Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Laser trabeculoplasty: laser treatment to the trabecular meshwork to enhance outflow of aqueous humor from the eye.
Laser peripheral iridectomy: laser treatment to create a full-thickness hole within the peripheral iris to alleviate pupillary block.
Typically performed with argon or a frequency-doubled neodymium:yttrium–aluminum–garnet (Nd:YAG) laser.
Indicated for ocular hypertension, primary open angle, pigmentary, pseudoexfoliation, and select other open-angle glaucomas.
Immediate pressure spike can occur.
May lose its effect chronically.
Typically done with Nd:YAG and/or argon laser.
Alleviates pupillary block angle-closure mechanism.
Hemorrhage, uveitis, and lens damage can occur.
The notion of anterior chamber angle photocoagulation, using a xenon arc light source, was introduced by Zweng and Flocks in 1961. Laser treatment of the human trabecular meshwork (TM) by puncturing Schlemm’s canal was performed initially by Krasnovin 1972, but the lower intraocular pressure (IOP) he described was short-lived. Ticho and Zauberman noted that argon laser treatment of the angle was successful in lowering IOP despite lack of permanent trabecular openings. Contemporary use of argon laser trabeculoplasty (ALT) is based on a report demonstrating safety and efficacy in a group of patients with open-angle glaucoma in 1979 by Wise and Witter. In 1998, Latina and colleagues used a frequency-doubled neodymium:yttrium–aluminum–garnet (Nd:YAG) nonthermal laser to lower IOP successfully in patients with open-angle glaucoma. This laser appears to selectively target pigmented cells with little or no damage to the surrounding structures, and hence is referred to as selective laser trabeculoplasty (SLT). ALT and SLT are equally safe and effective in lowering IOP in open-angle glaucoma. The mechanisms of action of ALT and SLT remain to be completely elucidated. With ALT, there appears to be a mechanical effect (one or more of tightening of the TM, opening intervening spaces, or opening a collapsed Schlemm’s canal) and/or a biological response (cytokines are released that change the extracellular matrix of the TM, open junctions between Schlemm’s canal endothelial cells, recruit macrophages and monocytes, and increase phagocytic activity of the TM). With SLT a cellular or biological mechanism is like ALT, without any obvious thermal/mechanical effects.
Micropulse laser trabeculoplasty uses repetitive microsecond pulses with frequent periodic pauses, thereby decreasing coagulative damage by allowing intermittent cooling periods from consistent thermal energy. IOP lowering is likely related to cytokine release, resulting in increased outflow. Studies have revealed a significant IOP reduction in patients with uncontrolled open-angle glaucoma with minimal complications.
Newer laser treatment modalities, such as Titanium Sapphire laser trabeculoplasty, have also shown early promising IOP reductions with minimal complications. More studies are needed to determine treatment safety and efficacy of the above lasers; this chapter therefore focuses on ALT and SLT.
The main indications for laser trabeculoplasty are summarized in the table below:
| Main Indications for Laser Trabeculoplasty | Relative Contraindications/Ineffective in |
|
|
|
|
|
|
|
|
|
|
Predictors for ALT success are shown in Table 10.23.1 . With optimal patient selection, after ALT, IOP typically declines 25%–30% below the initial IOP at 1 year (the effect fades with time at an attrition rate of about 10% per year). SLT offers a safe and effective IOP-lowering alternative to ALT in patients with open-angle glaucoma ( Table 10.23.2 ).
| Negative Predictors | Positive Predictors | |
|---|---|---|
| Age (y) | <40 | >65 |
| Trabecular meshwork pigmentation | Little or none | Moderate to marked |
| Corneal clarity | Poor | Clear |
| Disease entities |
|
|
| Lens status | Aphakic or anterior chamber intraocular pseudophakia | Phakic or posterior chamber intraocular pseudophakia |
| Contralateral eye | Little effect | Strong effect |
| Mean Intraocular Pressure at Various Time Points to 1 Year | |||
|---|---|---|---|
| ALT (SD) | SLT (SD) | P Value | |
| Baseline | 23.48 (4.21) ( n ≡ 87) | 23.84 (4.88) ( n ≡ 89) | 0.60 |
| 3 months | 19.75 (4.79) ( n ≡ 73) | 18.89 (4.71) ( n ≡ 76) | 0.31 |
| 6 months | 18.42 (4.20) ( n ≡ 79) | 17.83 (4.33) ( n ≡ 79) | 0.40 |
| 12 months | 17.88 (3.92) ( n ≡ 74) | 17.97 (4.74) ( n ≡ 73) | 0.90 |
IOP decline with SLT depends on baseline IOP but seems independent of TM pigmentation. Caution needs to be exercised, however, in patients with heavy degrees of meshwork pigmentation, because these patients are at higher risk for a sustained, irreversible IOP spike.
