Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radiographs are the workhorse of knee imaging. Almost any symptom or sign may be initially evaluated with an x-ray. Radiographs provide useful information across the entire spectrum of knee pathology, including congenital deformities, arthritis, trauma, oncology, sports injuries, metabolic disease, and arthroplasty evaluation.
A brief orientation to x-ray technology enhances an understanding of knee imaging. An x-ray tube converts electricity into a beam of high-energy photons. The x-ray beam is aimed through the knee. A cassette containing x-ray film is positioned opposite the x-ray beam on the other side of the patient. Photons that pass through the patient strike the film, exposing it. Tissue density is the primary determinant of whether a photon successfully reaches the film. A dense tissue, such as bone, absorbs or deflects most photons. Thus few photons reach the film. Areas of unexposed film appear white, representing dense tissue. Less dense materials, such as the lung or fat, do not obstruct as many passing photons. Here the exposed film appears darker. Simplistically a radiograph is a shadow formed by high-energy light outlining the patient's anatomy.
Traditionally an exposed film was developed and hung for interpretation. Over the past 20 years, new cassette designs have replaced film with an imaging plate, creating computed radiography (CR). After exposure, the imaging plate is run through a CR reader, and the captured image is digitized. The imaging plate is subsequently reset and can be reused thousands of times. Digital radiography (DR) represents the next evolution of filmless image capture. DR dispenses with the cassette entirely and uses a flat panel detector. The detail and overall image quality of DR are superior to CR.
A remaining niche for true film radiography is the standing, frontal, long-standing view radiograph of the lower extremity. This may be requested for precise knee anatomic and mechanical axis measurements.
After an image has been acquired by a CR or DR reader, it is transmitted to the picture archiving and communication system (PACS) for interpretation. The advantages of PACS are manifold, including image manipulation (windowing, zooming, etc.), transmission (electronic), and storage (online, easily accessible). The time-honored file room has given way to a well-ventilated closet housing several hard-working computers.
Standard radiographic examination of the knee consists of three views: anteroposterior (AP), lateral, and axial (sunrise or Merchant). Tunnel, posteroanterior (PA) flexion weight-bearing (Rosenberg view), and oblique views may be performed for particular indications. In the setting of knee instability and ligamentous injury, stress radiographs may be performed. If a bilateral examination has been requested, each knee should be imaged separately.
The AP view is obtained with the knee extended, the cassette posterior to the knee, and the central x-ray beam perpendicular to the cassette. A standing (weight-bearing) AP radiograph more accurately assesses the joint space than one obtained with the patient supine. For this reason and to allow the estimation of valgus or varus angulation, weight-bearing images are preferable whenever possible ( Fig. 5.1 ). Normal structures evaluated on every AP radiograph of the knee are the patella, medial and lateral femoral condyles, medial and lateral joint compartments, tibial spines, medial and lateral tibial plateaus, and fibula. The AP view also provides a gross assessment of femoral tibial alignment ( Fig. 5.2A ). The lateral compartment is normally slightly wider than the medial.
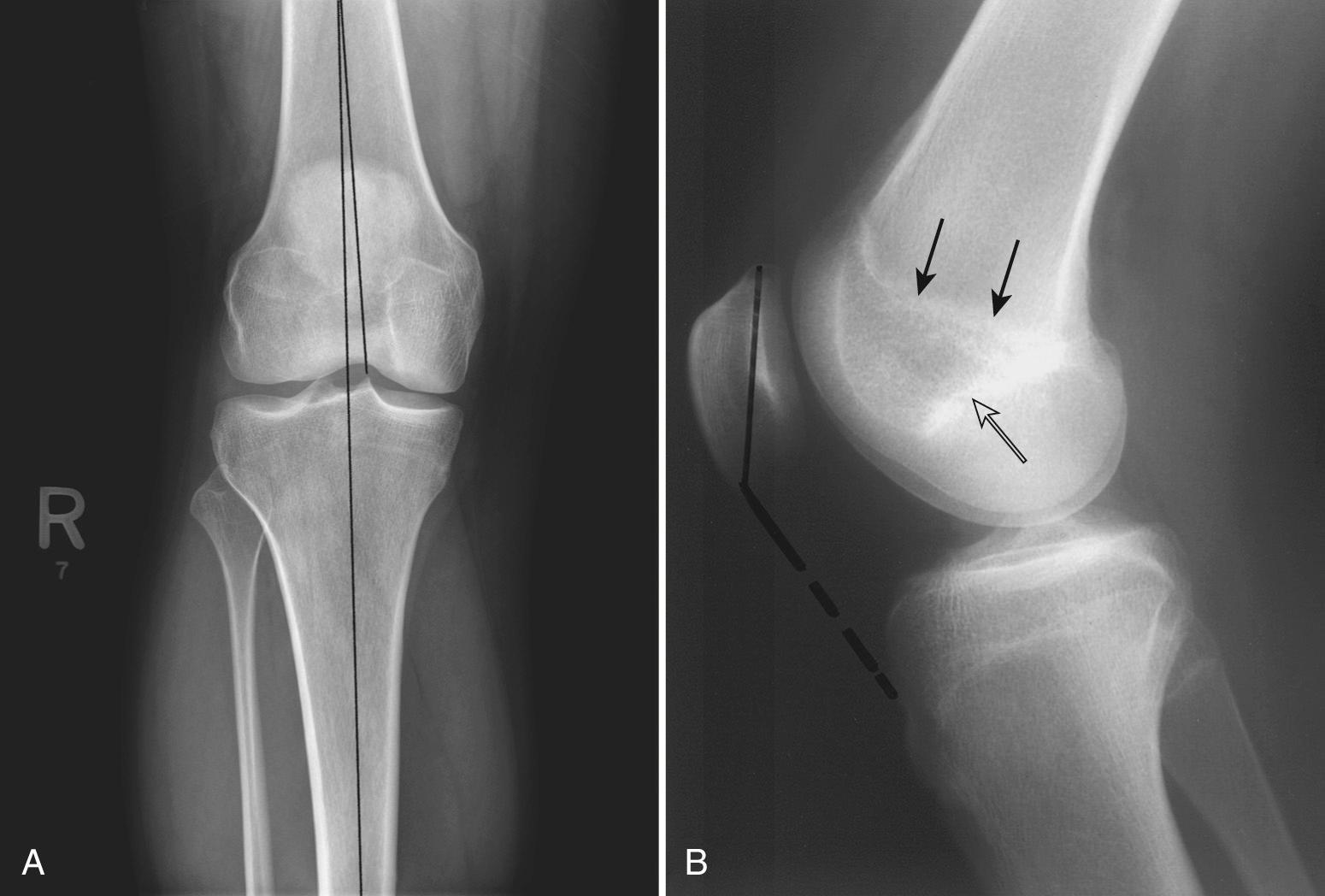
The lateral view is obtained with the knee flexed 30 degrees and the patient lying on the affected limb. The cassette is positioned under the lateral side of the knee, and the x-ray beam is directed perpendicular to the cassette. This view depicts the quadriceps tendon, patella, patellar tendons, suprapatellar bursa, distal femur, proximal tibia, and proximal fibula (see Fig. 5.2B ).
