Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intraoperative parathyroid hormone monitoring (IPM) has been used since the 1990s to guide the excision of abnormal parathyroid glands in patients with sporadic primary hyperparathyroidism (SPHPT). Currently, many high-volume parathyroid surgeons use IPM, selectively or routinely, to guide parathyroidectomy in patients with primary hyperparathyroidism (PHPT).
This surgical adjunct has helped change the operative approach to parathyroidectomy from the traditional bilateral neck exploration (BNE) (which had visualization of all parathyroids and excision of enlarged glands based on the surgeon’s subjective judgment of gland size) to a minimally invasive parathyroidectomy with removal of only the hypersecreting gland(s); this helps preserve all normally functioning tissue. This less invasive approach to parathyroidectomy, safely achieved with the help of IPM, is not only as successful as BNE but also allows for surgery in an ambulatory setting with less neck dissection, often with fewer glands excised, shorter operative time, and fewer postoperative complications (see Chapter 56 , Standard Bilateral Parathyroid Exploration).
The goals of this chapter are the following: (1) to discuss the practical issues regarding the use of intraoperative PTH monitoring during parathyroidectomy, (2) to suggest guidelines for interpreting intraoperative PTH levels based on the available published data and the authors’ personal experiences, and (3) to give an overview of the current controversies associated with the use of this surgical adjunct.
Since the 1990s, a significant volume of information has been gleaned regarding the application of this methodology as well as its influence on the conduct of parathyroidectomy in various parathyroid disorders. The basic premise justifying the use of such a test resides in the ability to rapidly measure the hyperfunction of abnormal parathyroid tissue in the operating room.
The discovery of parathyroid hormone (PTH) and the subsequent development of assays to accurately measure levels in both the physiologic and pathologic state has been earmarked by a number of major events, which together have led to the current application of the intraoperative measurement of PTH in managing surgical parathyroid disease. In 1923, a general surgeon, A.M. Hanson, was the first to demonstrate presence of the hormone. The extract of the hormone, which he developed from bovine parathyroid glands, was used successfully in treating experimental tetany. Nearly 3½ decades after its initial discovery, two groups working independently were able to further characterize this extract as PTH. Rasmussen and Craig from the Rockefeller Institute in New York, as well as G.D. Aurbach in Boston, extracted a stable parathyroid polypeptide and demonstrated that the hypercalcemic properties previously described resided in a single hormonal substance. Berson and Yalow, working at the Bronx VA Hospital in 1963, in collaboration with Aurbach and John Potts from the National Institutes of Health (NIH), described a radioimmunoassay for PTH. In an effort to raise an antibody that recognized human PTH specifically, Eric Reiss and Janet Canterbury, working at the Michael Reese Hospital in Chicago in 1965, harvested bovine parathyroid glands and injected the extract into various experimental animals. These early efforts were unsuccessful. However, after many trials, an antibody to bovine parathyroid was obtained that had a high affinity for human PTH in experimental chickens. Using this antibody, these investigators developed an assay with satisfactory identification of PTH concentrations in humans.
In 1988, Nussbaum et al. modified the original immunoradiometric assay (IRMA) by increasing the temperature of incubation and employing a kinetic enhancer; these changes decreased the turnover time to approximately 15 minutes. In this initial report, these investigators described the first use of PTH monitoring during parathyroidectomy, although the patients in their series underwent BNE, and PTH was measured postoperatively. Although the reporting of this clinical experience appeared to be of interest clinically, it was not readily accepted as an alternative to the existing practice of conventional BNE, especially given that operative success rates in the treatment of PHPT were approximately 95%. Flentje et al. modified the PTH assay by decreasing the laboratory turnaround time to 1 hour and attempted to use it perioperatively in 1990. They described PTH level changes during parathyroidectomy and, although measured after the operation, it was clear that PTH levels dropped after excision of the abnormal parathyroid gland. In 1990, Chapuis et al. reported on their series of 13 patients in whom the PTH dropped > 70% in 20 minutes after parathyroidectomy by using the IRMA for intraoperative PTH measurement.