A 360° treatment with ALT or SLT appears to be more effective than 180° or 90°, but there is a higher risk of postoperative IOP spike. Studies suggest that both ALT and SLT could be offered as first-line therapy in patients with ocular hypertension and open-angle glaucoma. In the Glaucoma Laser Trial the authors concluded that initial ALT is at least as effective as initial treatment with topical medication (typically a beta-blocker). The LiGHT study, a randomized controlled trial in treatment-naive patients with open-angle glaucoma or ocular hypertension, randomized patients to initial SLT or to eye drops (typically a prostaglandin analogue). The study showed no significant difference between groups in the health-related quality of life at 3 years. In addition, patients treated with SLT were within target IOP at more visits versus initial medication use (93% vs. 91.3%), required less surgery, and 74.2% of patients in the SLT group required no drops to maintain IOP at target.
One study by Hong et al. suggested repeating SLT once may be effective, but not as effective as initial treatment. The SLT LiGHT study, through a post-hoc analysis, also supports the effectiveness of repeat treatment. However, much more work needs to be done in this area.
Following 360° of SLT, a comparison of repeat laser with SLT versus ALT at 12 months demonstrated that both lasers reduced the IOP approximately 3 mm Hg; however, the time-to-failure analysis favored SLT over ALT. Another study showed that 180° SLT has a greater effect of decreasing the usage of medication than ALT.
