial border of the latissimus muscle. At that point there was a constant bifurcation into a horizontal (medial or transverse) branch and a descending (lateral or vertical) branch, but there are interconnections between the horizontal and descending/lateral branches.
In more than 90% of cases, the thoracodorsal artery bifurcates into the medial and the slightly larger lateral branch. The lateral branch characteristically parallels the lateral border of the muscle, running approximately 2.5 cm from its edge. The upper or medial branch separates from it at an angle of about 45° and parallels the upper muscle border. Within the muscle, both branches divide into lesser branches, which run medially and anastomose with perforators from intercostals and lumbar arteries. A very significant feature of these anastomoses is their large diameter.
In the remaining cases, the neurovascular tree splits into three or four major branches. Both branching patterns supply the muscle with long, parallel neurovascular branches, which run in the fascia between bundles of muscle fibers and thereby enable the muscle to be split into independent vascularized innervated units.
Cutaneous perforator vessels could be traced to the thoracodorsal artery and had a caliber of >0.5 mm. They were always found in proximity to the horizontal or the lateral branch. All thoracodorsal cutaneous perforators originated within a distance of 8 cm distal to the neurovascular hilus.
The thoracodorsal artery supplies predominantly the latissimus dorsi muscle but also gives branches to the serratus anterior muscle, the axillary skin, and the subscapular and teres major muscles.
The thoracodorsal artery gives off 1–3 branches of about 1 mm diameter to the serratus anterior, which penetrate the muscle in its midportion along the course of the long thoracic nerve. Reversal of flow may take place in these vessels and also in vessels from teres major in the paratenon around the insertion and perhaps in other direct vessels entering from axillary and intercostal vessels.
The thoracodorsal artery also gives off a cutaneous branch in about 75% of cases, before it continues on to penetrate and supply the latissimus dorsi. The cutaneous branch arises between 0.5 and 2 cm beyond the bifurcation of the subscapular artery.
The subscapular artery arises in general, as a branch of the third portion of the axillary artery. Its average external diameter at its origin at the axillary artery is about 6 mm and its average length to the origin of the circumflex scapular artery is about 2.2 mm.
Usually the circumflex scapular artery (average length 4 cm, average diameter 4 mm) is found to be the first branch of the subscapular artery but in about 3% the circumflex scapular artery is a direct branch of the axillary artery.
The second major branch of the subscapular artery is the thoracodorsal artery.
perforating posterior branches of the posterior intercostal arteries
Length: 2 cm (range 1.5–2.5 cm)
Diameter: 1.5 mm (range 1–2.1 mm)
The 9th, 10th, and 11th intercostal vessels provide the three largest medial dorsal branches and have been the major vascular pedicles for the reverse latissimus dorsi musculocutaneous flap. In contrast, the lateral branches initially were only occasionally mentioned as a source of pedicled flaps, but later they were also used as donor vessels for the reverse latissimus dorsi flap. Because of their short pedicle, both the medial and lateral dorsal branches have been confined to their use as pedicled flaps. Even if the vascular pedicle is of sufficient length for a free flap, the difficult and harmful preparation of the vessels through the thick package of paraspinous muscles down to the source vessels is justified only exceptionally.
These vessels predominantly supply the distal part of the latissimus dorsi muscle. They are found in two rows as segmental vessels 5–10 cm from the dorsal midline. There are usually 4–5 vessels in each segmental row. The lateral row derives its blood supply from branches of the posterior intercostal artery and the medial row derives its blood supply from the lumbar artery.
Accompanying veins follow the arteries
thoracodorsal vein
Length: 9 cm (range 7.5–10 cm)
Diameter: 3.5 mm (range 2–5 mm)
Usually, the thoracodorsal vein originates from the subscapular vein. Anatomic variations in venous anatomy are present in 3–5%. Most often, the thoracodorsal vein is doubled or originates direct from the axillary vein.
In the majority of cases, the subscapular vein and artery usually arise adjacent to each other but in about 10% of cases, the axillary artery arises proximal to the subscapular vein. The length of the subscapular vein averages 2 cm, with an average diameter of 9 mm. The circumflex scapular vein can arise directly from the axillary vein; two veins are normally found, both with a diameter that allows microanastomosis.
concomitant veins, running with the perforating arterial vessels, provide secondary venous drainage
Length: 2 cm (range 1.5–2.5 cm)
Diameter: 2 mm (range 1.1–2.7 mm)
The venous drainage of the muscle parallels the arterial supply but the presence of venous valves has important implications for flap design. The lower and medial parts of the muscle preferentially drain through the intercostals and lumbar venous system and not via the thoracodorsal system. Valves within the vein ensure this direction of flow. Also, the circumflex scapular vein can provide secondary drainage of the flap. In cases where a pedicled latissimus flap is performed based on retrograde flow from the circumflex scapular artery, the vein can provide adequate drainage to the flap.
