Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In this chapter we review a practical approach to intraoperative frozen section and highlight the role of the pathologist in guiding intraoperative decision making. For convenience sake, we use the term “frozen section,” but at the onset we wish to point out that the pathologist’s role extends beyond looking at slides to, obviously, careful gross inspection which dictates not only areas to be selected for evaluation under the microscope but also tissue to be taken for special studies that are increasingly indicated in modern medicine. The intraoperative consultation (IOC) also often includes advising the surgeon, particularly when an unusual neoplasm is encountered. The pathologist needs to be familiar with the natural history of the disease and the surgical approach that may be most appropriate.
Frozen section in gynecologic surgery has primarily the following indications:
To determine the nature of a disease process
To assess tumor extent and guide further surgical management
To evaluate specimen margins
To ensure that adequate diagnostic tissue is present
To plan for ancillary studies
The first three dominate in the field of gynecologic oncology. Although ovarian tumors represent the most common indication for frozen section (36 %) (Scurry and Sumithran, 1989), the majority are from other areas in the female genital tract. This chapter discusses the use of the technique in the uterus, vagina, and vulva with an emphasis on common problems and pitfalls.
Overall, frozen section accuracy in gynecologic pathology ranges from 91 % to 97 % (Acs, 2002). To ensure a timely and accurate intraoperative opinion, effective communication between surgeon and pathologist is critical (Kumar et al, 2012). Ideally, relevant clinical information, including previous history, serum markers, imaging studies, and antecedent pathology reports, should be provided. In addition, a review of slides from prior specimens at other institutions should be carried out prior to the operation. In exceptional circumstances, it may be helpful to review prior in-house slides in the intraoperative setting. Careful gross examination of large specimens is essential in guiding the selection of sections taken and sometimes may preclude the need for a frozen section. This includes serial sectioning of masses and careful inspection of each slice looking for aberrant gross characteristics. While some authors suggest better accuracy when the frozen section is interpreted by a gynecologic pathologist, in most centers experienced general surgical pathologists are equally capable. Request for a second opinion is prudent if the pathologist is unsure of the correct diagnosis because deferring the diagnosis to permanent section potentially may put the patient at risk.
The incidence of ectopic pregnancy is increasing and is a major cause of morbidity and mortality in reproductive-age women, accounting for slightly less than 10 % of pregnancy-related deaths in the first trimester (Lipscomb et al, 2000; Centers for Disease Control and Prevention, 1995). The most reliable way to exclude an ectopic pregnancy is to histologically confirm an intrauterine pregnancy because noninvasive tests have a 40 % false-positive rate (Barnhart et al, 2002). Most specimens submitted for frozen section are endometrial curettages; however, the use of Pipelle biopsy sampling has recently been explored. The sensitivity of the latter is low compared to a curettage which has up to 87 % sensitivity and 100 % specificity, depending on the study (Barnhart et al, 2002; Heller et al, 2000; Spandorfer et al, 1996).
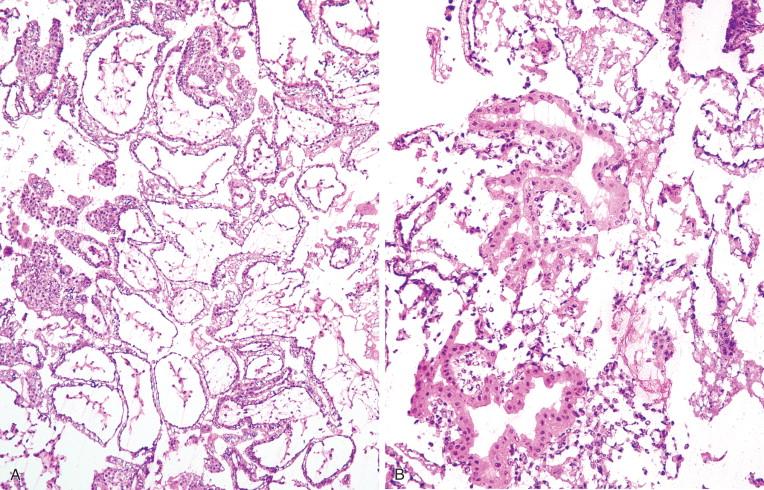
When a “rule out ectopic” specimen is received, the first step is to evaluate the amount of tissue that appears to be villous ( Figure 18-1A ). There is no rule regarding the precise manner by which the tissue should be evaluated grossly or how material should be sampled for frozen section evaluation. Several methods can be utilized, including “floating” the specimen in a Petri dish with saline, looking for “spongy” tissue (which corresponds to chorionic villi) with the naked eye, or alternatively using a dissecting microscope (stereomicroscope). Depending on the pathologist’s experience, visual verification can be sufficient. However, these methods do not allow for a permanent record of the findings (Spandorfer et al, 1996), and confirmation by histology is always necessary. Some pathologists may elect to freeze the material as a first option. If the tissue is abundant and villi are visually suspected, they should be selected for frozen section. Blood generally should be avoided except if it has a granular or firm texture because this may contain diagnostic tissue (Baergen, 2005). If the tissue is scant, it should be entirely submitted for microscopic evaluation. Because freezing artifact is common and may hinder correct evaluation, a decision to defer to rapid permanent (“rush”) processing may be an option after discussion with the clinician.
