Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Trauma to the larynx accounts for less than 1% of all trauma. This is explained in part by the fact that the larynx is relatively protected by the mandible, sternum, and flexion mechanism of the neck. An alternative perspective is the percentage of patients with laryngeal injuries who are dead on arrival at the emergency department. Line and associates reported a series of 171 victims of blunt neck trauma (strangulation), of whom 112 persons (65%) did not survive. It has been estimated that the emergency departments in busy trauma centers will treat one patient with laryngeal trauma for every 5000 to 30,000 emergency department visits.
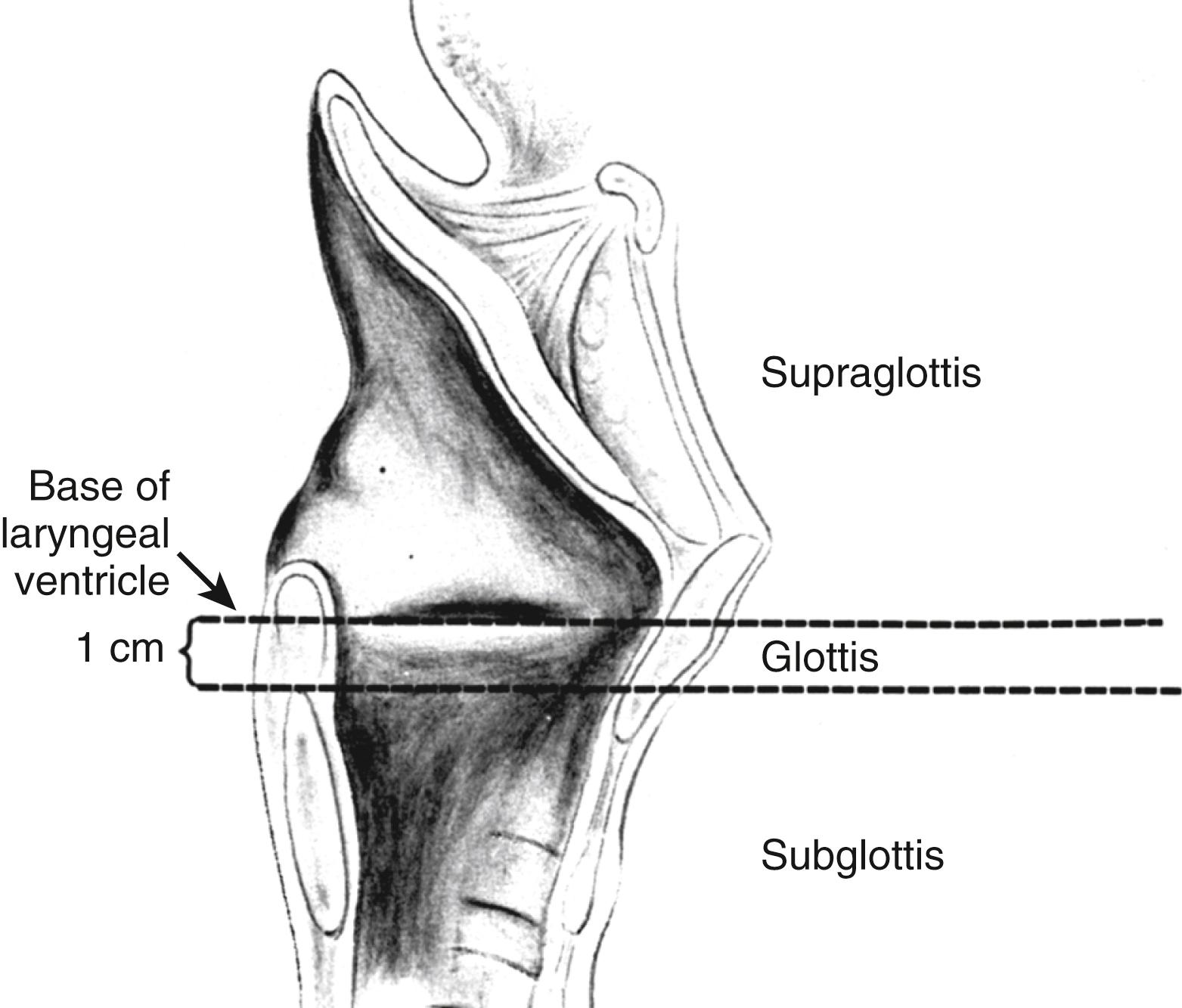
A basic knowledge of the laryngeal anatomy and physiology is fundamental to understanding the principles established for the management of laryngeal trauma. The larynx is classically divided into three anatomic areas with different functions and characteristics ( Fig. 8.1 ). The primary functions of the larynx are to serve as an airway conduit and to protect the lower respiratory tract. The production of voice, although extremely important for socioeconomic development, is of teleological secondary importance. Respiratory epithelium that is part of the mucociliary clearing system of the respiratory tract lines most of the larynx. The sensory innervation of the supraglottic larynx is supplied by the paired superior laryngeal nerves, which are also branches of the vagus nerves. The superior laryngeal nerves also innervate the cricothyroid muscle, which tightens the vocal folds and, accordingly, is responsible for pitch. The function of the larynx depends on a complex arrangement of intrinsic muscles innervated by