Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Compared with traditional open ventral hernia repair, minimally invasive approaches offer several advantages, including reduced wound and mesh infections, quicker return of bowel function, and reduced length of hospitalization as well as improved cosmesis. However, not everyone is a candidate for laparoscopic repair. Size and complexity of defects, history of infection, prior hernia repairs or abdominal surgeries, body habitus, and comorbidities all are factors that should be weighed to determine if laparoscopic repair is appropriate.
Laparoscopic repair of ventral hernias borrows much from the open techniques espoused by Rives and Stoppa. It maintains the tenets of large mesh overlap with transabdominal fixation of the prosthetic. In a standard laparoscopic ventral herniorrhaphy, the mesh prosthetic is placed intra-abdominally in an underlay position. Because the mesh lies juxtaposed to the underlying viscera, a tissue-separating mesh is required to reduce visceral adhesions to the mesh.
Traditionally, the hernia defect is bridged with mesh; however, some surgeons advocate closing the defect with transabdominal sutures. Potential benefits of defect closure include reduced seromas and mesh exposure in the event of superficial infection as a result of dead space obliteration above the mesh. Additionally, the law of LaPlace dictates that there will be increased tension on the bridged portion of mesh from a hernia repair without defect closure. This increased tension may ultimately lead to mesh “eventration,” or bulging of the mesh within the hernia sac. Based on Pascal’s principle, closing the defect would equalize pressure across the mesh. Another theoretical benefit of defect closure is akin to open repairs with reapproximation of the midline, restoring a more native and functional abdominal wall with medialization of the rectus muscles. The biggest drawbacks of defect closure are additional operative time spent closing the defect and increased postoperative pain from additional transfascial sutures.
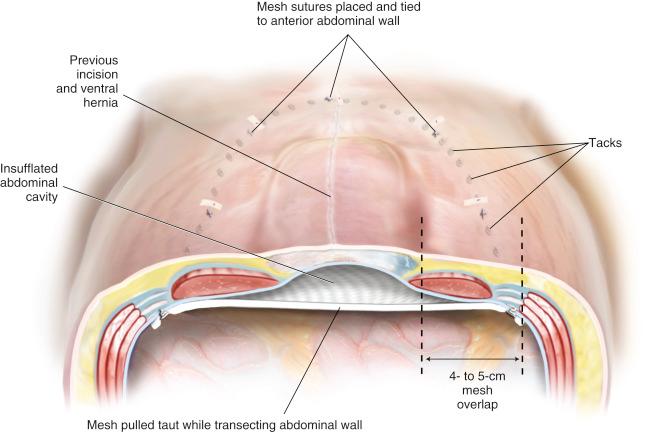
The amount of mesh overlap required for a durable ventral hernia repair is unknown. Based on Pascal’s principle, the intra-abdominal pressure is evenly distributed over a large surface area of mesh. The initial experience with laparoscopic ventral herniorrhaphy reported a 3-cm overlap of mesh, but the current recommendation is at least a 4- to 5-cm margin. The amount of overlap depends on the diameter of the largest hernia defect and the thickness of the patient’s abdominal wall. One large defect warrants at least 5 cm, whereas numerous small defects (“Swiss cheese” defects) may require only 4 cm of additional mesh. If hernia defect closure is chosen at the time of repair, a generous overlap of at least 5 cm is still recommended; therefore a minimum of 10- to 12-cm-wide mesh should be used.
In a laparoscopic ventral hernia repair, the mesh is placed in an insufflated abdominal cavity. Ideally there is a slight degree of tension on the mesh at the completion of the repair. The mesh does not lie flush against the underside of the abdominal wall. Rather it transects the abdominal space, so that when the abdominal cavity is desufflated, the mesh will not occupy the hernia sac ( Fig. 2.1 ).
When considering candidates for a laparoscopic ventral hernia repair, certain patient characteristics must be considered. Contraindications include the following:
Inability to tolerate general anesthesia
Hypercoagulability
Active infection
Loss of domain
Poor skin quality overlying hernia (ulceration, skin graft)
Patient expectations (scar revision or panniculectomy desired)
Surgeon skill, particularly in the area of adhesiolysis, needs to be factored in when choosing a laparoscopic ventral hernia repair. Factors that portend a more difficult case requiring experience with the technique include the following:
Multiple previous laparotomies
Previous intra-abdominal mesh
History of peritonitis
Atypical location of hernia (suprapubic, subxiphoid, flank)
The preoperative consultation is critical in a patient undergoing laparoscopic ventral herniorrhaphy. Although a minimally invasive approach, laparoscopic ventral hernia repair can result in significant postoperative pain and is not much different from an open repair in terms of postoperative discomfort. The real benefit of the laparoscopic approach is the well-documented reduction in wound- and mesh-related infectious complications. The likelihood of postoperative seroma formation should be discussed. The need for conversion to an open repair and the possibility of an enterotomy should be considered as well. The anticipated options if an enterotomy occurs should be explained to the patient, including delayed repair of the hernia defect until the abdomen is free from contamination.
Because ventral hernias can usually be identified on physical examination, no further work-up generally is required. However, computed tomography (CT) of the abdominal wall can be helpful in a patient who is morbidly obese, has a recurrent hernia (particularly with intra-abdominal mesh), demonstrates a defect in proximity to a bony structure (ie, suprapubic, subxiphoid, flank defects), or has concern for loss of domain.
Patients with previous failed attempts at repair can be difficult to treat. The reasons for recurrence are usually unknown, but efforts should be made not to repeat errors of the past. All operative reports that pertain to prior hernia repairs should be obtained to determine the mesh or meshes used and planes disrupted by prior repairs. Before approaching a recurrent defect, the surgeon should feel extremely confident with adhesiolysis and have a low threshold to convert to an open procedure. Patients who have had previous mesh infections that required removal of the prosthesis pose an extremely difficult challenge and should be considered for open repair.
The preoperative orders consist of antibiotic and deep venous thrombosis prophylaxis. A first-generation cephalosporin is typically given, and the dosage is adjusted for morbidly obese patients. Because patients with ventral hernia are frequently obese, will be less mobile postoperatively, and will experience increased intra-abdominal pressure from pneumoperitoneum, sequential compression devices and subcutaneous heparin are employed preoperatively.
For most patients with defects in the midline, supine positioning with both arms tucked is optimal, as this allows superior access for trocar placement and instrumentation. The pressure points at the elbow and wrist should be padded ( Fig. 2.2 ). For larger patients, arm sleds may be required. In patients with defects off the midline or lumbar defects, a bump may be placed under the hip on the side of the hernia, or a true lateral position may be necessary with the aid of a beanbag.

A Foley catheter is placed for bladder decompression; a three-way Foley catheter may be used to insufflate the bladder for identification in the repair of suprapubic defects. Gastric decompression is usually reserved for patients requiring a difficult orotracheal intubation and may be achieved with orogastric tube decompression.
The patient should be prepared and draped widely to allow lateral trocar placement. An iodine-impregnated adhesive drape is applied to the patient’s skin after preparation and draping to protect the biomaterial from the patient’s skin flora.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here