Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In most parts of the face and neck, a component of the superficial musculoaponeurotic system (SMAS) lies just deep to the subcutaneous fat.
SMAS elevation by suspension with deep anchorage can provide stable correction of mid-face, lower face, and neck ptosis.
Optimal suspension of the SMAS layer requires the release of retaining ligaments beneath this fascia (in the deep plane) in order to increase its mobility.
Tumescent anesthesia greatly reduces postoperative morbidity in face-lift surgery.
The structures at greatest risk of injury in face-lift surgery are branches of the facial nerve.
Liposuction of the neck and jowls enhances the results of face-lift surgery.
Facial aging occurs through three mechanisms: photoaging, gravitational aging, and volumetric aging. Photoaging is the result of sun damage and primarily affects the skin; it probably does not occur to a significant degree in tissues deeper than the dermis. Gravitational aging is evidenced by stretching and sagging of soft tissues, especially those of the superficial fascia of the face and neck, the superficial musculoaponeurotic system (SMAS). Volumetric aging is manifested by atrophy of soft tissues (primarily fat and muscle) and of bone. Soft tissue atrophy is most evident in the anterior face and cheeks and can produce hollowing in the mid-cheek and infra-orbital areas. Bone atrophy results in recession of the maxilla and mandible. Volumetric aging has an unknown etiology.
The most effective solution to gravitational aging is lifting surgery. The goal of a face lift (rhytidectomy) is to elevate sagging soft tissue along vectors that reverse the effect of gravity on those tissues. The SMAS fascia is the preferred soft tissue layer for lifting because it can be mobilized and is robust enough to sustain long-term lifting. SMAS mobility is limited by retaining ligaments (zygomatic and masseteric) that anchor this fascia to underlying fixed tissues. In a deep plane face lift, as described in this chapter, these retaining ligaments are divided, thus increasing mobility of the SMAS when lifting tension is applied. The mobilized SMAS connective tissue layers re-adhere during healing, affording long-term stability of the SMAS in its lifted position.
This chapter describes a minimum incision (short scar) rhytidectomy that can be performed under tumescent local anesthesia. It reviews the anatomy of the neck, lower face, and mid-face regions and discusses how face-lift surgery can correct gravitational aging of these structures. In this surgery, tumescent local anesthetic solution is infused throughout the operative field. The tumescent anesthetic solution can be administered in a nearly painless fashion, thus enabling the use of minimal perioperative sedation. The tumescent anesthetic facilitates surgical dissection in the subcutaneous and deep (sub-SMAS) planes and also enhances hemostasis. The prolonged vasoconstriction that results from the use of the tumescent anesthetic results in reduced postoperative ecchymosis and edema, which greatly accelerates the patient's recovery.
Traditional face lifts include a significant posterior vector of SMAS lifting (toward the mastoid area) in order to improve sagging soft tissues in the neck. The relatively posterior direction of tightening of the SMAS/platysma layer in the neck creates significant skin redundancy in the postauricular and mastoid areas. An extended skin incision in this area is thus necessary in order to enable excision of excess skin. This classical, extended incision often results in a visible scar, especially if the patient's hair is not worn so that it helps conceal the scar. The face lift described herein is a lamellar (multi-layered) technique in which a skin flap (created by subcutaneous undermining) and a deeper SMAS flap (created by sub-SMAS undermining and release of sub-SMAS retaining ligaments) are lifted along independent vectors. Compared with most deep plane face-lift techniques, the SMAS is incised in a relatively anterior and cephalad position on the cheek (a high-SMAS incision). The high-SMAS flap that is created by SMAS undermining and release of retaining ligaments is in a position to exert a greater lifting effect in the mid-face region. These lifting vectors on both SMAS and skin flaps are relatively superior (cephalad) compared with traditional face lifts and convey redundant neck and cheek skin upwards rather than backwards, enabling the use of a minimum-length skin incision that terminates just behind the earlobe. The SMAS suspension sutures are tied under significant tension. The skin can be closed in a predictable way after placement of key sutures and trimming of excess skin.
Safe and effective face-lift surgery requires a thorough understanding of facial anatomy, especially that pertaining to the superficial musculoaponeurotic system (SMAS) and its retaining ligaments, the platysma and other superficial muscles of facial expression, and motor nerve branches.