the superior and recurrent laryngeal nerves, which are branches of the right and left vagus nerves. A framework composed of cartilage and ligaments supports the laryngeal soft tissue. The cartilaginous framework of the larynx relies on the blood supply provided by the perichondrium. This framework is then suspended on a sling between the mandible (via the hyoid bone) and sternum.
Trauma to the larynx may manifest in a wide variety of ways, reflecting a multitude of uncontrollable variables. Accordingly, evaluation and management of the patient with laryngeal trauma requires accurate assessment, a working understanding of the principles of laryngeal reconstruction, and an ability to accommodate unexpected findings at exploration in the operating room.
Children rarely suffer direct trauma to the larynx. This reflects the morphologic differences between children and adults. The larynx in children is relatively protected since it is high in the neck and generally shielded from direct trauma by the mandible. In addition, the soft, flexible cartilaginous structures of the pediatric laryngotracheal complex are more tolerant of blunt trauma.
The mechanism of trauma greatly influences the likelihood for associated injury and the need for multidisciplinary collaboration. In general, laryngeal trauma is classified as blunt or penetrating . The most common mechanism of injury is blunt trauma. With a patient injured in a motor vehicle accident, a broad general assessment of the patient’s overall well-being is clearly mandated.
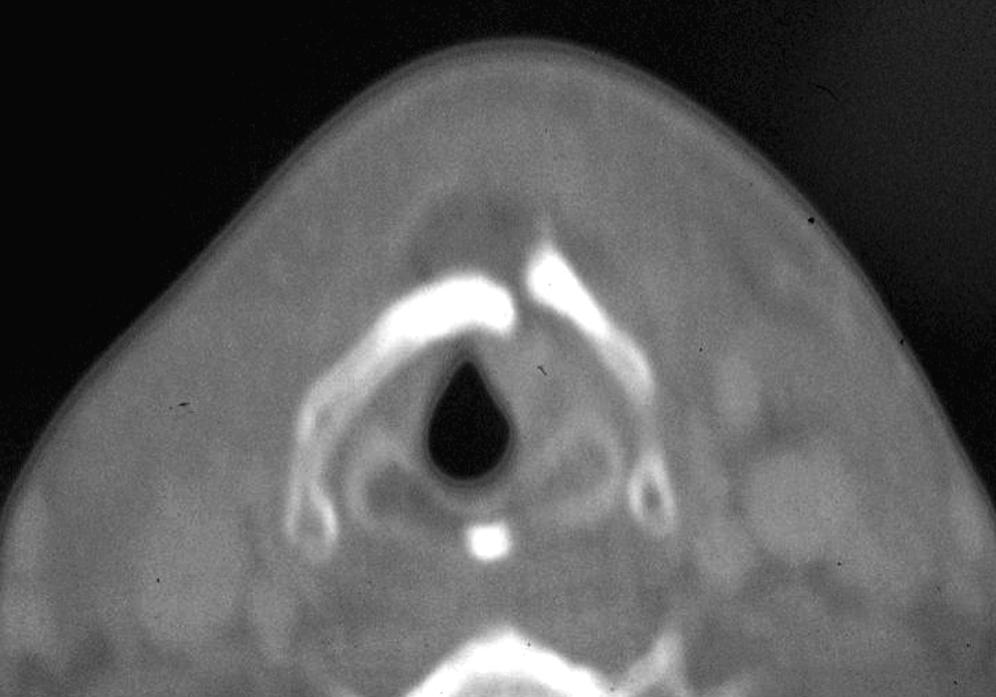