The medial femoral condyle is slightly larger than the lateral condyle. The lateral femoral condyle can be identified by the presence of the lateral femoral sulcus at the anterior aspect of its weight-bearing portion. Blumensaat line represents the roof of the intercondylar notch. The closed physeal scar is also evident on the lateral view, and the patella should fall between the closed scar and Blumensaat line.
The tibial plateaus slope downward as they progress posteriorly, which can aid in fracture identification. The plateaus may be differentiated by several clues. The higher of the two tibial spines belongs to the medial plateau. At its posterior extent, the medial tibial plateau projects most dorsally and is squared. In contrast, the posterior aspect of the lateral tibial plateau slopes smoothly downward with a rounded contour.
The quadriceps and patellar tendons are well evaluated on a lateral view. The distal quadriceps tendon attaches to the superior pole of the patella. The patellar tendon extends from the inferior pole of the patella to the tibial tubercle. Both structures are well demarcated by a posterior fat plane. They should be straight and of uniform thickness.
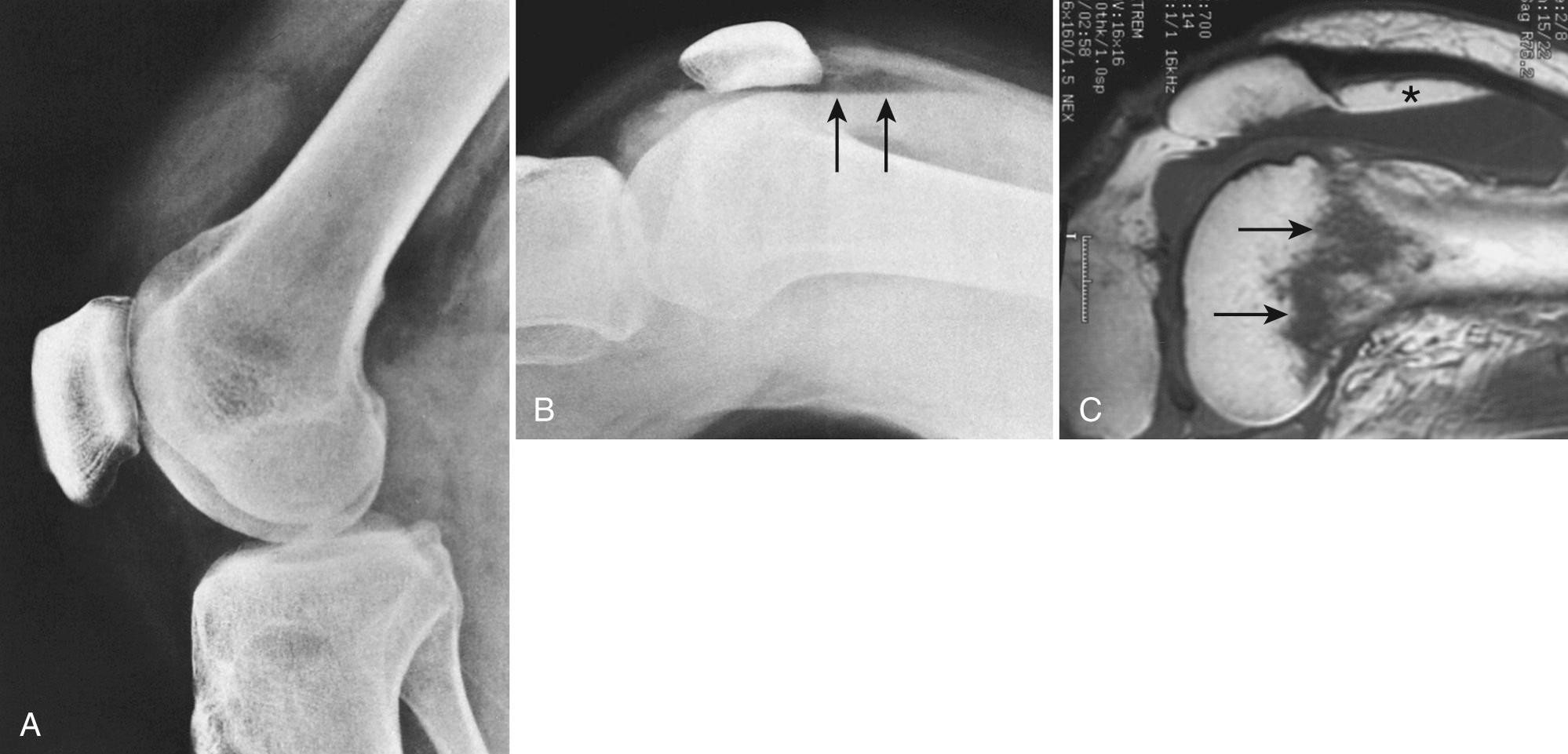
In the setting of a joint effusion and suspected occult intra-articular fracture, a cross-table lateral view is useful for evaluating for lipohemarthrosis. The view is obtained with the patient supine and the knee slightly elevated. The cassette is placed adjacent to the medial knee. This positioning, in contrast to the standard lateral view, is better tolerated by a traumatized patient. The presence of a fat fluid level indicates an intra-articular fracture (most commonly, the tibial plateau) and prompts further evaluation with computed tomography (CT) or magnetic resonance imaging (MRI) ( Fig. 5.3A to C ).
The suprapatellar bursa is the proximal extension of the joint space. It may be identified on the standard lateral view as a slender, 1- to 2-mm, vertically oriented structure contained within the lucent area of fat formed by the anterior margin of the distal femur and the posterior margin of the quadriceps tendon.
Superoinferior positioning of the patella may be evaluated using the Insall-Salvati ratio. This is the ratio of the greatest length of the patella divided by the length of the patellar tendon. This ratio averages 1.17 and normally falls between 0.8 and 1.2 (see Fig. 5.2B ). A long patellar tendon generates a ratio greater than 1.3, indicating a high patella (patella alta). Conversely, a short tendon accompanies a low patella and a ratio less than 0.8, termed patella baja.