Histologic findings diagnostic of intrauterine pregnancy are:
Chorionic villi
Fetal tissue
Syncytiotrophoblast (typically present within blood)
Implantation site
Recognition of the first two is generally straightforward, but confident appreciation of the latter two may be more challenging. Even though the literature reports a very low false-positive rate of villous identification, freezing- related artifact may result in a false-positive diagnosis. Additionally, villi, if scant, may be overlooked or erroneously considered present if mimicked to a degree by superficial fragments of endometrium or endocervix. Such fragments, if tangentially sectioned, may appear “blown up” due to freezing artifact, as well as to pregnancy-related changes ( Figure 18-1B ). Fibrin deposition and intermediate trophoblast replacing the walls of large vessels should be seen in order to establish the diagnosis of implantation site. Intermediate trophoblastic cells interspersed between decidual cells may be an additional helpful finding. The presence of either decidua or large blood vessels with hemorrhage is not diagnostic of intrauterine pregnancy. On the other hand, the finding of syncytiotrophoblastic cells alone does not exclude an ectopic cornual or interstitial tubal pregnancy. Exceedingly rare heterotopic pregnancy (simultaneous intrauterine and ectopic) may occur. Villi can be seen in frozen section, but in this scenario an ectopic pregnancy is not excluded (Gruber et al, 1997). Surface endometrial cells may be difficult to differentiate from syncytiotrophoblastic cells especially when tissue is scant ( Figure 18-1B ). If this is the only finding, it is best to defer to rapid permanent processing because the use of immunohistochemistry may be needed. Another potential pitfall is the misinterpretation of immature chorionic villi as molar villi causing undue patient anxiety (Heller et al, 2000).
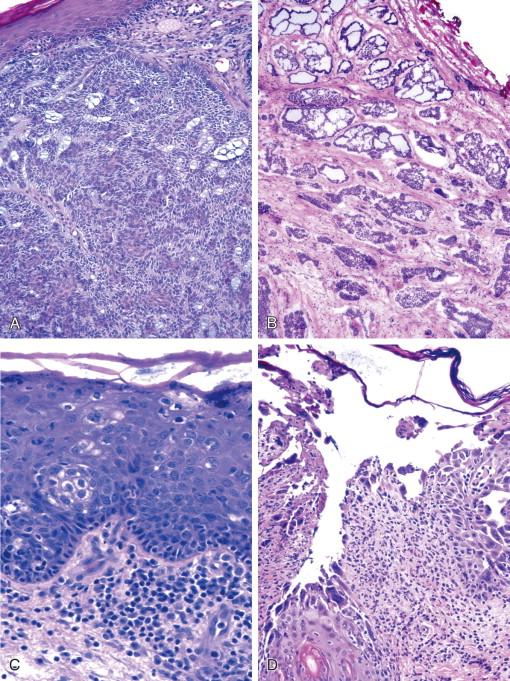
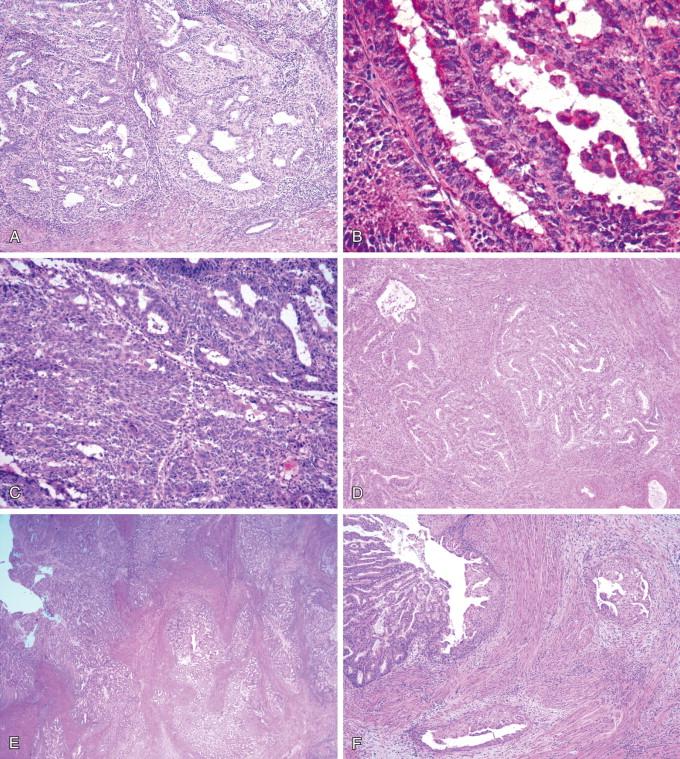
Intraoperative evaluation of vulvar specimens is an infrequent request, with issues relating to squamous cell carcinoma accounting for the great majority of cases ( Figure 18-2A ). The most common indications are:
Margin evaluation
To prove the multifocal nature of disease (Rodolakis et al, 2003)
Lymph node status (discussed below), less often for basal cell carcinoma or other neoplasms (Smith-Zagone and Schwartz, 2005).
A compelling argument for frozen section examination of margins is the significant recurrence rate for squamous carcinoma (between 30 % and 67 %).
