Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the first laparoscopic cholecystectomy was successfully performed in 1987, there has been a remarkable adoption of minimally invasive techniques, which has dramatically changed the field of general surgery. The surgical management of inguinal hernias, traditionally one of the most commonly performed procedures by the general surgeon, has paralleled the natural evolution of such surgical innovation. Compared with the open tension-free technique, laparoscopic inguinal hernia repair has been found to be associated with less postoperative pain, as well as a more rapid return to normal activities. In addition, the laparoscopic approaches are advantageous for patients with bilateral hernias because the same incisions can be used to access and repair both sides. Similarly, by avoiding the anterior scarring and previously placed mesh, these minimally invasive surgical (MIS) techniques are optimal in repairing recurrences associated with a prior open repair. A thorough understanding of the anatomy of the groin is crucial for both techniques to achieve a durable repair and minimize the risk of complications.
The transabdominal preperitoneal (TAPP) and the totally extraperitoneal (TEP) are the most commonly performed of the available MIS techniques. Broadly speaking, the major difference between the two approaches is in the access and development of the preperitoneal space. Otherwise, the tenets associated with each operation are essentially the same.
The TAPP approach first requires entry into the abdomen and then the creation of the preperitoneal space. An incision of the peritoneum just lateral to the medial umbilical ligament is extended laterally to the level of the anterior superior iliac spine (ASIS). The peritoneal flap is developed by bluntly dissecting the peritoneum from the transversalis fascia. The hernias are exposed and reduced. Ultimately the pocket for placing the mesh into the preperitoneal space is created. Upon completion of mesh placement, the peritoneal flap is then closed so that the mesh is excluded from the abdominal viscera.
In contrast, the TEP approach does not require entry into the peritoneal cavity. Rather, a balloon dissector or blunt telescopic dissection can be used to develop the preperitoneal space directly. Mesh is then placed and secured in a similar manner to the TAPP technique. Closure of the peritoneum is therefore not necessary.
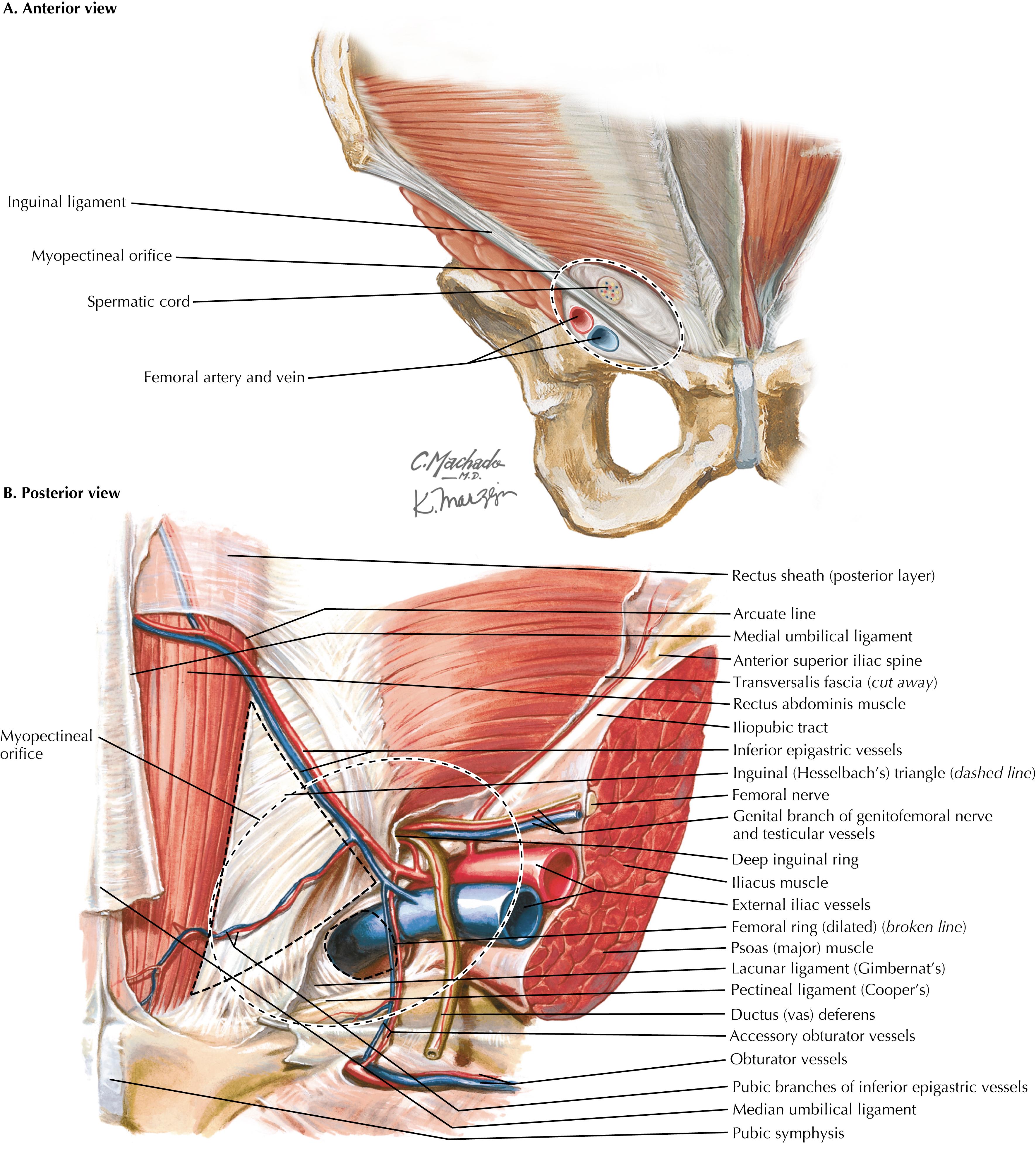
Initially named by Dr. Henri Fruchaud, the myopectineal orifice is a critically important feature of groin anatomy ( Fig. 37.1 , dashed ovals ). All groin hernias originate from within this area of weakness, which is covered only by the transversalis fascia and the peritoneum. Superiorly and medially, this aperture is bordered by the rectus muscle and the conjoined tendon, inferiorly by the superior pubic ramus and the pectineal (Cooper’s) ligament, and laterally by the iliopsoas muscle and the lateral border of the femoral sheath. The myopectineal orifice is divided into two by the inguinal ligament. The suprainguinal region contains the spermatic cord in males or the round ligament in females, and the infrainguinal region contains the femoral nerve, femoral artery, and femoral vein. The goal of mesh placement in either inguinal hernia repair is coverage of the entire region.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here