A drop of apraclonidine (0.5%) or brimonidine (0.15% or 0.2%) is instilled in the eye 30–60 minutes preoperatively to minimize IOP elevation after treatment.
If the angle is closed or narrow, a peripheral iridectomy or laser iridoplasty can be performed beforehand to deepen and allow better visualization of the angle.
A Ritch or a three-mirror Goldmann lens with antireflective coating is used. The lens does not invert the image but reverses the position, such that the 12 o’clock position of the mirror represents the 6 o’clock position at the angle, the 1 o’clock position of the mirror represents the 5 o’clock position at the angle, and so forth.
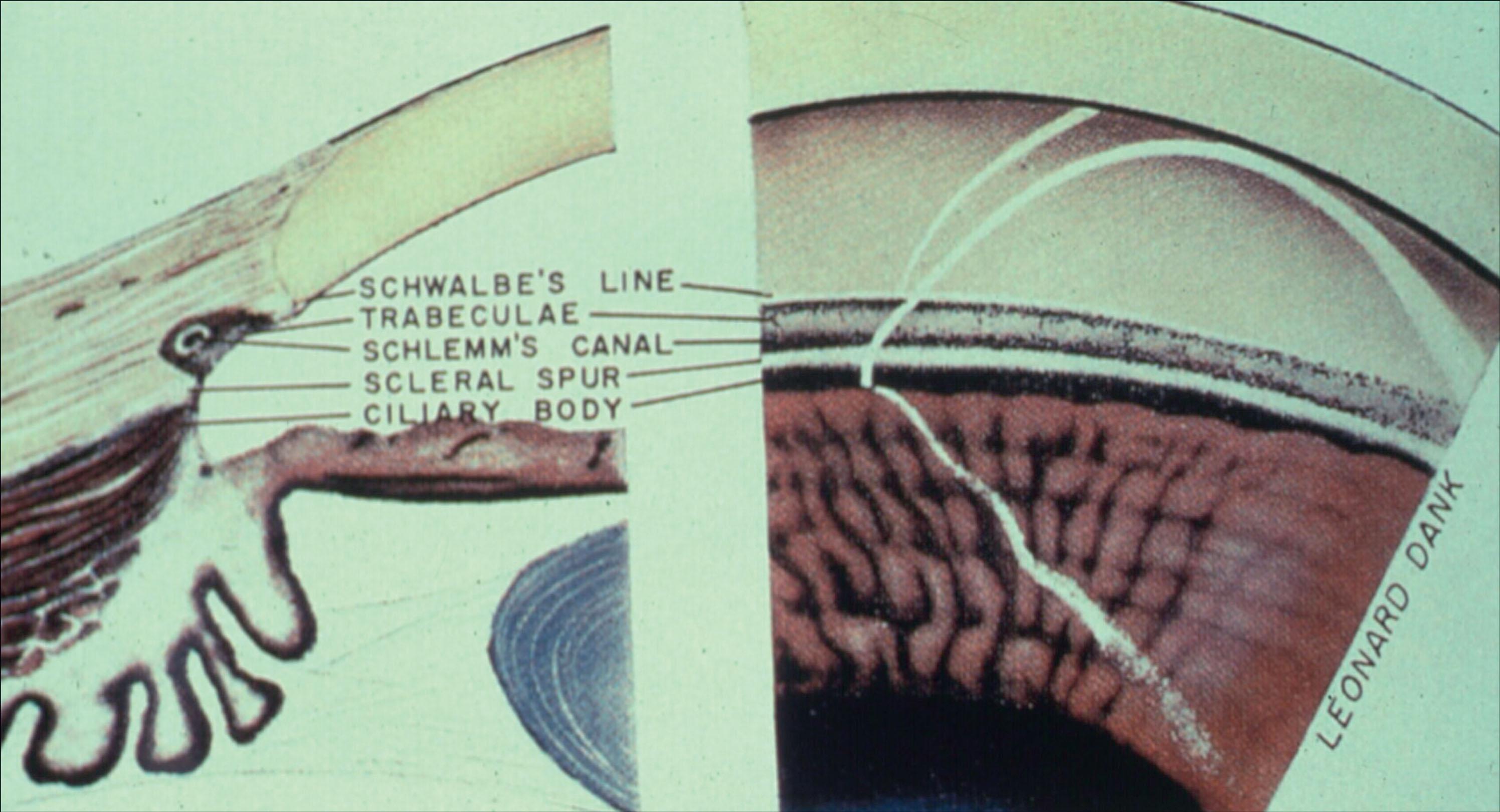
The TM may occasionally be variably pigmented, and a pigmented Schwalbe’s line or a ciliary body band may be confused with the TM. In this case the corneal wedge reflex can help to locate Schwalbe’s line ( Fig. 10.23.1 ).
Topical anesthetic is instilled immediately before the procedure. The goniolens is applied using methylcellulose as the coupling agent. The procedure begins with the goniolens at the 12-o'clock position (to visualize the inferior angle that is the deepest part of the angle), and the lens is typically rotated clockwise. To ensure delivery of laser energy with maximal efficiency, the aiming beam is always kept in the center of the mirror, round and sharp, keeping the goniolens perpendicular to the laser beam. The lens is rotated after several applications.