An early advocate of the use of IPM in the United States was Dr. George Irvin from the University of Miami. Irvin’s initial venture into adding the intraoperative assessment of PTH levels to his surgical practice, by his own admission, came from an operative failure in the early 1990s. After the initial failed parathyroidectomy in this patient, a reexploration was performed at which time a contralateral thyroid lobectomy for an occult second intrathyroidal parathyroid adenoma was carried out. Using a modification of the technique described by Nussbaum, Irvin was able to demonstrate a rapid decline in PTH levels measured intraoperatively after removal of the second parathyroid adenoma. In 1991, Irvin et al. described for the first time a series of 21 patients who had their parathyroidectomies guided exclusively by IPM using an immunoradioisotopic method.
With George Irvin’s help in 1996, this rapid assay was converted to an immunochemiluminescence method, and the “quick” PTH assay became commercially available for intraoperative use, which is still the methodology used today. After Irvin’s initial publication, which provided impressive clinical justification for the implementation of this methodology, the literature has been replete with increasing reports describing numerous investigations on the use of intraoperative PTH measurement for parathyroid exploration. These pioneers, and especially Dr. Irvin, have changed the surgical management of PHPT as IPM-guided parathyroidectomy has become the approach of choice of many specialized surgeons in the treatment of parathyroid disease.
IPM has been extensively described and studied in patients with SPHPT, whereas its use in patients with secondary and tertiary hyperparathyroidism as well as in multiple endocrine neoplasia (MEN) requires further investigation as the studies are limited. Postoperative long-term follow-up of these patients to determine which is the optimal intraoperative criteria and protocol to predict cure in these distinct forms of HPT is necessary to establish the use of IPM in these patients. IPM can be used to guide parathyroidectomy in isolated familial hyperparathyroidism (HPT) with an acceptable accuracy. However, the results of this surgical adjunct in predicting operative success in patients with parathyroid cancer are not as encouraging. The data and suggested guidelines for the use of IPM methodology discussed in this chapter are best applied for treatment of only SPHPT.
The authors use the information of IPM to do the following:
Confirm complete excision of all hyperfunctioning parathyroid tissue before the operative procedure is finished, without visualization of normally functioning parathyroid glands.
Point out the presence of additional hypersecreting tissue by an insufficient PTH drop, indicating that further neck exploration is required in an attempt to prevent operative failure.
Differentiate parathyroid from nonparathyroid tissues by using biochemical fine-needle aspiration (FNA), to be described in detail later in this chapter.
Lateralize the side of the neck harboring the most hypersecreting parathyroid gland by performing differential jugular venous sampling in patients with negative or equivocal preoperative localization studies.
The accuracy of this adjunct in correctly guiding the surgeon to the desired outcome (complete excision of all hyperfunctioning glands and achievement of postoperative eucalcemia) is strongly related to the criteria used to predict such an outcome. Intraoperative PTH assays only measure PTH levels at specific time points during the procedure as determined by the surgeon. It is therefore essential to understand hormone dynamics during parathyroidectomy to properly request blood sampling during the procedure.
A peripheral access with a 16-gauge catheter or arterial line for blood sampling during the procedure is obtained either in the holding area or in the operating room. It is important to ensure that blood can be drawn after access is obtained, especially after the patient’s arms are tucked in; positioning may affect satisfactory sampling from an adequately placed line. This access is kept open with saline infusion throughout the procedure, and an intravenous (IV) extension is used to give the anesthesiologist access to the tubing for blood collection at times requested by the surgeon. It is important to instruct the anesthesia team about discarding 10 cc of blood with saline to avoid sample dilution potentially leading to falsely lower PTH levels. Three to 5 cc of whole blood are collected for PTH measurement and are placed in an ethylenediaminetetraacetic acid (EDTA) tube at specific times, including the following:
in the operating room before the skin incision is made (preincision),
when all blood supply to the suspicious gland is ligated (preexcision or time zero),
5 minutes,
10 minutes, and
occasionally, 20 minutes after excision of the suspected abnormal gland.