Challenges in the differential diagnosis in squamous cell carcinoma include:
Tangentially sectioned normal squamous epithelium
Involvement of adnexal structures by in situ neoplasia
Frequent bulbous expansion at the base of in situ carcinoma (often misdiagnosed as early invasion)
Associated inflammation
Paget disease
Squamous eddies in irritated seborrheic keratosis
Melanocytic proliferations
Sebaceous carcinoma
Pseudoepitheliomatous hyperplasia associated with granular cell tumor
Herpetic infection
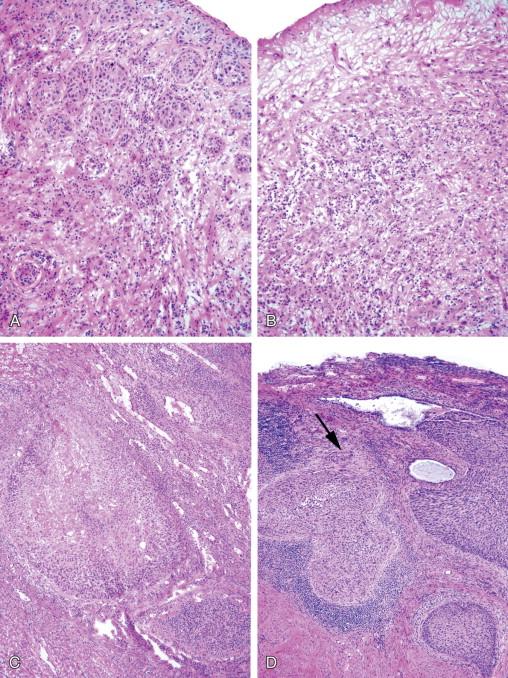
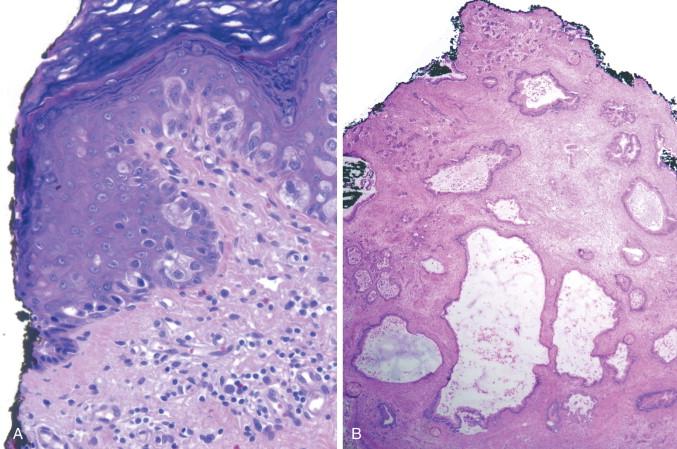
Careful attention should be paid to ensure proper orientation of the specimen. Adnexal involvement and bulbous expansion are distinguished from invasion by their smooth contours and lack of typical keratinization seen in early invasive carcinoma. Chronic inflammation often accompanies in situ or early invasive squamous cell carcinoma and may obscure the epithelial-stromal interface ( Figure 18-3A, B ). Paget disease may closely mimic the appearance of squamous cell carcinoma in situ because the pale quality of the mucinous cytoplasm cannot be appreciated in a frozen section. However, the distribution of the cells within the epidermis is often discontinuous at the base (pagetoid) in contrast to a usually continuous presence of abnormal cells at the base in carcinoma. Furthermore, there is usually full-thickness involvement of the epidermis in carcinoma. A modified periodic acid–Schiff (PAS) stain may be helpful in highlighting intracellular mucin in Paget disease ( Figure 18-4A ) (Fishman et al, 1998). Seborrheic keratosis shows a uniform proliferation of squamous cells without significant cytologic atypia. Although squamous eddies may be misinterpreted as the keratinization of carcinoma, they are always intraepidermal with good preservation of the basal cell layer. Melanocytic proliferations may be difficult to distinguish from squamous carcinoma because melanin pigment may be incorporated within squamous cells, and both can involve the full thickness of the epidermis and may show a spindled growth. However, malignant melanoma often shows pagetoid spread, as well as a nested appearance at the epidermal-dermal junction at the periphery of the neoplasm. Sebaceous carcinoma, if poorly differentiated, may closely mimic squamous cell carcinoma ( Figure 18-2C ). Usually an invasive tumor has a lobulated architecture, and at least some cells may show foamy cytoplasm due to intracytoplasmic