Blunt trauma to the cervical region may produce serious and life-threatening injury, including total obstruction of the airway and significant life-threatening vascular disruption ( Fig. 8.2 ). Cervical spine injuries occur in a significant percentage of patients and may not be appreciated initially because of the obvious soft tissue damage. Injuries to major structures are more clearly apparent when a sharp instrument or penetrating missile results in soft tissue wounds. Nevertheless, injury may be significant even with minimal signs of external wounds. Any type of blunt trauma may disrupt the laryngeal soft tissue or its cartilaginous framework, producing scarring, loss of support, and subsequent collapse of the airway and stricture. It may also dislocate the cricoarytenoid joint, leading to fixation of the vocal cord, or disrupt the laryngeal innervation, paralyzing the vocal cords. It is important to realize that significant laryngeal trauma may be possible in the absence of signs of external injury.
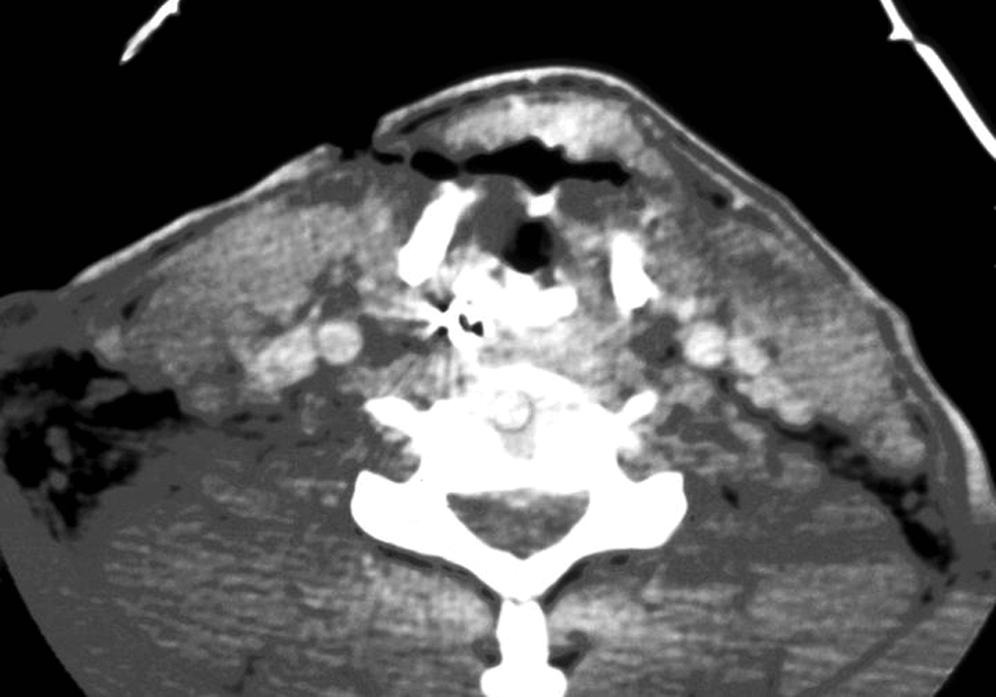
The larynx may also be involved in penetrating trauma to the neck. It is important to recognize that approximately 60% of the patients with penetrating trauma to the larynx will have other associated injuries, such as neurologic vascular or esophageal injuries. Penetrating trauma includes a wide range of injuries, ranging from stab wounds to gunshot wounds. Although stab wounds usually follow a straight line or predictable path, bullets or other projectiles tend to follow planes of least resistance (e.g., fascial planes), producing less predictable injuries. Bullets cause injury both by direct contact as well as tissue distention caused by the abrupt displacement of the tissues produced by the bullet’s shock wave ( Fig. 8.3 ). The trauma caused by this shock wave increases as the square of the velocity, hence high-velocity weapons such as assault rifles cause much greater injury.