In the arteries, reversal of flow can easily take place and blood can reach the extreme parts of the muscle; on the venous side there are problems in draining the inferior end of the muscle into the thoracodorsal system. The result is that the muscle-only flap suffers venous compromise in its lower part, and any areas that appear suspect after reperfusing a free flap should be excised, as experience has shown that these areas, which initially have an arterial inflow but which ooze dark deoxygenated blood, do not survive. By contrast, the musculocutaneous flap fares better in its distal part, perhaps because venous blood from the muscle can find an additional pathway of return through the subcutaneous venous network.
the posterior branches of the lateral cutaneous branches of the intercostal nerves provide cutaneous sensibility laterally, and lateral branches of the posterior rami (VI through XII) posteriorly.
Usually these branches are not used to reinnervate the flap, but in the special case when a reverse pedicled flap is performed based on the posterior intercostal vessels, its sensory innervation can be preserved and so the sensory innervation can be maintained.
the thoracodorsal nerve arises from the posterior cord of the brachial plexus and travels latero-inferiorly behind the axillary artery and vein.
The thoracodorsal nerve is usually located 3 cm medial to the origin of the subscapular artery in the axilla. It accompanies the vascular pedicle more closely, approaching the entrance of the neurovascular bundle, and it is sometimes difficult to preserve the nerve during elevation of the flap. Even if only a small portion of muscle is included, the entire muscle is denervated. The nerve divides into lateral and medial branches approximately 1.3 cm proximal to the neurovascular hilus and each branch runs with its vascular counterpart.
Some authors have described an intramuscular dissection of the nerve that allows for its preservation. Thus, if the intention is to split the muscle and retain half of it on the chest with an intact nerve supply, then the dissection is more complicated. The vascular basis for splitting the flap is the known bifurcation of the thoracodorsal artery within the muscle, which enables either the superior horizontal part of the muscle or the anterior vertical part to be harvested on the thoracodorsal pedicle. In this situation, the part of the muscle left on the chest is detached from the thoracodorsal pedicle and receives its blood supply from the intercostal perforators. If this part of the muscle is left in continuity with the tendon of insertion and its innervation is preserved, then some function should be retained in it. The bifurcation of the thoracodorsal artery is, on average, 8.7 cm from the point where the subscapular artery arises from the axillary artery.
Proprioceptive nerve fibers accompany motor fascicles of the thoracodorsal nerve. This may be the reason why some studies report deep sensation of a transferred latissimus dorsi flap up to 18 months after coaptation of the thoracodorsal nerve to a sensory recipient nerve.
The latissimus dorsi flap can be raised as a muscle, or a musculocutaneous, an osteomusculocutaneous, or even a perforator flap (TDAP) (see Ch. 56 ). The skin is nourished via the fascia and the perforator vessels, which therefore must be taken with the muscle in musculocutaneous flaps.
Combinations and extensions are possible with any component from the subscapular system (i.e., bone, skin, fascia, muscle). On the same pedicle, it can be elevated with the serratus fascia or the serratus muscle, the accompanying rib or part of the scapula, or with a scapular or parascapular flap. In this way it is possible to harvest multicomponent flaps to simultaneously reconstruct complex defects with several flaps based on a single pedicle.
Latissimus dorsi dissection is rapid, easy, and safe because of the reliable anatomy of the thoracodorsal and subscapular vessels.
Microvascular transfer is facilitated by the long pedicle and large caliber of the vessels. The robust viability of this large muscle flap constitutes its major commending feature.
A skin island can be orientated vertically, obliquely, or transversely as desired or required by the defect.
The latissimus dorsi flap, one of the largest flaps in the body. It can be tailored to almost any size and shape. The flap can extend from the axilla to almost the iliac crest. Elevating the latissimus dorsi flap so far distal will result in an extremely long vascular pedicle, making the flap especially suitable for large skin defects or anastomotic sites remote from the defect.
As a pedicled flap, it is certainly one of the most versatile flaps for reconstructive problems of the chest wall and the upper arm. The pedicled muscle flap alone will also supply coverage for massive defects of the head and neck area as well as the shoulder.
Where large areas of a thinner flap coverage are required, the muscle alone can be transferred microsurgically and then skin grafted to avoid excessive bulk at the recipient area, and to avoid a large secondary skin defect in the donor area.
The musculocutaneous latissimus flap may be advantageous in providing bulk for the correction of contour defects.
Numerous combinations are possible. Combined (“chimeric”) flaps with other components from the subscapular system can be designed, vascularized bone can be harvested as rib grafts with the latissimus, or on a common pedicle from the scapula, fascia can be added from the serratus muscle.
The thoracodorsal nerve can be included so that the muscle can be reinnervated for restoration of motor function.
If the latissimus dorsi flap is harvested correctly, several flaps such as the scapular flap or the serratus muscle/fascia flap are still possible, although with smaller vessel diameters.
