Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ovarian cystectomy is the treatment of choice for the conservative management of ovarian cysts presumed to be benign. Simple aspiration is associated with a high recurrence rate, and a cyst fluid cytology test is unreliable. Transvaginal ultrasonography is used to evaluate an ovarian cyst. High-risk criteria on ultrasonography for predicting the pathologic diagnosis, such as a cystic-solid mass or ascites, are a contraindication to laparoscopic surgery unless a dermoid or endometriosis is suspected. A preoperative CA-125 level is useful in postmenopausal, but not in premenopausal, women. The same principle applies to Doppler flow assessment. Magnetic resonance imaging (MRI) does not help in distinguishing a malignant from benign mass.
An attempt should be made to remove the cyst without rupture. Equivalent rates of rupture are found with laparotomy and laparoscopy. Rupture of a dermoid cyst does not appear to be associated with any short-term complications if copious irrigation is used. Intraoperative rupture of stage I ovarian carcinomas does not appear to affect prognosis.
The patient should have consented to a laparotomy if cancer is found. Pneumatic compression stockings are placed on the calves. An orogastric tube is used if stomach distention is suspected. An examination is carried out with the patient under anesthesia, and a Foley catheter is inserted.
For an ovarian cystectomy to be performed, the standard three-puncture technique is used. The peritoneal cavity is systematically assessed as described in Chapter 113 . Peritoneal fluid should be obtained for cytology. If no excrescences or peritoneal signs of malignancy are present, the surgeon can proceed with the cystectomy.
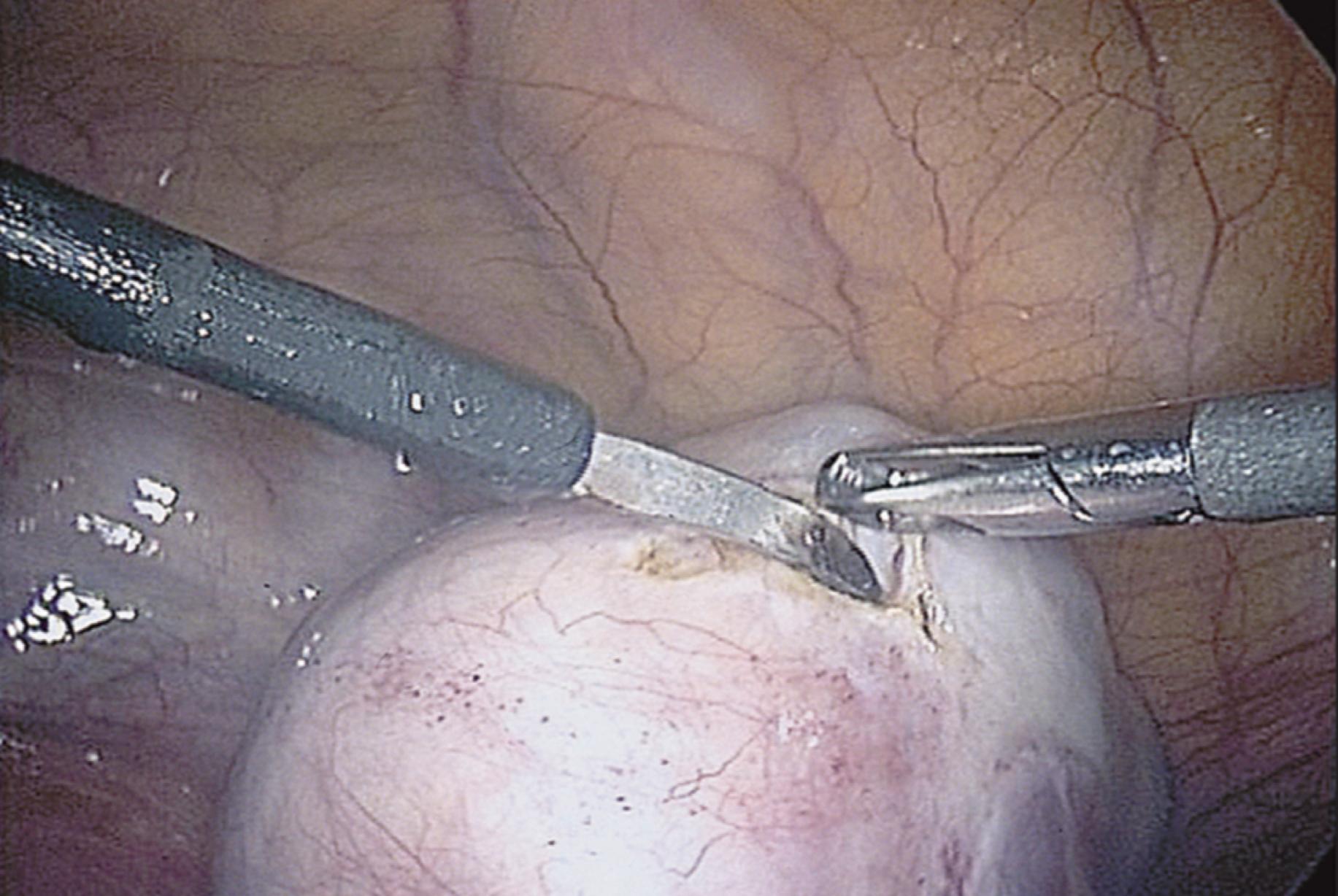
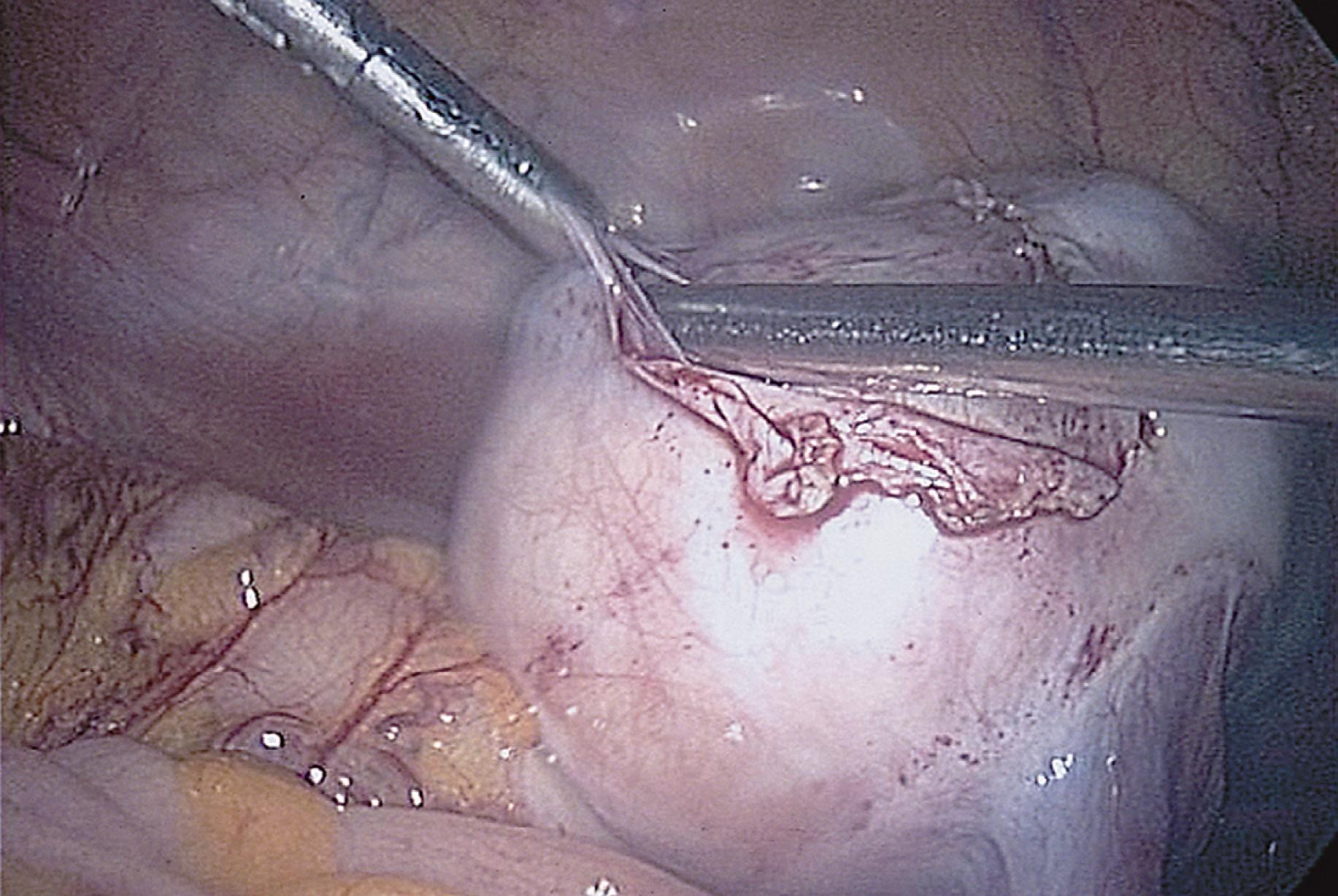
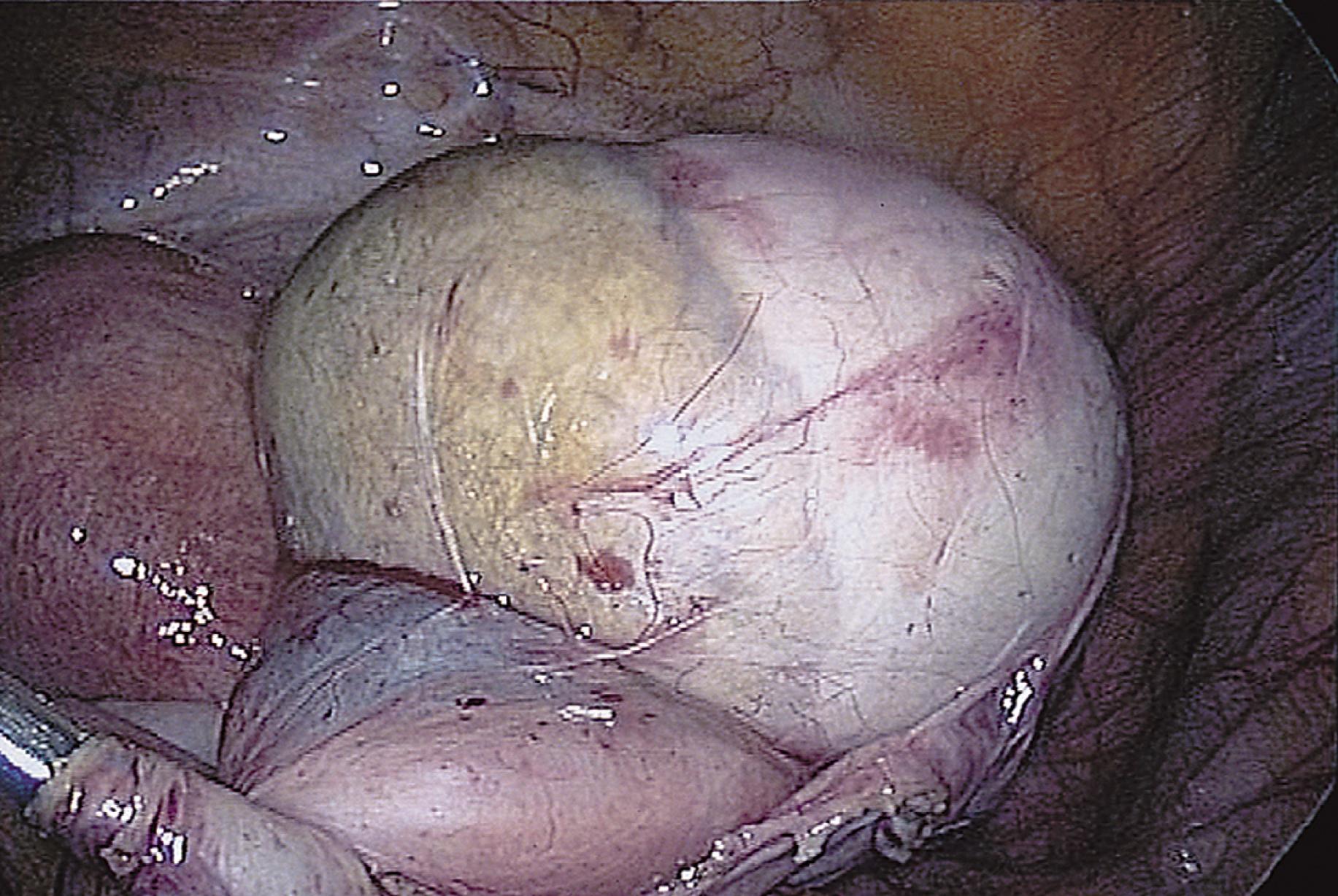
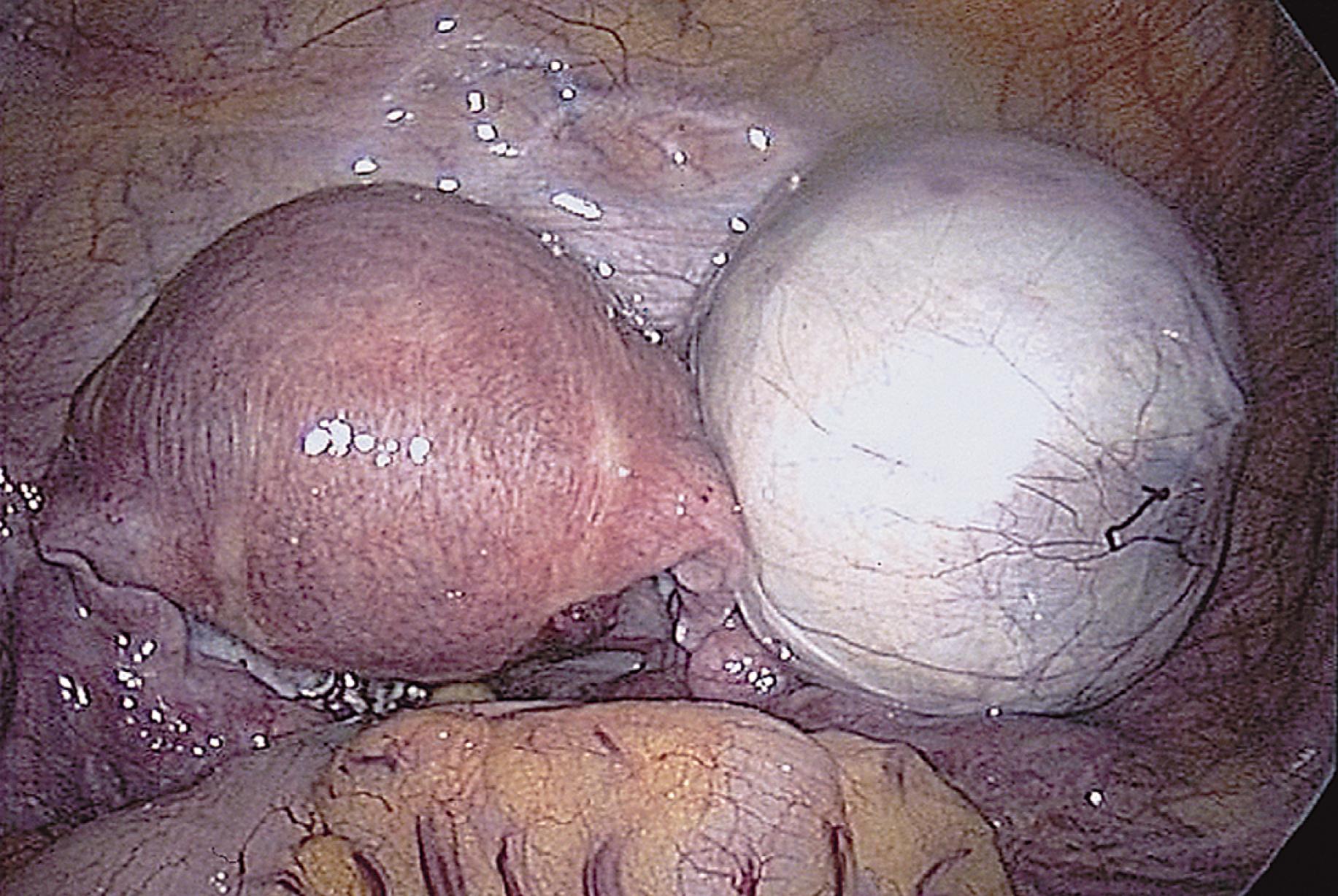