The SMAS is a complex mesenchymal tissue system that is most broadly defined as the superficial muscles of facial expression, fascial planes that are continuous with these muscles, and myriad septal attachments between these fascial planes and the dermis. Through the cutaneous attachments of the superficial facial musculature and of the fascial planes of the SMAS, contractions of the muscles are conveyed to the skin, resulting in facial expression. In most parts of the face and neck, a component of the SMAS lies just deep to the subcutaneous fat. The SMAS includes the platysma muscle in the neck and a robust fascia in the lateral cheek area. The fascial elements of the SMAS are continuous with, or envelop, many of the superficial muscles of expression.
In the anterior face, the superficial fascia level is continuous through the galea, frontalis, orbicularis oculi, cheek SMAS, and platysma. More posterior, in the temple region, the superficial fascia manifests as the superficial temporal fascia (also called temporoparietal fascia). This superficial fascia merges with deep temporal fascia at the zygomatic arch and is discontinuous with the SMAS of the cheek, which converges on the zygomatic arch from below.
The SMAS is attached to the dermis above and to deep immobile structures including bone or deep fascia via distinct retaining ligaments including the zygomatic (also referred to as “McGregor's patch”), masseteric, and mandibular ligaments. In addition, there are several ligamentous attachments between the SMAS and dermis in the periauricular areas ( Fig. 38.1 ). When performing a rhytidectomy, the surgeon creates a skin flap by undermining in the subcutaneous, supra-SMAS layer. Many superficial retaining ligaments (between the dermis and the underlying SMAS) must be divided during this undermining. Many of them surround perforating vessels and small sensory nerve branches. The vessels frequently require bipolar cautery for hemostasis; as a rule, the sensory nerves regenerate postoperatively, restoring sensation to the cheek region.
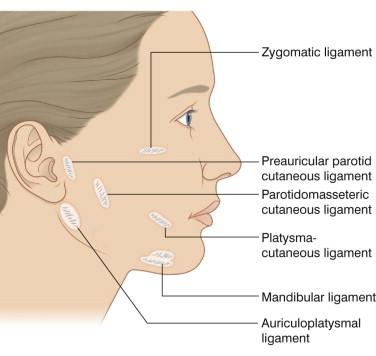
The platysma-cutaneous ligaments should be spared from division so that the suspended SMAS can convey lifting to the lateral perioral skin, thus affording improvement of ptosis of the lower nasolabial and marionette folds. The goal of deep plane (sub-SMAS) undermining is to create a mobile SMAS flap. The zygomatic ligaments (which attach deeply to bone) and the parotidomasseteric ligaments (which attach deeply to masseteric fascia) must be divided to enable adequate mobility of the SMAS flap.
The most important structure at risk of damage during face-lift surgery is the facial nerve ( Fig. 38.2 ). The nerve is deep to the parotid gland at its foramen and begins its branching deep to the gland. Inferior to the zygomatic arch, the facial nerve branches travel below the SMAS and innervate the superficial muscles of facial expression via the underside of the muscles. In a subcutaneous face lift, in which undermining is done superficial to the SMAS, all of these lower branches of the facial nerve are protected from injury by the SMAS itself. In a deep-plane face lift, undermining is performed beneath the SMAS, and zygomatic, buccal and marginal mandibular branches of the facial nerve are vulnerable to injury. The zygomatic and buccal branches are especially vulnerable during sub-SMAS release of the zygomatic and masseteric ligaments.