Overall, the usefulness of this remarkable flap far outweighs its recognized disadvantages.
This flap, especially the musculocutaneous type, is generally bulky, depending on the general physical constitution of the patient. Exact intramuscular dissection with tailoring of the flap to the defect size can significantly decrease the amount of muscle harvested. Even though the muscle atrophies to some degree, skin islands in musculocutaneous flaps are usually also bulky and require secondary thinning and contour correction for satisfactory aesthetic results.
Surprisingly, the functional deficit of shoulder and arm function from loss of the latissimus dorsi muscle is estimated to average approximately 7% in most individuals. If all the other muscles of the shoulder girdle are intact, the loss of the latissimus dorsi muscular function is rarely noticeable in normal activities. Occasionally, the harvest of this muscle will result in some winging of the scapula, even though the serratus anterior muscle is intact. It can also compromise the motion of “posterior push,” an important function in skiing, where the hand is pulling the body weight forward. Loss of the latissimus in paraplegics may also seriously weaken upper extremity function such as crutch-walking or bed-to-wheelchair transfer. Similarly, in patients with poliomyelitis or other neuromuscular diseases, loss of the latissimus dorsi muscle may seriously weaken pelvic stability.
Other disadvantages are directly related to donor site complications. Pains at the donor site and seroma formations are occasionally seen. Most of these symptoms disappear over time, and persistent complaints are rare.
No preoperative vessel identification is necessary. In cases of previous axilla dissection or radiation, muscle function has to be evaluated preoperatively. If muscle function is intact, the vessels are likely not violated. If the muscle function does not seem to be good or if the suspicion is high for vessel injury, further studies such as tracing the vessel course with high resolution ultrasound may be performed to see if adequate perfusion is available, and if the muscle is viable and can be used for wound coverage.
A donor site for possible skin grafting is also prepped and draped. Preoperative antibiotics are not given routinely and the decision is based on the recipient site and the condition of the patient.
The margins of the latissimus dorsi muscle extend from the tip of the scapula to the midline of the back posteriorly and with its fascial extension to the iliac crest inferiorly. The anterior border of the muscle passes on an oblique line from the mid-point of the iliac crest to the axilla. This prominent border forms the posterior axillary fold, together with the subscapular and the teres major muscles.
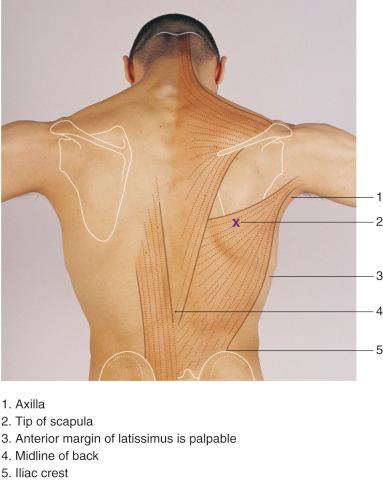
The design of the latissimus dorsi flap can be varied according to the requirements for skin or muscle. Therefore the location and proportion of the skin island must be exactly determined during preoperative planning. If more skin than muscle is needed, then the skin island should be based toward the anterior edge of the muscle, where perforating vessels can be found, which also form the base of the TDAP (thoraco-dorsal artery perforator flap).
Several areas of skin can be raised separately on the same muscle flap, so that many reconstruction possibilities are available. The anterior edge of the muscle should always be included because the greatest number of perforating vessels supplying the skin is found there.
For breast reconstruction, the island over the upper free muscle border should be designed in a way that closure of the secondary defect leaves a transverse scar that is easily concealed by a brassiere.
For head and neck reconstruction, if the flap is to be pedicled, a skin island along the anterolateral margin of the muscle is necessary because the transverse island will not reach. Elevation of a muscle flap may be done through either incision.
When raising the flap with bone from the scapula, there are variations in the anatomy to be considered. The general scheme is shown with the angular branch supplying the lower pole of the scapula and the circumflex scapular artery the middle and upper thirds of the lateral border. The angular branch arises directly from the thoracodorsal artery just proximal to the origin of the branch of serratus.
In a small percentage of patients, the latissimus muscle may play a significant role in raising the pelvis while walking. In patients with spinal cord injuries affecting this area, the dimensions and thickness of the muscle may be quite small.
The latissimus dorsi muscle can be carried on the highest branch of the circumflex scapular artery, even if the thoracodorsal artery is sacrificed. This smaller vessel usually provides a reliable blood supply for the muscle with the exception of the most distal aspects.
In planning the pedicled flap, Chandra uses the horizontal continuation of a line drawn through the nipples (with the arm by the side) to surface mark the base of the flap. The long axis of the flap then has its center line 1 cm anterior and parallel to the edge of the latissimus dorsi. The largest flap described by Chandra was 7 × 20 cm and all donor sites were capable of direct closure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here