Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Laryngeal fractures are uncommon injuries that may be associated with life-threatening airway compromise.
The first and most important step in the management of laryngeal trauma is to verify and secure a safe airway.
Esophagoscopy should be performed in any patient going to the operating room to rule out concomitant injury.
The most common cause of internal laryngeal trauma is endotracheal intubation, especially in the setting of prolonged intubation.
Arytenoid dislocations are rare and may present similarly to unilateral vocal cord paralysis.
An experienced physician should manage the airway, and endotracheal intubation should only be performed under adequate visualization and when the larynx and trachea are in known continuity.
Intubating a patient blindly may convert a stable airway to an unstable airway.
Avoiding prolonged intubation is the most effective way to prevent internal laryngeal trauma.
Choosing the smallest endotracheal tube that will provide adequate ventilation will help to minimize mucosal trauma.
Laryngeal trauma should be included in the differential diagnosis when evaluating a patient with vocal cord paralysis.
External laryngeal trauma is rare, with an estimated incidence of 1 in 137,000 inpatient admissions and 1 in 30,000 emergency room visits. Laryngeal injuries in the pediatric patient are even more uncommon and account for <0.5% of trauma admissions compared to 1% of adult trauma admissions. The occurrence of blunt trauma injuries has decreased in the past several decades owing to improved automobile safety. However, the incidence of penetrating trauma has increased due to a rise in violent crimes.
Surrounding structures: Multiple surrounding structures shield the larynx and provide protection from external trauma. These structures include the mandible superiorly, sternum and clavicles inferiorly, sternocleidomastoid muscles laterally, and vertebrae posteriorly. Anterior soft tissue, including the strap muscles, provides minimal protection from the anteriorly directed force. In pediatric patients, the larynx is located higher in the neck in relation to the mandible and is thus further protected.
Laryngeal mobility: The larynx is mobile in multiple directions, most prominently in the lateral plane but also in the anterior/posterior and superior/inferior planes. This mobility allows it to be pushed out of the way by external forces.
Tissue pliability: In adults, ossification of the larynx increases the chances of fracture in the setting of blunt trauma. In children, laryngeal cartilages remain pliable and are consequently more resistant to fracture.
Blunt trauma occurs as the result of an anterior force compressing the larynx against the fixed vertebral column. These injuries most commonly result from motor vehicle accidents despite the use of seatbelts and airbags and occur when the hyperextended neck is thrust onto the dashboard or steering wheel during rapid deceleration. Similar crush injuries can occur during sports (i.e., ice hockey or karate), hanging, or strangulation. Another subset of these injuries includes “clothesline” injuries in which a thin horizontal structure (e.g., barbed wire fence) is struck at high speed in the cervical region.
The severity of trauma is variable but is generally proportional to the velocity or kinetic energy the struck object imparts to the surrounding tissues. Additional information regarding the size and shape of the blunt or penetrating object is also helpful. A larger force distributed over a smaller surface area is more likely to result in penetrating trauma than blunt trauma. Fortunately, penetrating injuries are much less common and occur as a result of violent crime and military conflicts, such as stab or bullet wounds.
Dyspnea, dysphonia, dysphagia, odynophagia, stridor, hoarseness, pain over the anterior neck, and hemoptysis are common symptoms of laryngeal trauma. The severity of symptoms may not correspond with the extent or rate of progression of the injury and the potential for impending airway obstruction.
Physical examination results may range from asymptomatic to critically ill, with typical findings including tenderness or ecchymosis over the larynx; loss of anatomical landmarks on neck palpitation that may indicate hyoid or laryngeal fracture; subcutaneous emphysema, particularly in the setting of positive pressure ventilation; cyanosis; air escaping from the neck wound; or persistent pneumothorax despite chest tube placement. Note that these patients are often at risk of cervical spine and vascular trauma.
Patients may present with mild symptoms and progress to airway compromise over minutes to hours due to progressive edema, hematoma, or instability of the laryngotracheal framework. Eliciting the time course of symptoms and signs is therefore important in determining management. Observation is recommended if history and physical examination are at all concerning, and the patient may require frequent examination by personnel with experience in neck trauma.
The initial step in the management of any trauma patient, including those with laryngeal trauma, follows the advanced trauma life support (ATLS) protocol. The first step in airway management is to determine whether the patient displays signs and symptoms of impending airway compromise such as stridor, dyspnea, respiratory distress, or aphonia. If a patient exhibits signs of airway compromise, a secure airway must be obtained as soon as possible. There are several methods that are appropriate for securing the airway in the setting of laryngeal trauma, including intubation, tracheostomy, and cricothyroidotomy.