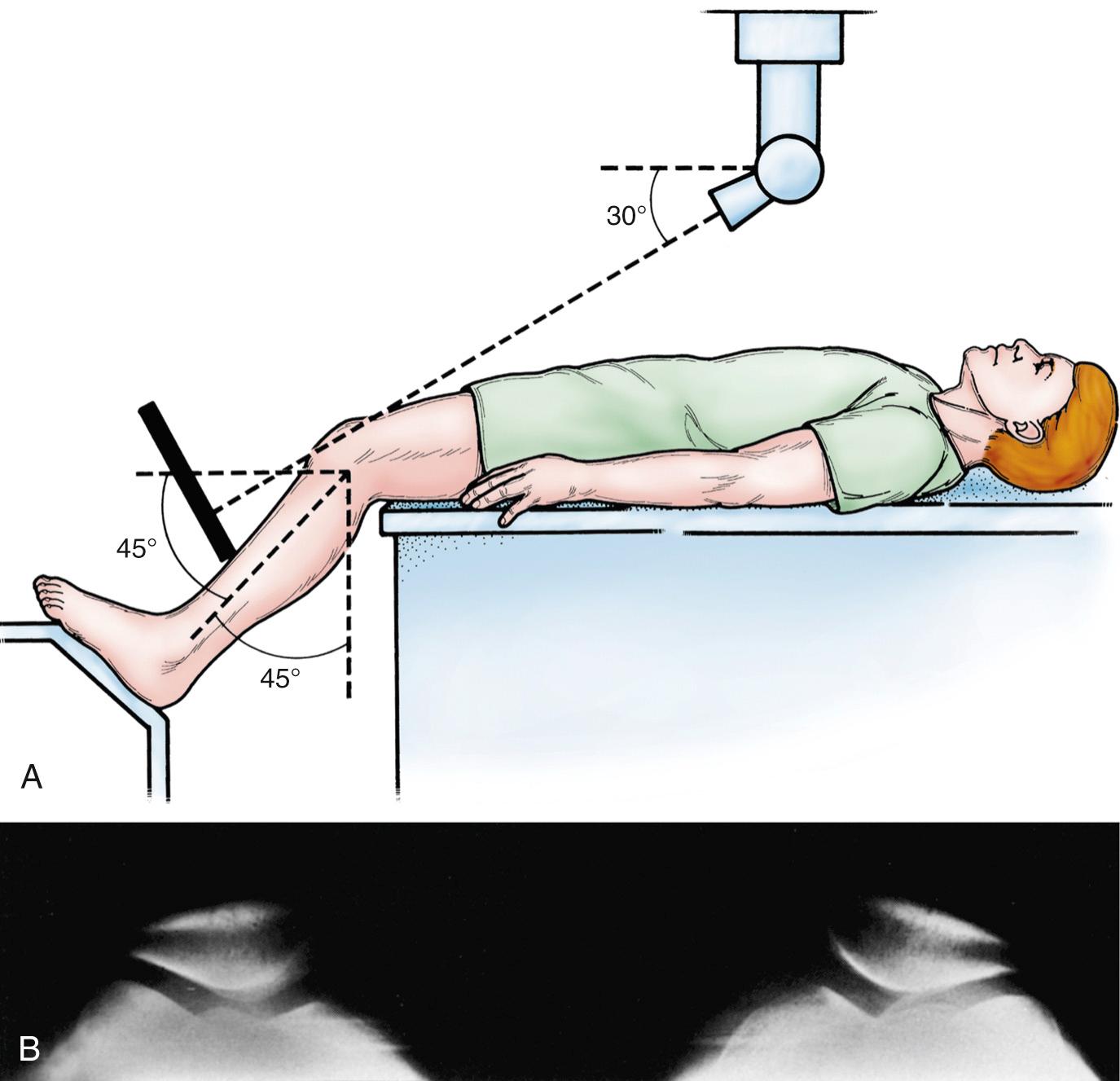
The axial view of choice is the Merchant view. The patient is placed in the supine position on the radiography table; the knees are flexed 45 degrees (using a fixed or adjustable platform), and the cassette is placed on the proximal part of the shins. Both knees are exposed simultaneously, with the x-ray beam directed toward the feet, inclined 30 degrees from the horizontal ( Fig. 5.4A ). This view provides an excellent assessment of patellofemoral alignment and is ideal for assessing the osseous patellofemoral articular surfaces (see Fig. 5.4B ). In contrast, a skyline (or sunrise) view is obtained with the patient prone and the knee in maximum flexion. This view demonstrates the posterior surface of the patella and the anterior surface of the femur, but the imaged femoral surface is not at the patellofemoral joint. Furthermore, accurate assessment of patellofemoral alignment is limited when the knee is flexed excessively. Some patients have difficulty tolerating this position.
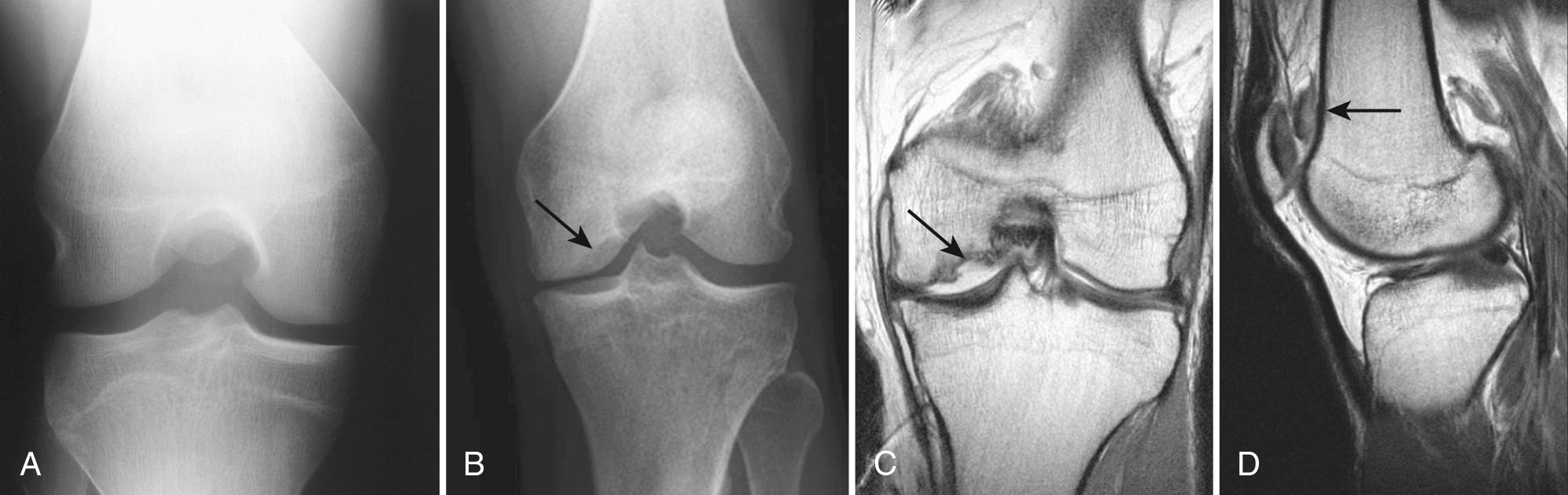
The tunnel view is a frontal view obtained with the knee flexed 60 degrees. It can be obtained AP with the patient in the supine position, or PA with the patient prone or kneeling on the cassette. The x-ray beam is directed perpendicular to the tibia. This view demonstrates the posterior aspect of the intercondylar notch, the inner posterior aspects of the medial and lateral femoral condyles, and the tibial spines and plateaus ( Fig. 5.5A ). It is ideal for evaluating patients with suspected osteochondritis dissecans, which tends to occur more posteriorly in the intercondylar notch (see Fig. 5.5B to D ).