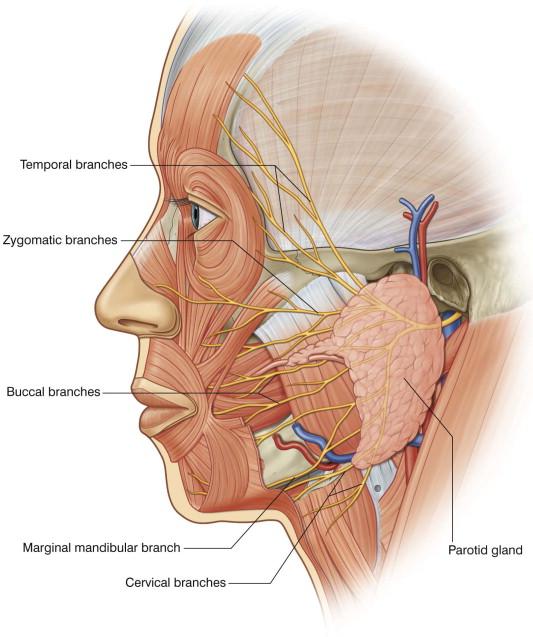
Cephalad to the zygomatic arch, the temporal branches of the facial nerve lie within the superficial temporal fascia ( Fig. 38.2 ). Care must be taken to undermine at a level superficial to this fascia (preferably within the subcutaneous fat) over and cephalad to the zygomatic arch. If the zygomatic arch or deep temporal fascia are to be used as anchor points for SMAS elevation, the distribution of temporal branch rami as they cross the zygomatic arch must be considered. In a study in which 35 cadaver hemifaces were dissected, the most posterior ramus of the facial nerve temporal branches crossed the zygomatic arch, on average, at a point 1.8 cm anterior to the auricle. The most anterior ramus of the temporal branch crossed the zygomatic arch on average at a point 2.0 cm posterior to the anterior origin of the arch.
Surgery that suspends the SMAS in a superior direction can reverse ptosis of the SMAS and attached soft tissues that are superficial to the SMAS. Elevated tissues include subcutaneous fat and skin, which are attached to the SMAS via myriad septal attachments between SMAS and dermis. The robust fascia of the cheek SMAS can withstand significant tension and is the ideal soft tissue layer to mediate lifting through suspension. In contrast, the dermis has much less tensile strength and will stretch to produce a spread scar if it is sutured under too much tension.
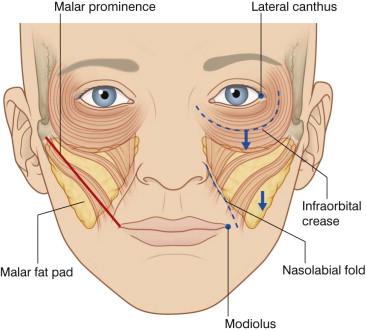
Recent anatomic studies have shown that in the mid-face (defined as the cheek medial to a line drawn from the malar prominence to the modiolus, Fig. 38.3 ), ptosis of the malar fat pad is largely responsible for the appearance of aging. The malar fat pad is a roughly triangular formation of subcutaneous fat that lies over the maxilla. Its supero-lateral corner extends into the malar area and its lower apex is near the modiolus. The malar fat pad is very fibrous and contains myriad dense connective tissue septae that connect the dermis to the underlying muscle fascia. Gravitational descent of the malar fat pad results in deepening of the nasolabial fold, infraorbital hollowing, and lowering and flattening of the youthful convexity of the mid-face. Cadaver dissection studies of the mid-face region have indicated that suspension of superficial tissues including the malar fat pad affords superior correction of mid-face ptosis.
When the SMAS is mobilized and suspended, it must be anchored to a relatively immobile point of fixture to maintain a stable lift. In general, the SMAS itself is relatively stable in the lateral cheek areas (preauricular and infra-auricular). The mastoid periosteum is a stable fixation point that can be used to secure platysma. Another fixation point for suspending the platysma is the auriculoplatysmal ligament, an immobile condensation of fascia in the inferior preauricular area. Skeletal fixation can also be achieved by suturing the SMAS to the periosteum of the zygoma or of the posterior zygomatic arch. Deep temporal fascia is another stable structure that can serve as an anchor for SMAS plication.
As with any major surgery, patients must avoid any prescription or over-the-counter medications that can predispose to bleeding. Aspirin should be discontinued 2 weeks prior to surgery. Vitamin E should be avoided starting 1 week before surgery. Because several over-the-counter herbal preparations can inhibit hemostasis, it is best to discontinue all herbal supplements 1 week preoperatively.
Patients who smoke should discontinue smoking at least 2 weeks prior to surgery and not resume for at least 2 weeks postoperatively. Smoking causes peripheral vasoconstriction, which can compromise revascularization of the face-lift skin flap and result in distal flap necrosis.
Preoperative laboratory evaluation should include bleeding parameters such as prothrombin and partial thromboplastin times and complete blood count (including platelets).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here