A peculiar injury is one produced by strangulation, which is a broad term that includes hanging, garroting (ligature strangulation), throttling (manual compression), and chokeholds. Strangulation accounts for 10% of the violent deaths in the United States. Victims of strangulation most often die at the site of the incident, accounting for its infrequency as an emergency department visit. Strangulation is characterized by the application of a static force over the laryngeal framework, which may fracture the cartilage and not disrupt the mucosa. This latter fact frequently leads the examiner to the false assumption that the victim has not suffered a significant injury. The classic injury in strangulation victims is a fracture of the superior thyroid cornu, which may be accompanied by cordal hematomas, petechiae of the endolaryngeal mucosa, or arytenoid dislocation. A history of significant bleeding that has spontaneously resolved or a hematoma that developed rapidly suggests a major vascular injury that will require evaluation. The Isadora Duncan syndrome consists of strangulation with carotid contusion, avulsion, or occlusion and laryngeal rupture.
The glottis depends on cartilaginous support, mobility of the cricoarytenoid joint, and perfect neuromuscular coordination to perform its sphincteric and voice-producing functions.
The adult airway is narrowest at the glottic level; therefore any decrease in the cross-sectional area of the airway at the level of the vocal cords may result in significant compromise of the airway (proportional to the square of the radius).
The subglottis is supported by the cricoid cartilage, which is the only circular cartilage of the laryngotracheal complex.
Penetrating laryngeal trauma requires endoscopic evaluation and repair of disrupted epithelium and cartilage.
Voice change following blunt cervical trauma mandates evaluation of the laryngeal anatomy.
All patients with significant laryngeal trauma should be considered at risk for an injury to the cervical spine.
Penetrating airway trauma may be associated with significant neurovascular injury.
Tracheostomy (or cricothyrotomy) may be required when laryngeal trauma results in stridor or cyanosis.
Displaced fractures of the thyroid and cricoid cartilage require early reduction to improve long-term results.
Keels and stents may facilitate epithelial regrowth and prevent scarring after major disruption of the laryngeal structures.
Keels are preferred to stenting. If stenting is required for support, minimize the length of time the stent is in place to prevent scarring.
Tracheostomy tubes must be secured in the presence of severe laryngeal trauma.
Airway evaluation (often with flexible laryngoscopy) in the patient who is suspect for laryngeal trauma is vital prior to “elective” radiologic evaluations.
When possible, awake transnasal flexible laryngoscopy is a vital tool in the evaluation of the injury.
Lacerations of the cervical esophagus or pharynx may occur, primarily with penetrating injuries, and need to be ruled out. Failure to recognize and treat them can lead to serious infectious complications. Depending on the circumstances, evaluation with either contrast radiographic studies or endoscopy is appropriate.
The nature of the trauma is pivotal to assessment of laryngeal trauma.
When evaluating patients with penetrating trauma, it is important to know the circumstances of the attack: factors such as angle of penetration, types of bullet and weapon, and distance of attack are all important to estimate the degree of trauma.
Factors that may significantly affect subsequent patient care include patient age, mechanism of injury, velocity of injury, and cutaneous penetration.
The integrity of the airway must be initially assessed. Cyanosis and stridor are indications for immediate intervention. Intubation of the acutely traumatized airway may be dangerous or impossible. Tracheostomy or, under some circumstances, cricothyrotomy should be initiated.
When the status of the cervical spine is either suspect or uncertain, manipulation of the neck and positioning of the patient for tracheostomy may be difficult and imprudent.
Under extreme circumstances, insertion of a large-bore needle directly through the cricothyroid membrane or into the trachea with administration of oxygen may be lifesaving and “buy time” for definitive airway intervention.
Patients with laryngeal trauma almost invariably have primarily inspiratory obstruction owing to collapse of the soft tissues during inspiration.
Oxygen delivered directly into the trachea may be expired through the injured larynx in most patients.