fat which can be highlighted by oil red O or Sudan IV stains (Callahan et al, 2004). Lastly, it is important to keep in mind that a granular cell tumor may occur in the vulva and may be associated with prominent squamous hyperplasia (pseudoepitheliomatous). In this instance it may mimic squamous cell carcinoma if the pathologist overlooks the underlying neoplastic proliferation or the biopsy is not deep enough to include the tumor (Lee et al, 2003). Herpes can involve the vulva, especially in immunocompromised patients, often presenting with painful ulcers or vesicles. The cytopathic features include a striking atypical appearance of the squamous cells. In these instances, blisters are commonly seen, and close scrutiny of the infected squamous cells, especially if pilosebaceous units are present, show multinucleation, as well as ground-glass chromatin and intranuclear inclusions (Frimer et al, 2011; Strehl et al, 2012) ( Figure 18-2D ).
Although, as noted above, most frozen section issues at this site revolve around squamous cell carcinoma, some other issues arise, most of them related to rarer carcinomas or malignant melanoma. In basal cell carcinoma, an important issue is reporting lateral margins. Not only unequivocal margins should be reported, but also those that are close, defined as a tumor coming to within one high-power field of the margin. The recurrence rate in the first instance is approximately 33 % but decreases to 12 % in the latter scenario (Smith-Zagone and Schwartz, 2005). Mimics that should be considered when examining a frozen section to rule out a basal cell carcinoma include tangential sectioning of a hair follicle because at its edge it may show palisading and hyperchromasia. However, the latter lacks the cleftlike space around the tumor nests, as well as the mitoses and apoptoses often seen in basal cell carcinoma. Toluidine blue may be helpful in this situation because it stains the inner root sheath of the hair follicle deep blue (Smith-Zagone and Schwartz, 2005). In equivocal cases, deeper sections should be obtained. A rare mimic of basal cell carcinoma is sebaceous carcinoma, particularly if poorly differentiated. Oil red O or Sudan IV may be helpful in demonstrating fat within the neoplastic cells. Rarely, the pathologist may be called upon to assess a mass in the Bartholin gland region, and standard criteria should be applied in distinguishing the common inflammatory lesions of Bartholin gland from the neoplasms that may arise from it ( Figure 18-2B ).