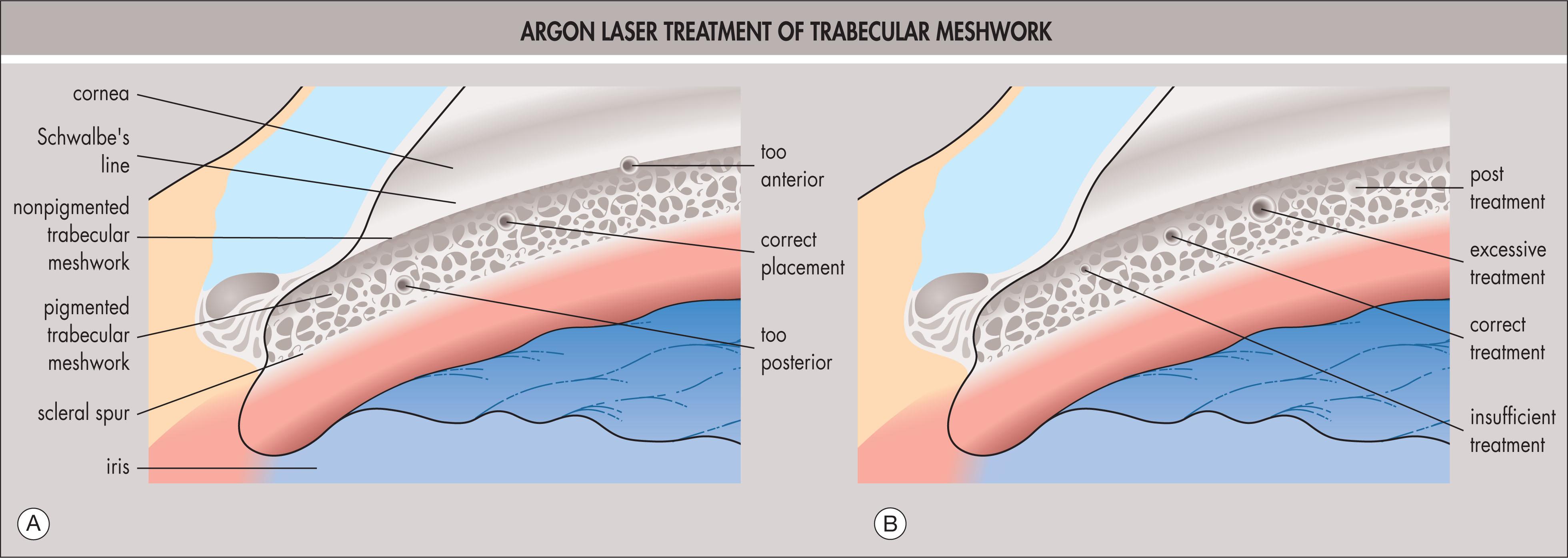
The laser spots for ALT are placed at the junction of the posterior pigmented and anterior nonpigmented TM, with a gap of about the diameter of one to two laser spots between spots ( Fig. 10.23.2A ). We currently treat 180° of the inferior angle in one session (it is generally best to treat the same portion of the angle first to avoid future confusion on completion of the remaining 180°). See Table 10.23.3 for recommended treatment guidelines.
| ALT | SLT | MLT | Peripheral Iridectomy | Argon Laser Iridoplasty | |||
|---|---|---|---|---|---|---|---|
| Argon | Yttrium–Aluminum–Garnet | ||||||
| Light Irides | Dark Irides | ||||||
| Spot size (μM) | 50 | 400 | 300 | 50 | 50 | Fixed | 200–500 |
| Spot duration | 0.1 s | 0.3 ns | 0.3 s | 0.2 s | 0.02–0.05 s | Fixed (ns) | 0.2–0.5 s |
| Power | 200–800 mW | 0.4–1.2 mJ | 1000 mW | 1000 mW | 1000 mW | 3–8 mJ | 200–400 mW |
| Number of spots | 50 per 180° | 50 per 180° | 50–60 per 180° | 15–25 | 25–100 | 1–5 (each burst consists of 1–3 pulses) | 4–6 per quadrant, typically treat 360° |
Settings should be adjusted according to the tissue reaction endpoint, which is minimal blanching (see Fig. 10.23.2B ). If the burn is too anterior, the treatment is more likely to be ineffective; if it is too posterior, it is more likely to create inflammation and peripheral anterior synechiae.