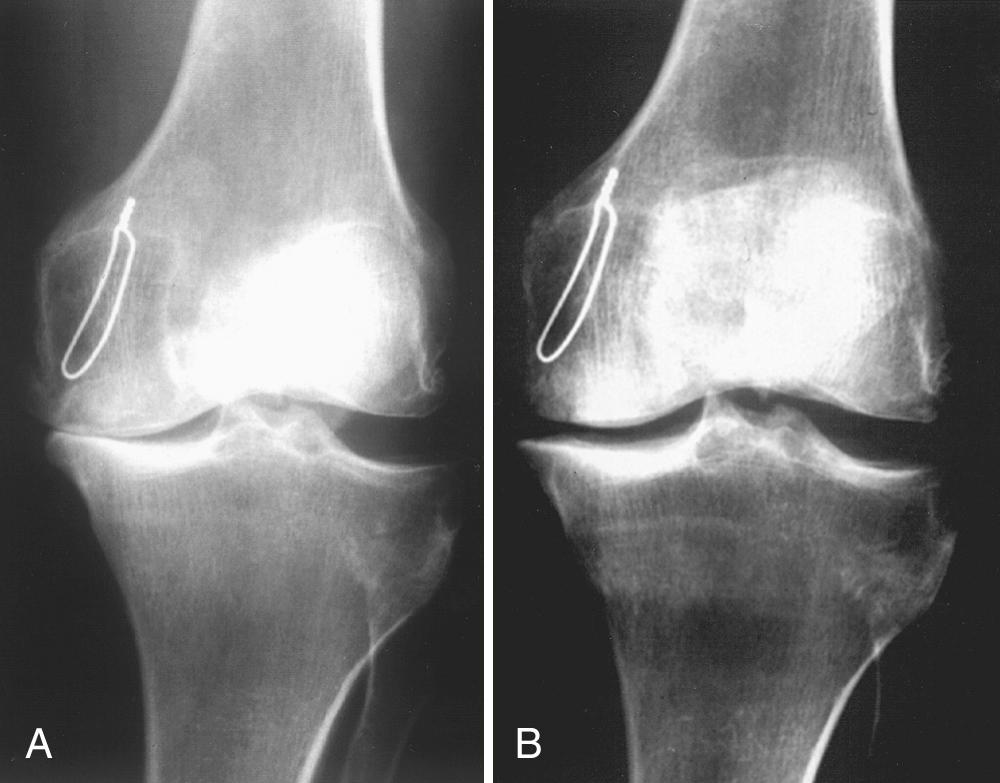
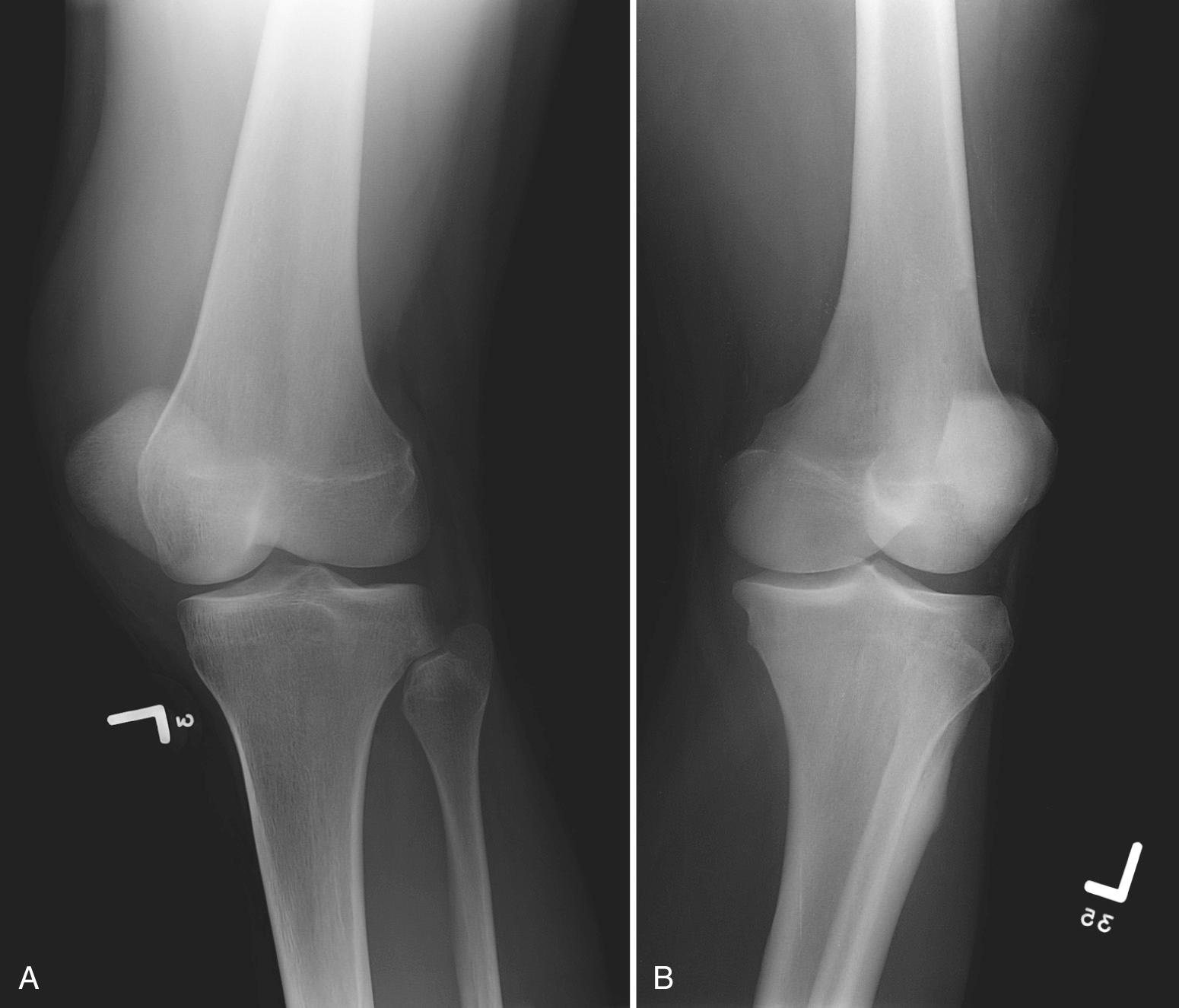
The flexed, PA weight-bearing (Rosenberg) view is a modified tunnel view. It is obtained with the patient standing and the knee flexed 45 degrees. The patellae should touch the film cassette. The x-ray beam is centered at the level of the inferior pole of the patella and is directed 10 degrees caudad. It captures the joint space at the posterior aspect of the femorotibial joint. This view is valuable for evaluating arthritis. It detects joint space narrowing because of cartilage loss that often goes unappreciated or underestimated on a conventional AP weight-bearing view ( Fig. 5.6A and B ). Comparisons of intraoperative and radiographic findings demonstrate that the flexed PA weight-bearing view has greater accuracy, sensitivity, and specificity than the conventional extension weight-bearing radiograph.

Oblique radiographs complement a routine examination. Occult fractures and tibiofibular arthritis may be more easily detected with oblique views than with routine AP radiographs. Bilateral oblique views are obtained at 45 degrees of internal and external rotation, with the patient supine, the affected knee extended, and the cassette behind the knee. The x-ray beam should be directed 5 degrees cephalad. Views should demonstrate the patella, femoral