Intraoperative frozen section analysis has been used to determine margin status in Paget disease (Kodama et al, 1995; Stacy et al, 1986), but its utility is controversial because the disease is frequently multifocal and extends beyond areas thought to be abnormal on gross examination (Shaco-Levy et al, 2010a; Shaco-Levy et al, 2010b). A modified PAS stain has been used to increase the accuracy of identification of Paget cells at margins (Fishman et al, 1998). While studies report the presence of microscopically positive margins to be a frequent finding, there is no correlation between positive margins and local recurrence (Black et al, 2007; Curtin et al, 1990; Fishman et al, 1995; Parker et al, 2000). It is important to keep in mind that Paget disease and melanoma show the same pattern of distribution in the epidermis, and these two cell types may very closely mimic each other. Thus the routine use of frozen section for margins in Paget disease is not advised.
Frozen section for melanocytic lesions should be discouraged because the histologic findings may be distorted by freezing artifact. Other important histologic features, including depth of invasion or cytologic atypia, cannot be accurately assessed. Staging and therefore treatment of the patient may be compromised (Smith-Zagone and Schwartz, 2005).
Mesenchymal tumors of the vulva may be specific to the female genital tract or similar to those seen in soft tissues (Nielsen and Young, 2001; McCluggage, 2009; Nucci and Fletcher, 2000). Typically these tumors have been diagnosed previously by biopsy, and the only indication for frozen section is to determine the margin status. One entity that merits comment, given that it usually occurs at this site, is deep (aggressive) angiomyxoma. Management of this tumor depends very much on obtaining a negative margin, and the pathologist may be asked to assess them by frozen section. This can be difficult due to the paucicellular nature of the lesion and to the fact that the myxoid matrix of the neoplasm can be difficult to distinguish from nonspecific edema, particularly in a frozen section. Appreciation of the typical vessels and in some cases an infiltrative growth may be helpful. The distinction from an angiomyofibroblastoma is important and may be aided by the gross characteristics of the neoplasm, including the surgical impression and prior imaging studies (Nielsen et al, 1996; Granter et al, 1997).
Primary tumors of the vagina are extremely rare, with squamous cell carcinoma being the most common. Frozen sections, although infrequent, are typically requested to assess margins or to confirm tumor type. Frozen section evaluation is generally more straightforward in these cases, as compared to those in the vulva, because the complicating factor of adnexal involvement in the vagina by in situ neoplasia is lacking (a rare exception being involvement of adenosis). Also, in our experience, the bulbous expansion of vulvar in situ neoplasia is rarely as striking in the vagina. Secondary tumors of the vagina, either by direct extension or metastasis, may also occur and should always be excluded (Staats et al, 2007). A rare indication for frozen section is the evaluation of a polypoid lesion in children or young adults, in whom embryonal rhabdomyosarcoma (sarcoma botryoides type) is a well-known entity. Distinguishing this sarcoma from the much more common fibroepithelial polyp may be challenging, particularly if only a small biopsy is available. It is important to search carefully for a cambium layer, rhabdomyoblasts, and cross striations, as well as to appreciate the gross characteristics (if known) and to assess the overall cellularity of the lesion (Daya and Scully, 1988; Li et al, 2013; Nucci et al, 2000).
No standard protocols exist for the surgical treatment of cervical cancer because it is largely dependent on the nature and extent of the disease, the desire to preserve fertility, and the patient’s age (Karimi et al, 2010). Tailoring surgery, based on intraoperative findings, improves patient care by enhancing the nature of the operative procedure and potentially preventing subsequent surgery, lessening patient anxiety, and decreasing the cost and risk associated with further surgery (Gu et al, 2004; Neiger et al, 1991). Evaluation of the degree of squamous dysplasia should not be performed intraoperatively because several factors may lead to an inaccurate diagnosis, including sampling issues, poor orientation, and freezing artifact.
In a patient with a prior diagnosis of squamous cell carcinoma, the surgeon may request a frozen section to evaluate depth of invasion. Possible scenarios include a previous biopsy showing equivocal invasion, uncertain depth of invasion, or issues related to fertility. The surgeon must be aware that, while the analysis of a cone biopsy specimen intraoperatively is reasonably accurate in detecting and assessing invasive disease, it is time-consuming (up to 45 minutes) (Giuntoli et al, 2003; Trumbull, 1962), but can be helpful in triaging patients to a simple or a radical hysterectomy (Martinelli et al, 2012). The role of frozen section in cone biopsies in the literature is controversial (Gu et al, 2004; Neiger et al, 1991; Giuntoli et al, 2003; Trumbull, 1962; Fletcher et al, 1985; Greenberg and Kaufman, 1963; Guerriero et al, 1964; Hannigan et al, 1986; Hoffman et al, 1993; Kaufman et al, 1965; Woodford et al, 1986). This approach is, in our opinion, only advised when a previous diagnostic biopsy has been performed (Gu et al, 2004; Woodford et al, 1986), and the findings of the frozen section should be correlated with the previous material; if they are discordant, additional surgical intervention should be delayed until permanent sections can be evaluated. In addition, the quality of the permanent sections may be compromised, and, if the lesion is very small, it may be missed or may disappear in permanent sections (Ren et al, 2012).