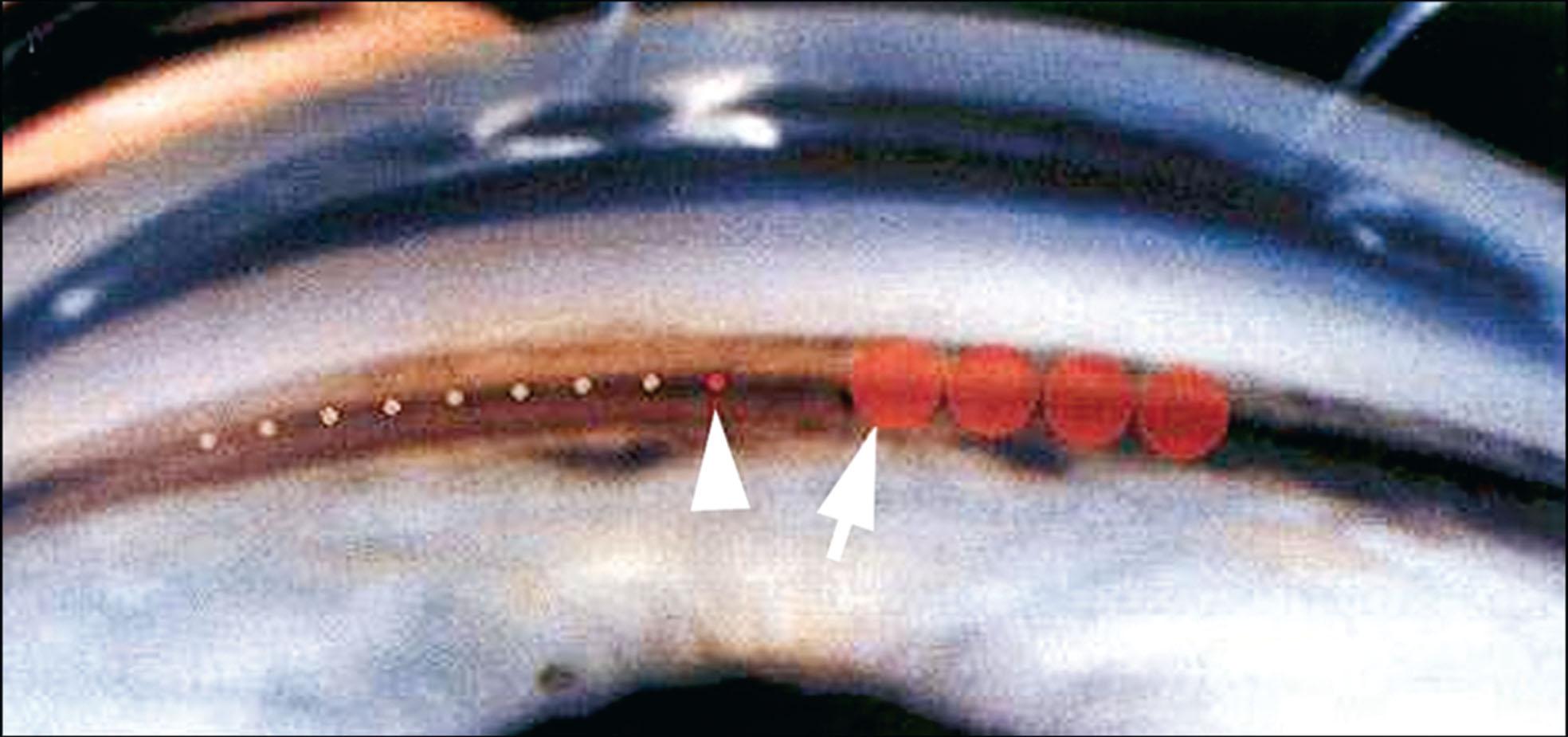
SLT has a relatively large, 400-μm fixed spot size, which ideally should be centered on the TM. The energy is adjusted from 0.8 mJ downward or upward, depending on the tissue response. For SLT, occasional creation of bubbles is a reasonable endpoint. The number of spots applied is approximately 50 over 180°, with 180°–360° treated initially (if treating 360° then 90–100 spots are applied). The spots are almost confluent and span the entire angle width because of the large spot size ( Fig. 10.23.3 ). Preoperative and postoperative care are similar to that of ALT.
The IOP is measured 1 hour after laser trabeculoplasty. If it is elevated, additional IOP-lowering medication is administered, and the IOP is rechecked 30–60 minutes later. Topical prednisolone acetate 1% or a topical nonsteroidal antiinflammatory drug (NSAID) four times daily is prescribed for 4–7 days, and as long as the 1-hour IOP was similar to or lower than baseline, the patient can be seen 4–6 weeks later. In eyes that were treated with corticosteroid or NSAID drops after SLT, significantly better IOP reduction at 12 weeks was measured. Short-term postoperative use of NSAID or corticosteroid drops may improve IOP reduction after SLT. Longer-term follow-up studies are indicated. The postoperative antiinflammatory drops may improve the IOP outcome. If there is a concern about IOP or inflammation, the patient can be reviewed after 1 week. If anterior uveitis is present at 1 week, topical corticosteroids are continued.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here