When peripheral PTH values drop > 50% from the highest, either preincision or preexcision levels (10 minutes after removal of all abnormal parathyroid glands), postoperative normal or low calcium levels are predicted with excellent accuracy. While waiting for PTH results to be reported by the laboratory (which can range between 8 and 15 minutes depending on the assay used), the surgeon may proceed with closure of the cervical incision, avoiding manipulation of the remaining parathyroid glands in an effort to minimize the chance of falsely elevating PTH levels, which could result in a delay in hormone drop. Although the 10-minute PTH level fall of > 50% is the definitive measurement of postoperative success, the PTH fall of > 50% at the 5-minute interval also will be seen in the majority of surgically cured patients. Given this, some surgeons prefer to check a 5-minute level, which if reduced > 50% allows the termination of the procedure without further neck exploration or visualization of the remaining, normally-secreting parathyroid glands; this allows the patient to be extubated and sent to the recovery room earlier. By this time, the 10-minute PTH level is reported, confirming operative success. Conversely, if the criterion is not met in the 10-minute sample, the neck is reexplored and the protocol for blood sampling is repeated for each additional excised gland until all hypersecreting tissue is removed as indicated by meeting the criteria.
In cases where the PTH percent drop is not quite sufficient in 10 minutes, but it is significant (~40%), a 20-minute sample can be collected for PTH measurement before the neck is reexplored. However, if there is no significant PTH drop in 5 or 10 minutes, the cervical incision should be reopened promptly to identify and excise additional hypersecreting tissue.
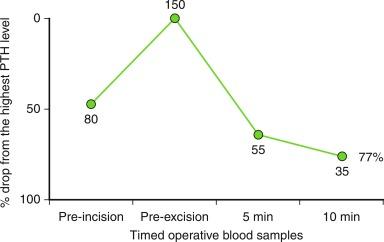
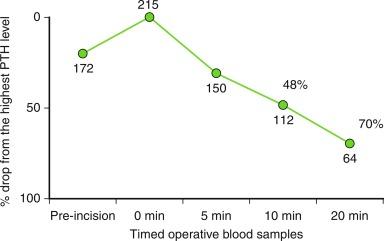
Adequate PTH drop after excision of a suspicious gland. Figure 59.1 shows the hormone dynamic after excision of a single hypersecreting parathyroid gland resulting in adequate PTH drop and operative success. When such a PTH fall is seen, the surgeon can proceed with closure of the cervical incision without visualization or biopsy of the remaining normally secreting parathyroid glands. Frozen section of the excised parathyroid gland is also not necessary because parathyroid tissue excision is confirmed by the adequate PTH drop.
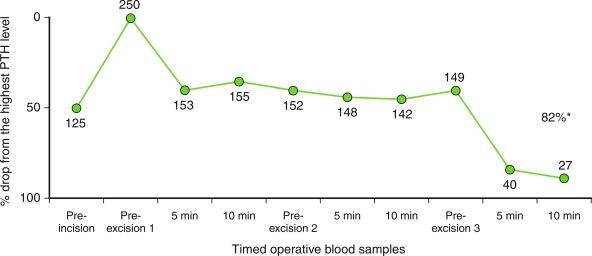
Insufficient PTH drop after excision of a suspicious gland pointing out the presence of multiglandular disease. Figure 59.2 shows the hormone dynamics in a patient with multiglandular disease. After excision of the first parathyroid gland, the PTH level did not drop adequately, guiding the surgeon to further explore the cervical area for additional hyperfunctioning tissue. Note that the same protocol for blood sampling is repeated for each excised suspicious tissue until the IPM criterion is met. The PTH level selected to calculate a sufficient PTH drop after an extensive neck dissection should be the last preexcision level or the preincision level, whichever is greater.