condyles, tibial plateaus, and fibula. In external rotation the tibia and fibula are superimposed on each other. With internal rotation there is less superimposition between the tibia and fibula ( Fig. 5.7A and B ).
Various stress views have been described for evaluation of instability and include valgus and varus stress radiographs for evaluation of the collateral ligaments and anterior drawer stress radiographs for evaluation of the anterior cruciate ligament (ACL). These require use of a mechanical stress device or lead gloves worn by the x-ray technologist and manually stress the knee joint. In current clinical practice these views are seldom ordered because MRI is considered the gold standard for evaluation of internal derangement and stress views often need to be performed with local anesthesia for pain control.
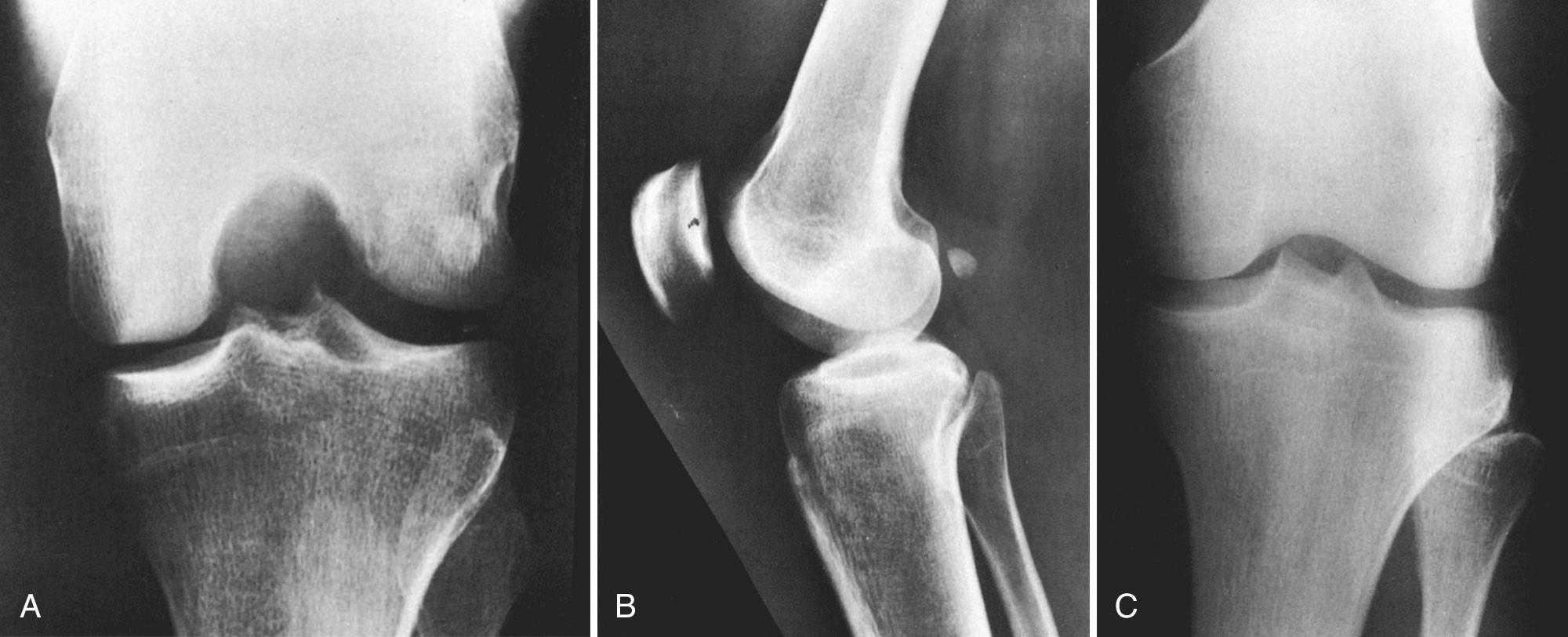
Two sesamoid bones commonly identified on knee radiographs are the fabella and the cyamella. The fabella is located within the lateral head of the gastrocnemius. It overlies the lateral femoral condyle on the frontal view and sits posterior to the distal femur on the lateral view. The cyamella lies within the popliteus tendon. On a frontal radiograph it may be found at the insertion of the popliteus in the notch of the lateral femoral condyle ( Fig. 5.8A to C ).