Most but not all investigators suggest the accuracy of frozen section diagnosis parallels that of permanent section, including its use in the evaluation of early invasive carcinoma (Gu et al, 2004; Neiger et al, 1991; Giuntoli et al, 2003; Martinelli et al, 2012; Fletcher et al, 1985; Greenberg and Kaufman, 1963). Nonetheless, in our opinion, cervical specimens are best handled by permanent sections in order to ensure optimal microscopic evaluation of the lesion and to avoid loss of diagnostic material. In our institutions, gynecologic surgeons are agreeable to this approach in most instances.
Trachelectomy is emerging as an alternative to radical hysterectomy in patients with early cervical cancer who wish to preserve fertility. The procedure separates the uterine fundus from the lower uterine segment/ endocervix, requiring frozen section examination to determine the distance between the carcinoma and the lower uterine segment/endocervix margin. The goal of the surgeon is to obtain a margin that is 5 mm or greater from the tumor. The pathologist may be asked to evaluate the proximal margin of the specimen and should treat it as a small cone specimen, inking the parametrial soft tissues, as well as the lower uterine segment/endocervix (Ismiil et al, 2009; Park et al, 2008).
Challenges in the interpretation of invasion in a squamous cell carcinoma include:
Sampling if invasive component is minimal (early invasive squamous cell carcinoma)
Involvement of endocervical glands by squamous cell carcinoma in situ
Marked inflammation obscuring the epithelial stromal interface
Cervical stromal decidua
Trophoblastic lesions
Marked artifact
Involvement of endocervical glands by in situ carcinoma can be extensive, and in these cases it is important to pay attention to the contours of the islands because they tend to be smooth and the basal membrane around the nests preserved and easy to identify. Presence of single cells or groups of entrapped endocervical cells may be seen in the center of the nests which also lack the paradoxical keratinization typically seen in early invasive squamous carcinoma. Inflammation is often prominent in carcinoma in situ and may preclude identification of early stromal invasion because the basal membrane is frequently obscured. Freezing artifact may be a major compounding factor in this setting because it adds to the difficulty in the evaluation of the cellular features ( Figure 18-3C, D ). Decidua may closely mimic the morphologic appearance of invasive squamous cell carcinoma, particularly if contiguous to an in situ component in women who are pregnant or taking oral contraceptives. Decidual cells grow in sheets or nodules and have abundant eosinophilic cytoplasm and round nuclei that may display nucleoli (Zaytsev and Taxy, 1987). In contrast to squamous cell carcinoma, the nuclear features are bland with no associated mitotic activity, there is no keratinization, and an associated stromal response is lacking. Trophoblastic lesions, particularly placental site nodule and epithelioid trophoblastic tumor, may potentially be encountered in a frozen section because they are not infrequently located in the cervix (Shih and Kurman, 1998; Shih and Kurman, 2001; Young et al, 1990). Like decidua, they can mimic invasive carcinoma in patients with an in situ squamous cell carcinoma, especially when small nests or single cells with nuclear atypia and containing globular eosinophilic material are present in the stroma. However, in most instances a helpful clue is an extensively hyalinized background.
Evaluation of glandular lesions is a much less common indication for frozen section but is seen with increasing frequency in the current era. Even when evaluating squamous lesions, the glands should be separately assessed because recognition of adenocarcinoma in situ, which is often multifocal, may change surgical management (Martinelli et al, 2012). When the preoperative diagnosis is that of a glandular abnormality, ruling out invasion and, if present, assessing the depth falls in the realm of intraoperative pathologic evaluation. These cases are not always straightforward due to the well-known variability of architecture of even benign endocervical glands, such that when involved by neoplasia, judging invasion is often difficult except in flagrant cases. The finding of striking abnormalities of architecture (cribriform glands and conspicuous papillary formation) or a stromal reaction may be just as helpful in permanent section evaluation.