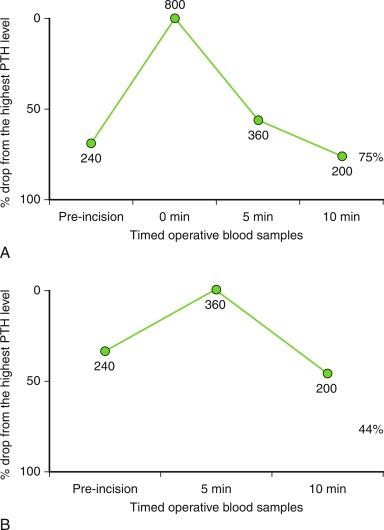
Elevation of PTH level at the preexcision/0-minute sample. Figure 59.3 , A , shows the intraoperative hormone dynamic of a patient in whom the manipulation of an abnormal gland during dissection increased the PTH level significantly in the preexcision/0-minute sample. In patients like this, which are seen in about 16% of cases, the importance of collecting both samples (preincision and preexcision/0 minute) to calculate the PTH decline accurately is evident. Figure 59.3 , B , shows the same patient’s PTH levels and the consequence of not collecting the 0-minute sample leading to a falsely inadequate PTH drop. In such patients, by not registering the peak of the PTH level during manipulation of the parathyroid gland, this apparent insufficient PTH drop can lead to unnecessary BNE. The same issue is possible if the preexcision/0-minute sample is obtained too early in the dissection, which will also result in missing the peak of PTH level.
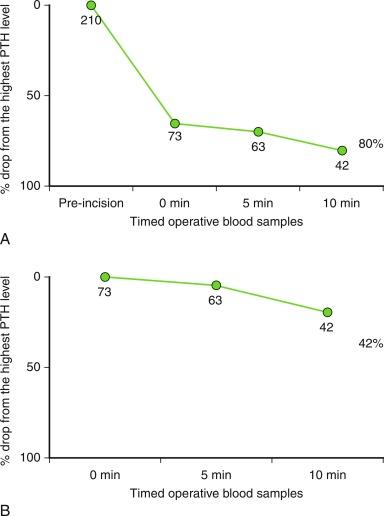
Sufficient PTH drop on the preexcision/0-minute level. Figure 59.4 , A , shows the intraoperative PTH dynamics of a patient in whom the PTH level already met the criterion at the 0-minute sample. This finding indicates that the parathyroid gland’s main blood supply was ligated early in the dissection and the PTH has already dropped. In this case, it is clear by the preexcision/0-minute sample that this is the only hypersecreting parathyroid gland, thereby allowing the surgeon to finish the procedure safely. Figure 59.4 , B, demonstrates that in cases where the PTH level has already declined significantly in the 0-minute sample (15% of the cases), not measuring the preincision sample might result in an apparent insufficient PTH drop, potentially leading to unnecessary further neck exploration.
Delay of intraoperative PTH drop after successful excision of a single hypersecreting parathyroid gland . Figure 59.5 shows the intraoperative hormone dynamics in a patient with a delayed PTH drop after excision of a single hypersecreting parathyroid gland. In these situations, the PTH declines significantly but does not meet the criteria in the 10-minute sample; a 20-minute value might be helpful in preventing further neck exploration. The 20-minute sample might also be useful to surgeons who require a drop in PTH level > 50% and a return to normal range to predict operative success. When the PTH level is very high in the 0-minute sample, it is biochemically impossible for the PTH to return to normal limits in a period of 10 minutes; however, it often occurs 20 minutes after excision of all hypersecreting parathyroid glands ( Box 59.1 and Figure 59.6 ). This scenario may be encountered as well in a patient with preexisting renal insufficiency, whereby metabolic changes can result in a delayed decline in PTH levels
Baseline preincision sample.
Baseline preexcision sample, taken just before the fully dissected adenoma’s vessel is ligated and adenoma is resected.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here