Concurrent intrathoracic injury, including pneumothorax, fractured ribs with a flail chest, or a pulmonary contusion, may be the cause of respiratory distress and must be ruled out.
The principles (airway, breathing, circulation) of trauma care must be recalled and be kept primal.
Even with trauma limited to the head and neck, the integrity of the cardiovascular system, potential for intracranial injury, and status of the cervical spine must always be assessed as an initial step of management.
Airway assessment
Cranial nerve assessment
Flexible laryngoscopy, when possible, is a vital aspect of the physical examination to assess airway patency, mucosal integrity, and vocal fold motion.
Dysphonia, hoarseness, dysphagia, or odynophagia in the setting of blunt trauma to the neck must be considered evidence of severe laryngeal injury until proven otherwise.
The patient suspected of having trauma of the larynx must have an airway assessment (ideally, flexible laryngoscopy) prior to being sent out of the emergency department for radiologic testing.
The finding of cervical subcutaneous emphysema warrants a presumptive diagnosis of a ruptured viscus. It is incumbent on the emergency team to identify the injured area and make plans for subsequent management.
The potential for injury to cranial nerves must be considered.
Neuropathy in the face of a sharp or penetrating injury is an indication for nerve exploration and neurorrhaphy as needed at the time of surgical exploration.
Neurorrhaphy may result in synkinesis, but some authors have reported useful return of motion or at least tone.
The potential for vascular injury must be considered. An expanding hematoma or continuing hemorrhage from an open wound is an indication for immediate operative exploration.
The presence of a bruit may be one indication of such an injury. The value of close collaboration with a vascular surgery team is critical.
When circumstances permit, a careful physical examination followed by directed imaging studies will facilitate subsequent treatment planning and intervention.
In one study of patients with laryngotracheal injury, the most prevalent findings on physical examination were subcutaneous emphysema (53%), hoarseness (47%), neck tenderness (27%), and stridor (20%).
Physical examination should include assessment of the airway and voice.
Dysphonia or hoarseness suggests laryngeal injury.
The soft tissues of the neck should be carefully observed and palpated.
The loss of the prominent contours of the thyroid cartilage and cricoid ring may be significant observations.
Point tenderness should lead to suspicion of a fracture.
Soft tissue abrasion and ecchymosis help confirm the severity and direction of injury.
The presence of a mass often indicates vascular injury.
Soft tissue emphysema indicates perforation of an air-containing viscus.
Examination of the oral cavity and oropharynx should be supplemented by direct visualization of the larynx and hypopharynx. This can be undertaken with either a rigid telescope or flexible laryngoscopy. The observer should note soft tissue disruption, lacerations, edema, or ecchymosis.
Patency of the airway and vocal fold function should be ascertained.
Shortening of the anteroposterior diameter of the glottis is an indication of fracture and subluxation of the thyroid cartilage.
The arytenoid cartilage may be dislocated.
Traumatic separation of the larynx from the trachea can occur even in blunt injuries and is frequently associated with bilateral vocal cord paralysis.
The airway must be secure. Flexible laryngoscopy must be done prior to any imaging.
Cervical spine imaging is primal for most patients suspected of potential laryngeal trauma.
Angiography or computed tomography (CT) angiogram should be done when vascular injury is suspected.