Mimics of adenocarcinoma in situ parallel those seen in final pathology specimens, namely endometrial epithelium (benign or malignant), tubal and tuboendometrioid metaplasia, superficial endometriosis, Arias-Stella reaction, and microglandular hyperplasia. The latter two are typically encountered in pregnancy or in women taking oral contraceptives, and microglandular hyperplasia may be confused with invasive adenocarcinoma.
Difficulties associated with the distinction between tubal and tuboendometrioid metaplasia, superficial endometriosis, and endocervical adenocarcinoma in situ in the frozen section setting include:
Nuclear pseudostratification
Nuclear elongation and hyperchromasia
Occasional mitoses
Altered stroma
All of these features may be accentuated by freezing artifact.
Although it may be difficult, recognition of cilia or endometrial-type stroma are important clues in making a benign diagnosis (Baker et al, 1999; Oliva et al, 1995). Arias-Stella reaction is typically considered in the differential diagnosis of clear cell carcinoma, and particularly in frozen section the presence of cytologic atypia may cause concern for adenocarcinoma in situ. The variation in nuclear size and quality of the chromatin should aid in making the correct diagnosis (Felix et al, 2010; Nucci and Young, 2004). Microglandular hyperplasia has distinctive histologic features that should allow for the correct diagnosis (Medeiros and Bell, 2010). Benign lower uterine segment may be confused with adenocarcinoma in situ when assessing the lower uterine segment/endocervical margin in a trachelectomy specimen. The presence of cellular stroma and absence of mitoses may help in this distinction (Park et al, 2008). Secondary extension of an endometrial adenocarcinoma may closely mimic an invasive endocervical adenocarcinoma ( Figure 18-4B ), and it may be impossible to distinguish between these two entities on frozen section. However, a sense that the tumor is growing from the outer aspect of the cervix inward, rather than the converse, may be helpful, as well as the finding of squamous metaplasia, which is much more characteristic of endometrial cancer. Awareness of a previous endometrial carcinoma is important when considering a diagnosis of primary cervical adenocarcinoma because in most circumstances the cervical tumor is due to extension from the corpus. The diagnosis of minimal deviation adenocarcinoma is notoriously difficult on biopsy; however, in cone biopsy or hysterectomy, malignant cytologic features and overt invasion are more readily recognized. Accordingly, if the clinical finding of a barrel-shaped cervix is present, or a preoperative biopsy has resulted in an equivocal pathologic interpretation, frozen section may enable a definitive diagnosis, and the appropriate surgical approach may be undertaken (Gilks et al, 1989).
Although lymphoma can occur anywhere in the female genital tract, the cervix is the most common location. It should be suspected in a patient with a monomorphous round blue cell tumor which is often associated with extensive sclerosis. In these cases, if sufficient tumor is available, fresh tissue should be saved for lymphoma protocol. However, even if fresh tissue is not available, a diagnosis of a lymphoproliferative disorder can, in most circumstances, be made on formalin-fixed, paraffin-embedded material utilizing immunohistochemistry and molecular techniques.
Endometrial carcinoma is the most common indication for a frozen section of the uterus. The well-known challenging distinction between complex atypical hyperplasia and low-grade endometrioid carcinoma may be even more difficult at frozen section but nonetheless may be an important distinction. In many cases, a hysterectomy is going to be performed for either because up to 40 % of patients with complex atypical hyperplasia have an associated grade I endometrioid carcinoma (Trimble et al, 2006). If hyperplasia can be confidently diagnosed, only simple hysterectomy will be performed. The goal of the frozen section when cancer has been diagnosed is to identify patients who are at risk for extrauterine spread and require full staging, including pelvic and/or paraaortic lymphadenectomy. The incidence of pelvic lymph node metastases is related to the depth of invasion, tumor type, and grade (Malviya et al, 1989; Mikuta, 1995; Quinlivan et al, 2001; Shim et al, 1992; Zorlu et al, 1993). Pelvic lymph node involvement is predictive of para-aortic lymph node metastases; the incidence of para-aortic lymph node metastases without pelvic lymph node involvement is very low (up to 2 %) (Boronow et al, 1984). Thus a hysterectomy specimen is submitted to confirm tumor type and grade and to assess depth of invasion. A frozen section is not indicated when the prior endometrial biopsy shows a high-grade endometrial carcinoma, including but not limited to serous, clear cell, and high-grade endometrioid.