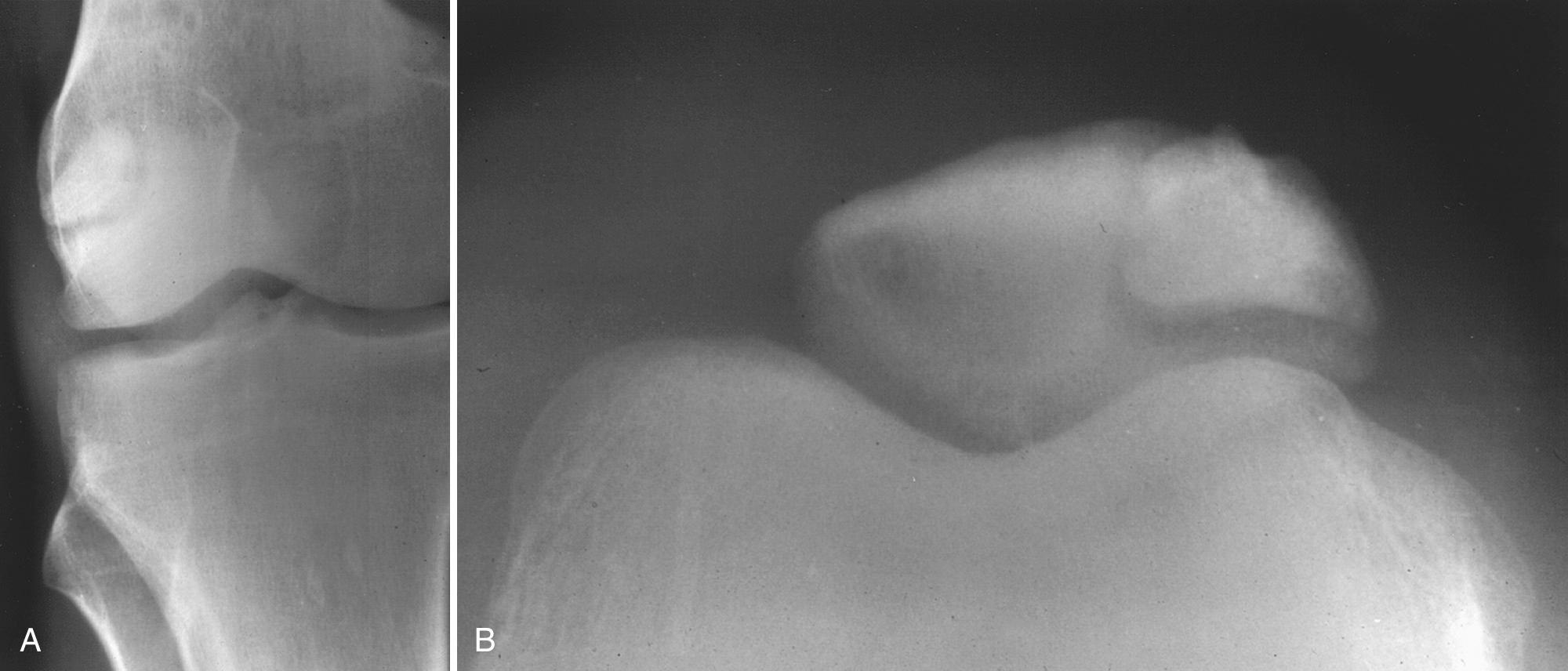
Normal variants also occur in the patella, which can have two or more osseous centers, referred to as a bipartite or multipartite patella ( Fig. 5.9A and B ). A bipartite patella is the more common variant, seen in 1% of the population. It is bilateral 50% of the time. The smaller pieces of the patella are located superolaterally and should fit neatly together like pieces of a jigsaw puzzle. The width of a bipartite patella is usually greater than that of the contralateral patella when assessed on a tangential axial view. MRI depicts intact cartilage overlying a bipartite patella, whereas a fracture displays disrupted osteochondral integrity. These features help to dismiss the suspicion of a fracture. Rarely (<2% of the time), a bipartite patella can be symptomatic. MRI of the knee may demonstrate bone marrow edema on one or both sides of the synchondrosis.
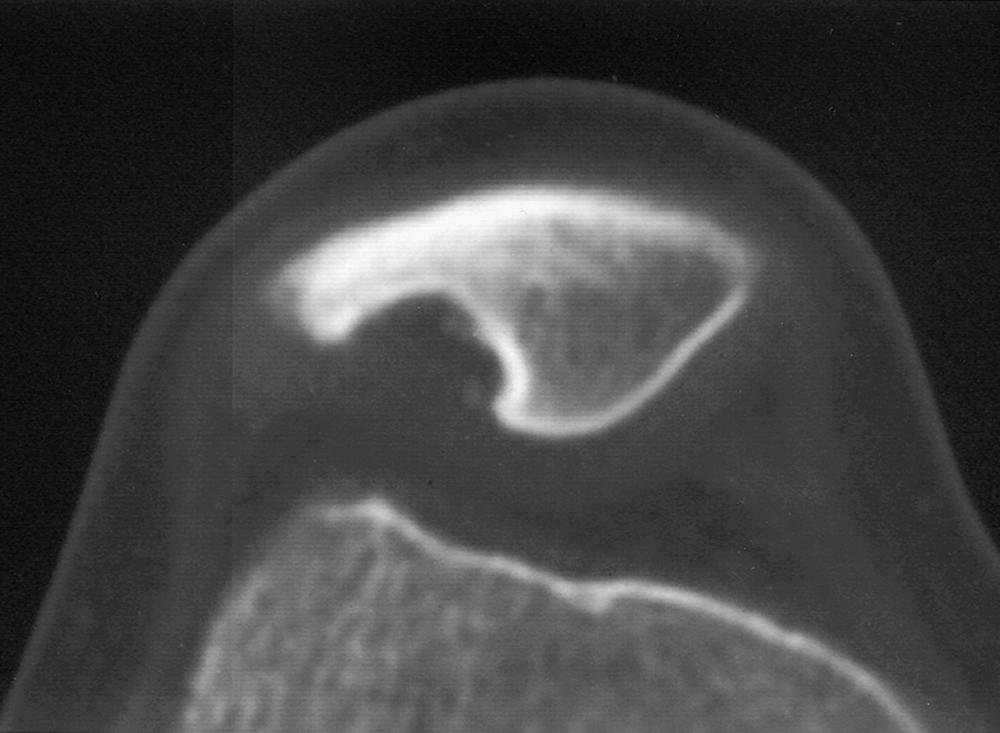
A dorsal defect of the patella is another anatomic variant, usually detected incidentally. It appears as a lucent area of the superolateral patella ( Fig. 5.10 ). Pathologically the lesion is composed of fibrous tissue and spicules of bone. This uncommon entity is seen in children and typically fills in with normal or sclerotic bone in adulthood.