Fine-cut CT scan of the larynx with contrast (coronal and axial) ( Figs. 8.4 to 8.6 )

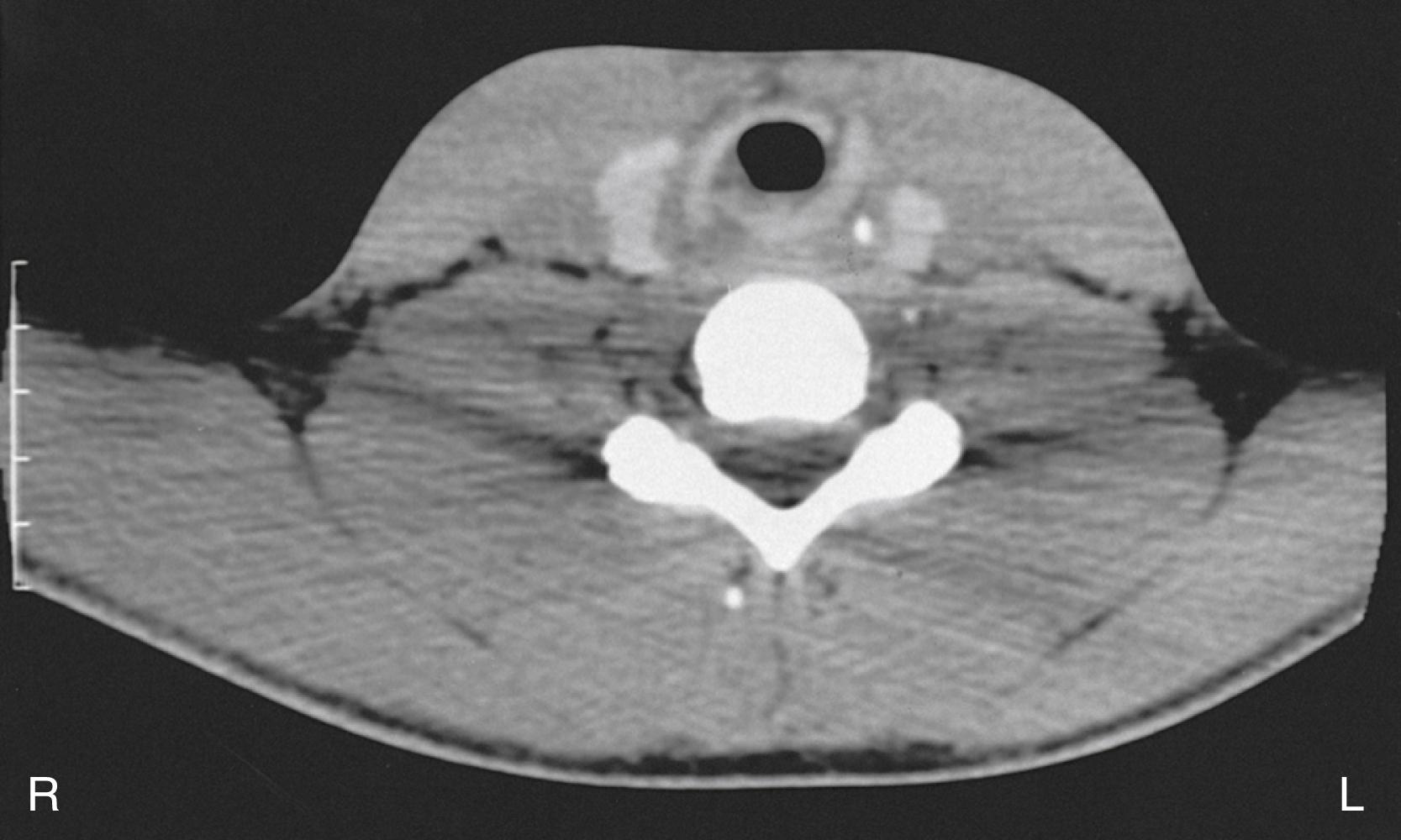
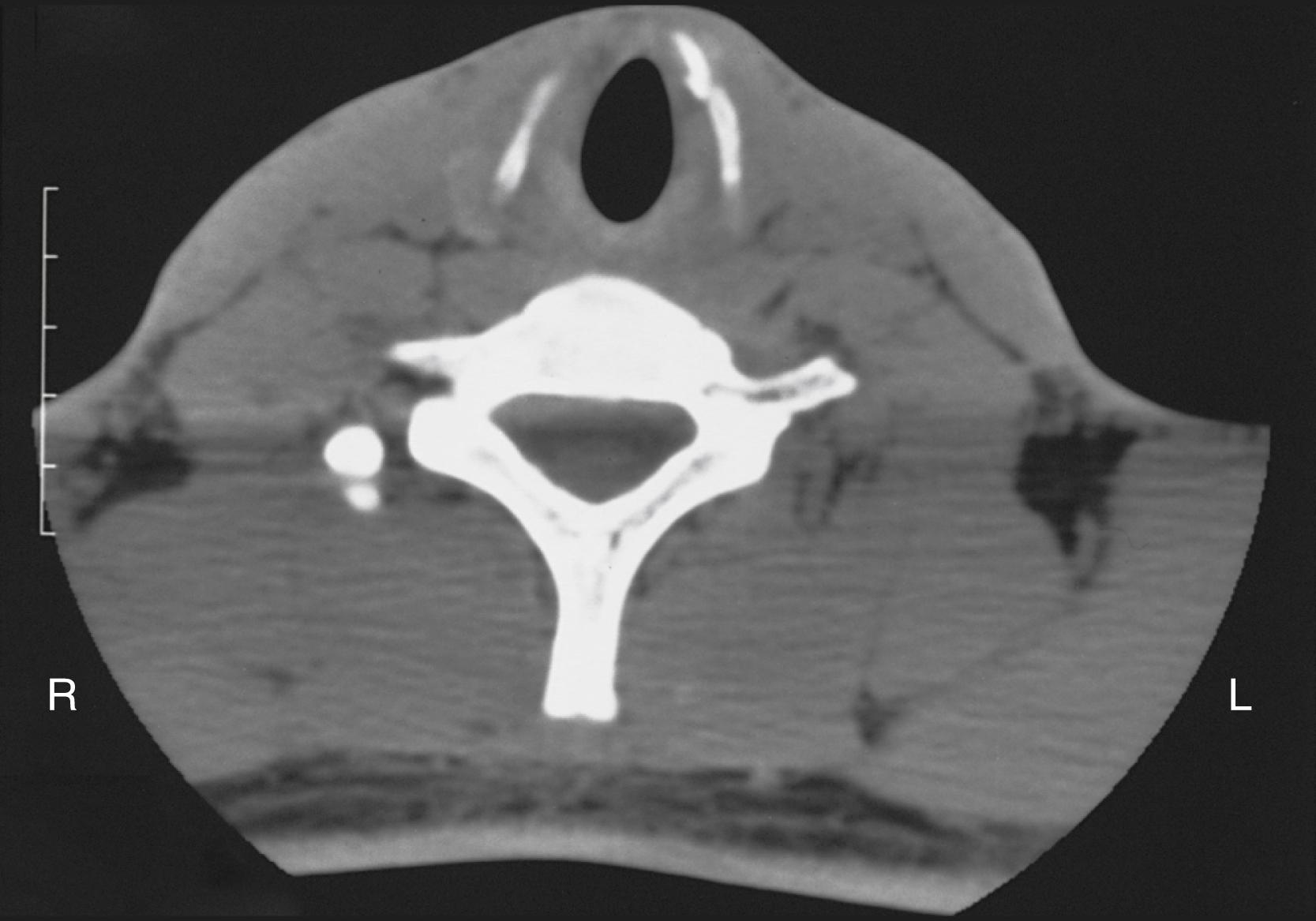
Presence or absence of laryngeal fracture
Laryngeal fracture displaced or nondisplaced
Esophagram should be considered for penetrating trauma near the esophagus.
Displaced laryngeal fracture
Foreshortened vocal fold
Exposed cartilage
Arytenoid
Thryoid
Cricoid
Narrowed airway due to cricoid fracture
Displaced fractures or soft tissue disruption almost always requires surgical exploration and repair.
Nondisplaced fractures should be treated only when obvious symptoms arise from the fracture.
With soft tissue disruption, interval tracheotomy may need to be performed. Early exploration invariably results in easier reduction of cartilaginous injury and more accurate soft tissue repair. Delay in the performance of the procedure leads to scarring, edema, local infection, and distortion of tissues that may result in a suboptimal outcome.
When possible, laryngeal exploration within 24 to 48 hours is ideal if the patient’s general condition permits.
Unstable from a cardiovascular perspective
Severe neurologic trauma
Presence of vascular trauma
Cervical spine clearance
Radiologic
Functional
Cardiovascular clearance
Neurosurgical clearance
Trauma surgeon assessment is complete
Coordination of surgical procedures and sequence of repairs between different surgical teams/specialties
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here