Algorithms may be used as a guide for surgical management. Some centers include in their frozen section report tumor size (2 cm or less), endometrioid versus nonendometrioid histology, grade if endometrioid type, extent of myometrial invasion, and extension outside the corpus (Kumar et al, 2012). If there is a discrepancy in tumor type and/or grade between the prior biopsy and frozen section findings, the surgeon should proceed based on the overall findings. In a study of biopsy-proven stage I, grade I endometrioid carcinomas, the International Federation of Gynecology and Obstetrics (FIGO) grade was increased in 15.5 % of cases; 2.5 % were changed to serous or clear cell type, and 1 % to carcinosarcoma (Prat et al, 1994). Other researchers have reported similar results (Celik et al, 2010a; Daniel and Peters, 1988; Kumar et al, 2011). It has been shown that gross assessment of depth of invasion becomes less accurate as grade increases (Goff and Rice, 1990). Exceptionally, grade I endometrioid carcinomas may deeply infiltrate the myometrium and frequently are not associated with a gross abnormality (Longacre and Hendrickson, 1999). It should be noted, however, that in some cases, palpation may reveal textural differences which should prompt sampling of the suspicious area in an attempt to disclose tumor not visible to the naked eye. Careful gross examination of lower uterine segment, cervix, uterine serosa, and adnexa should be performed, and any suspicious areas should be evaluated microscopically (Celik et al, 2010b). Frozen section accuracy in assessing depth of myometrial invasion ranges from 70 % to 97 % (Malviya et al, 1989; Celik et al, 2010a; Attard Montalto et al, 2008; Fanning et al, 1990; Kucera et al, 2000; Ozdemir et al, 2009; Turan et al, 2013; Ugaki et al, 2011) compared to approximately 71 % for gross examination alone (Doering et al, 1989) because the latter may fail to reveal any definitive invasion in superficially invasive tumors, although stage is unchanged (Mavromatis et al, 2012; Nevadunsky et al, 2009). It is not crucial to distinguish between adenocarcinoma confined to the endometrium and one with superficial invasion of the myometrium but rather to ensure that those with invasion confined to the inner half are clearly separated from those with deeper invasion.
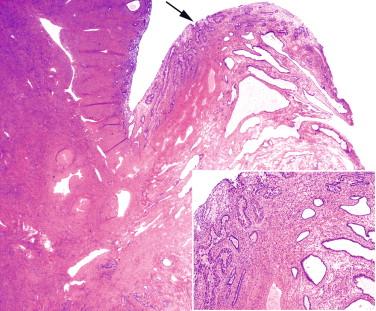
A good approach to examining specimens with endometrial pathology is to bivalve the uterus and to perform serial sections approximately every 5 mm. The number of sections recorded in previous studies has ranged from one to four (Malviya et al, 1989; Shim et al, 1992; Zorlu et al, 1993; Fanning et al, 1990; Noumoff et al, 1991). However, if an invasive tumor is grossly identified, one section usually suffices. If no tumor is visible, random sections should be taken, including full-thickness myometrium, particularly if the wall is thin (Kucera et al, 2000). Pitfalls in assessing depth of invasion include misinterpretation of adenomyotic foci involved by adenocarcinoma as invasive (Kir et al, 2004) or irregular endomyometrial junction involvement as invasive carcinoma. Interpretation may be more difficult than in permanent sections due to limited sampling which may fail to identify areas of adenomyosis not involved by tumor or to identify the outline of the endomyometrial junction ( Figure 18-5 ). As alluded to above, misinterpretation of carcinoma involving adenomyosis as invasion is significant because it can result in the misdiagnosis of deep invasion. Overinterpreting carcinoma as invasive, due to the irregularity of the endomyometrial junction, is not critical because it does not result in a change in stage as compared to permanent sections.
Relying on intraoperative endometrial curettage as a primary diagnostic procedure should be discouraged. The frozen tissue may not be representative, the specimen is often fragmented, and cytologic detail may be obscured by freezing artifact and blood. Additionally, artifactual lymphovascular invasion due to mechanical displacement of tumor into vessels is more common in laparoscopic-assisted hysterectomy specimens (Folkins et al, 2010; Krizova et al, 2011) but not in all studies (Fanfani et al, 2011). In such instances, caution should be exercised, especially if no myometrial invasion is present.
Polyps may harbor subtle carcinomas, and if carcinoma is not identified, the entire polyp should be frozen, especially in patients with a prior diagnosis of serous carcinoma ( Figure 18-6 ) (Prat et al, 1994; Silva and Jenkins, 1990).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here