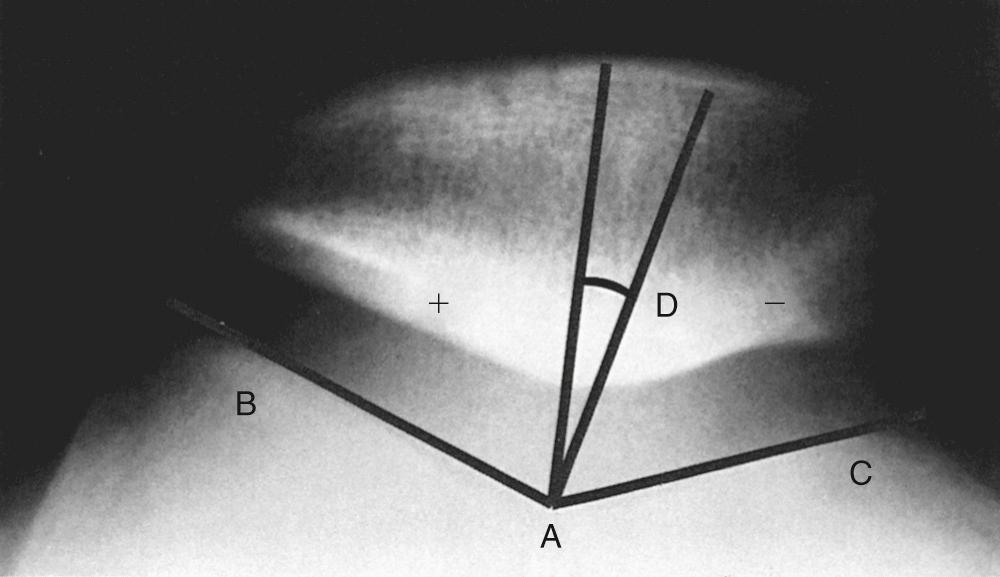
Merchant views can evaluate patellofemoral malalignment, which can be quantified with the sulcus and congruence angles. The sulcus angle is formed by drawing lines outward from the deepest portion of the trochlear sulcus to the tops of the femoral condyles. The angle normally measures 138 degrees (±6 degrees). A shallow sulcus greater than 144 degrees is associated with recurrent patellar dislocation.
The congruence angle provides an index of subluxation. To measure it, the sulcus angle is bisected to create a reference line. An additional line is then drawn from the deepest portion of the trochlear sulcus to the patellar apex. The angle formed between this line and the reference line is the congruence angle. If the patellar apex falls lateral to the reference line, then the value of the congruence angle is positive. If the apex falls medial to the reference line, then the value of the congruence angle is negative. The normal congruence angle is 6 degrees (±11 degrees) ( Fig. 5.11 ).
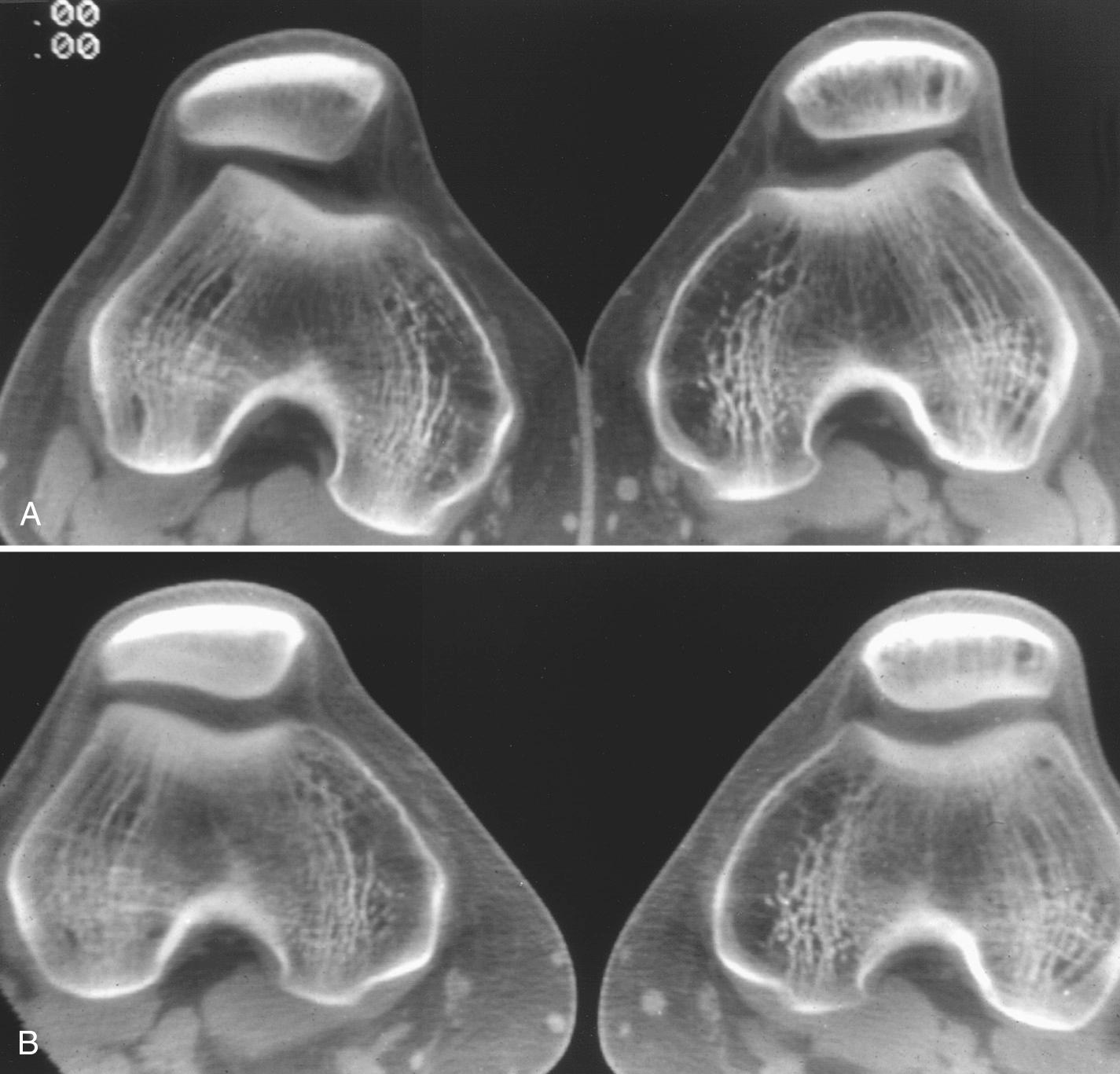
Patellar tilt is another measure of patellofemoral alignment. It is measured by the angle formed between a horizontal line and a line drawn between the medial and lateral corners of the patella. In a study performed by Grelsamer and colleagues the mean tilt angle of a group of patients with signs and symptoms suggesting patellofemoral malalignment was 12 degrees (±6 degrees); in a similar group of control subjects it was 2 degrees (±2 degrees). Tilting of 5 degrees was taken to be the limit of normal. It is noteworthy that in the Grelsamer study, the knee was held in 30 degrees of flexion, rather than 45 degrees of flexion in the normal Merchant view. Other imaging techniques (CT scans performed at various degrees of flexion) are sometimes necessary to detect patients with subtle or transient lateral patellar subluxation ( Fig. 5.12A and B ).