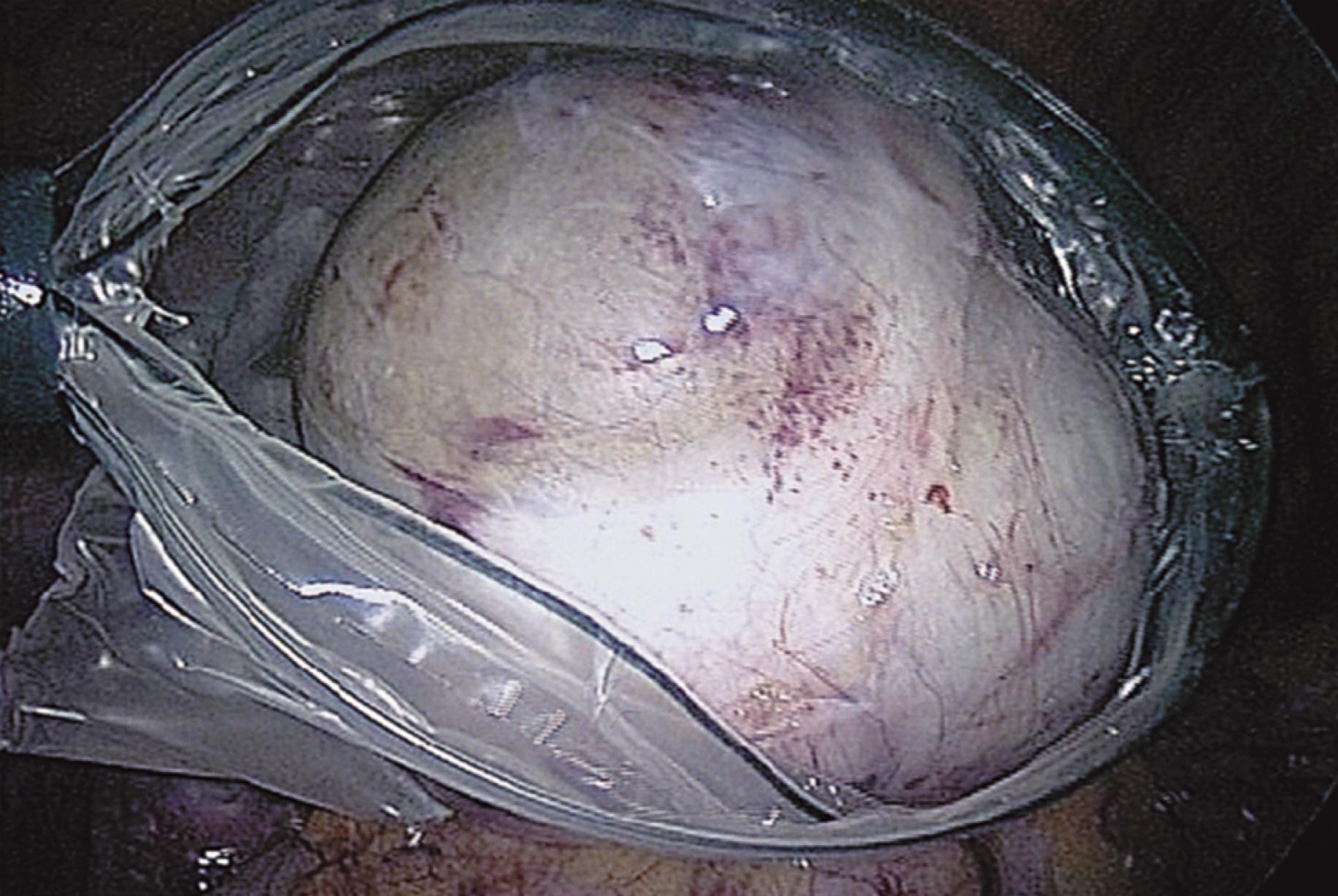
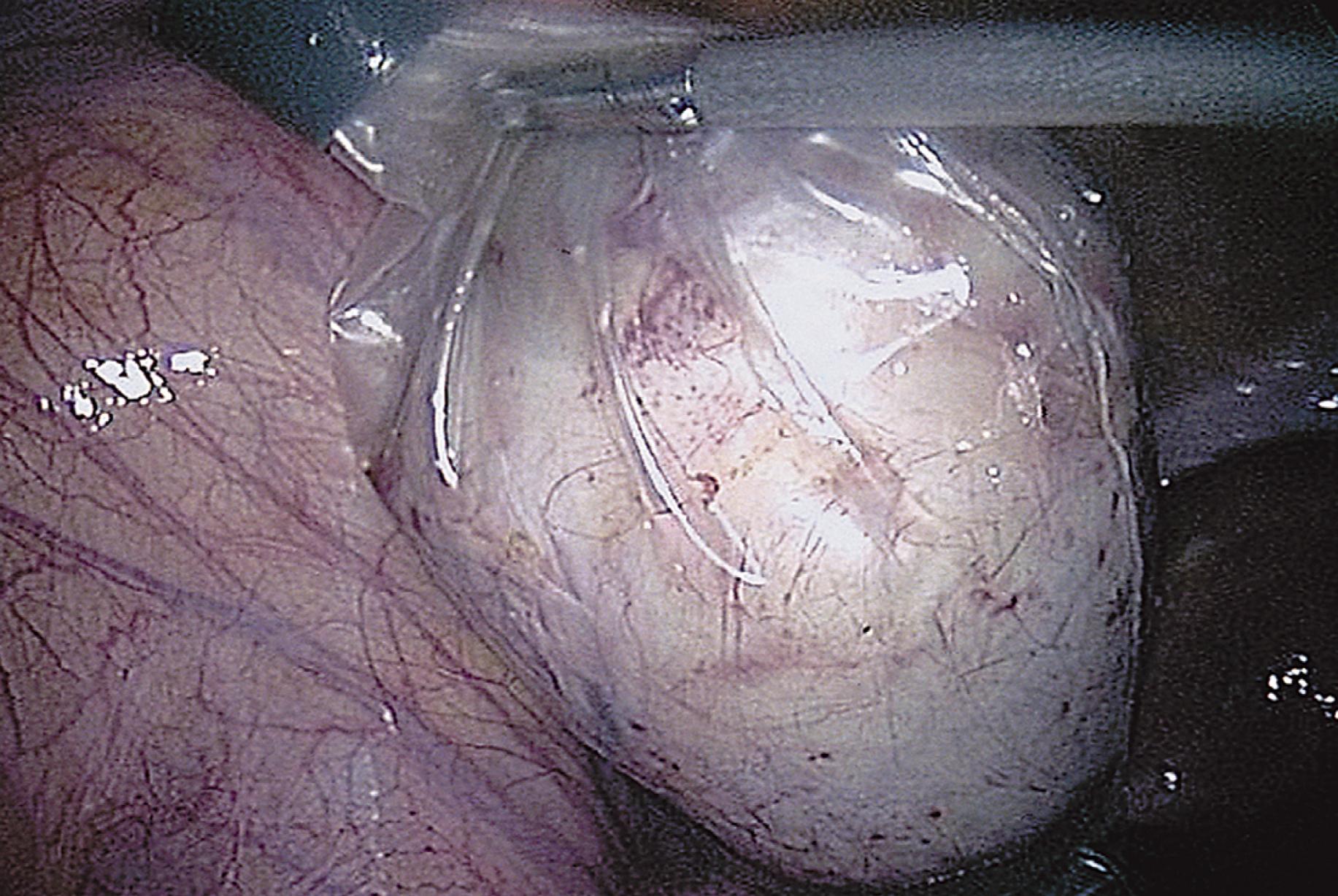
The ovarian cortex is coagulated, and an incision is made ( Fig. 115.1 ). The edge of the cortex is grasped with an Allis forceps and dissected from the cyst. The cyst can be separated from the cortex with blunt dissection with the use of the suction-irrigation device ( Fig. 115.2 ). The cyst is then enucleated from the ovary ( Fig. 115.3 ) and placed into the anterior cul-de-sac ( Fig. 115.4 ). Bipolar electrosurgery is used to achieve hemostasis from any blood vessels encountered. Once the cyst is ready to be removed from the peritoneal cavity, it is placed in a bag ( Fig. 115.5 ). The bag is then brought up to the skin, and the cyst is decompressed within it ( Fig. 115.6 ). The cyst can then be morcellated out of the bag. The ovarian cortex is not usually closed, but a simple suture can be applied to close a deep defect.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here