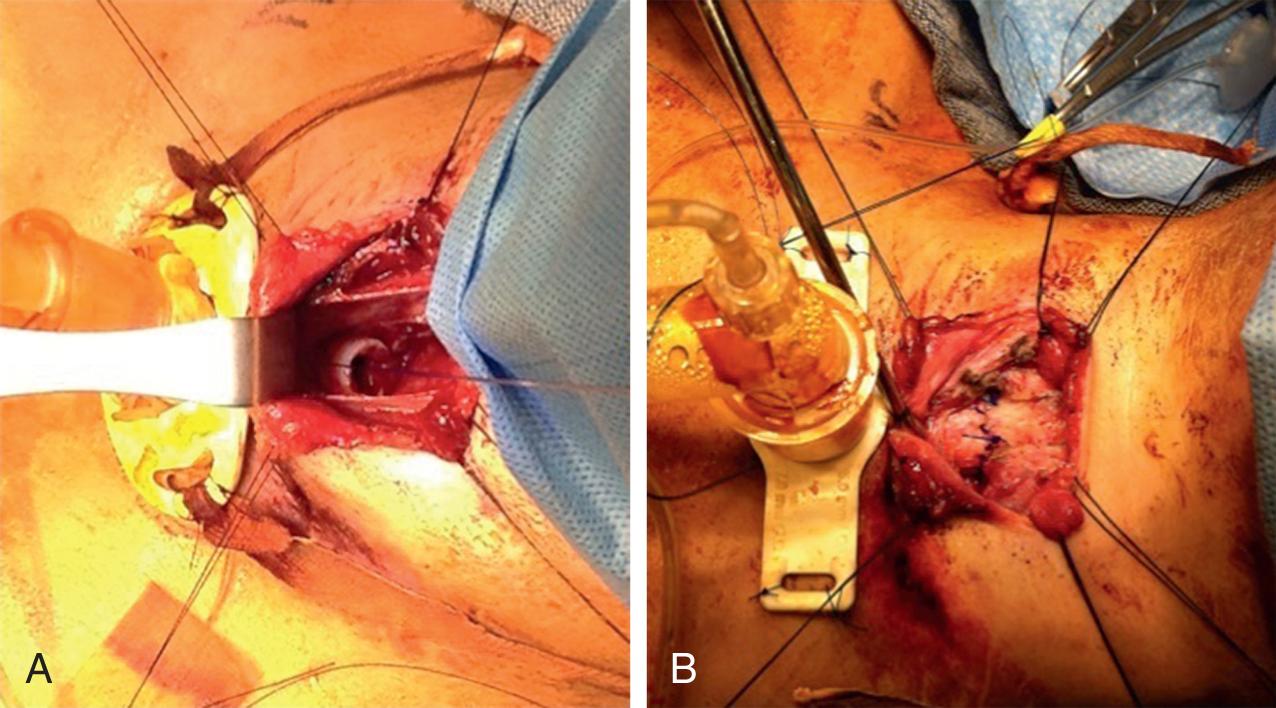
Several factors must be considered when choosing which method will be used to secure the airway, including patient stability and injury severity. Airway control should occur in the emergency room or, when possible, the operating room to allow for optimal direct and endoscopic evaluation. For endotracheal intubation to proceed, the larynx and trachea must be clearly intact and in continuity to prevent mucosal trauma, destabilization of laryngeal fractures, laryngotracheal separation, and further respiratory compromise. This can be done by placing an endotracheal tube over an endoscope to allow inspection of the airway and intubation. In addition, consideration should be given to the status of the cervical spine, which may be unknown at that point in the evaluation. Spinal stabilization should be maintained until it is clinically and/or radiographically cleared. It is important to note that intubation should be performed by an experienced physician to help prevent intubation-related trauma ( Fig. 80.1 ).
If the airway is determined to be unstable, awake tracheotomy in the operating room should be performed. Cricothyroidotomy is reserved for patients with a rapidly deteriorating airway, those who do not meet the optimal conditions for intubation, or those in whom tracheostomy is not possible due to patient factors or availability of physicians experienced in the surgical airway. Cricothyroidotomy should subsequently be converted to tracheostomy to prevent the development of subglottic stenosis. Following emergent management of the airway, these patients should undergo endoscopic evaluation of the aerodigestive tract in the operating room.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here