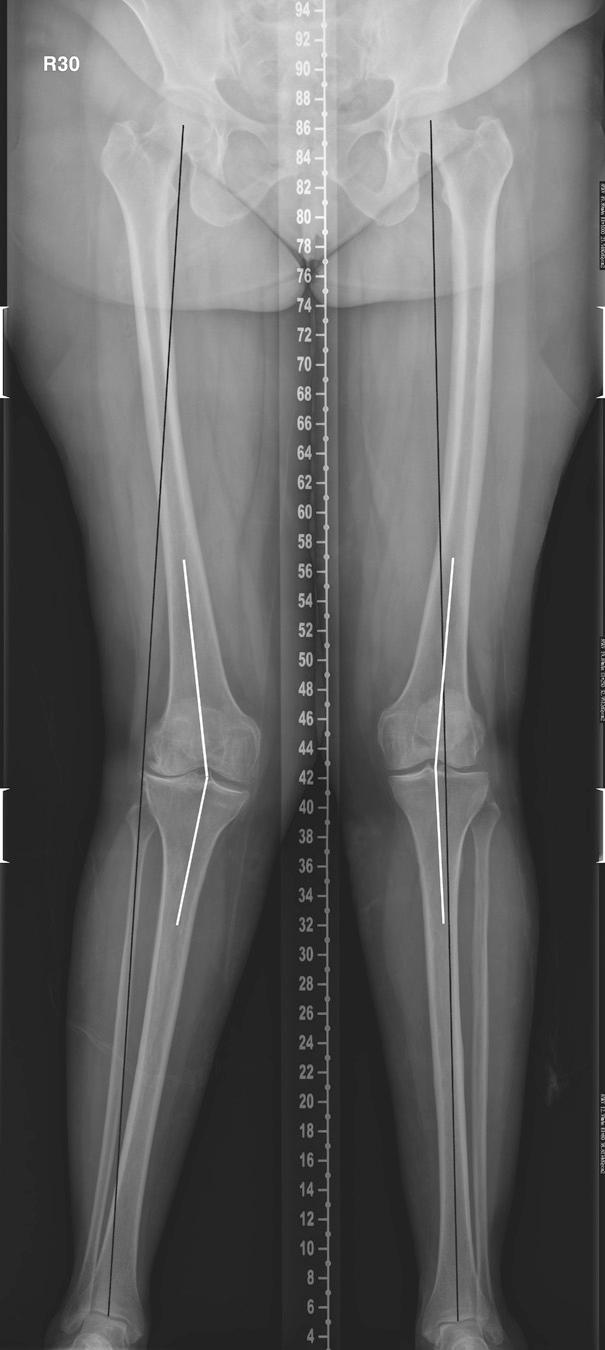
Short-standing frontal views (weight-bearing AP or Rosenberg) are typically sufficient for measuring the anatomic axis of the knee joint. The normal anatomic axis is 6 to 7 degrees of valgus angulation. If the exact quantitative measurement of the mechanical axis is required, then a long-standing frontal view of the lower extremity may be performed. The mechanical axis (weight-bearing axis) of the lower extremity is defined by a line drawn from the center of the femoral head to the center of the tibial plafond. In the normal setting this line should pass through the inner aspect of the medial compartment of the knee joint. If genu valgus is excessive, then the mechanical axis will shift laterally. A medially shifted mechanical axis indicates genu varus. Knowledge of the mechanical axis and how it relates to the anatomic axis is important in evaluating patients who are about to undergo or have undergone total knee arthroplasty and/or revision arthroplasty. It is also helpful in evaluating patients with posttraumatic deformities, malalignment, or limb length discrepancies.
Obtaining long-standing radiographs requires a long cassette. If a long cassette is not available, a CT scanogram can be obtained. CT scanning to obtain the mechanical axis is not advocated by the authors because it is not weight bearing, does not provide functional information, and may fail to take account of ligamentous laxity. In addition, CT scanograms entail higher radiation dosage exposure compared with conventional radiographs ( Fig. 5.13 ).
Radiographic arthrography entails intra-articular injection of x-ray dye, typically an iodine-based product. Arthrography has many uses, including confirming placement before joint aspiration. Commonly, after radiographs or real-time ultrasound confirm dye placement within the joint space, a CT or MRI is performed to better evaluate meniscal or articular cartilage pathology and or component loosening ( Fig. 5.14 ).

Radiography necessitates exposing the patient to ionizing radiation. The associated risk is low, particularly in the extremities. Special consideration should be given to children and young adults to minimize their exposure.
CT provides detailed information about osseous structures and generally functions as a problem-solving modality once the limits of radiography have been reached. Specialized knee applications include evaluation of complex trauma, such as tibial plateau fractures, fracture healing, and joint loose bodies. CT is used with increasing frequency for preoperative joint replacement planning, arthroplasty complications, and revision arthroplasty preparation. Extensor mechanism and patellofemoral joint evaluation in the setting of knee pain has also been reported.
CT arthrography may be requested to evaluate menisci and/or articular cartilage when a patient is unable to undergo an MRI. This situation is commonly encountered in patients with claustrophobia or MRI-contraindicated metallic devices, such as pacemakers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here