Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Human papillomavirus (HPV) infection is the cause of virtually all cases of cervical dysplasia/cancer and many cases of vaginal and vulvar dysplasia/cancer.
The majority of HPV infections regress spontaneously, but if the infection persists, dysplasia and cancer may develop.
Smoking increases the likelihood that an HPV infection will persist or progress.
Preventive vaccines are available that prevent HPV infection and the development of dysplasia and cancer.
When Papanicolaou (Pap) testing is used widely, it decreases the incidence of cervical cancer by approximately 50% to 70%.
The Bethesda System terminology is used for the reporting of cervical cytologic specimens.
Colposcopy is used to evaluate women with abnormal Pap tests and/or positive HPV tests.
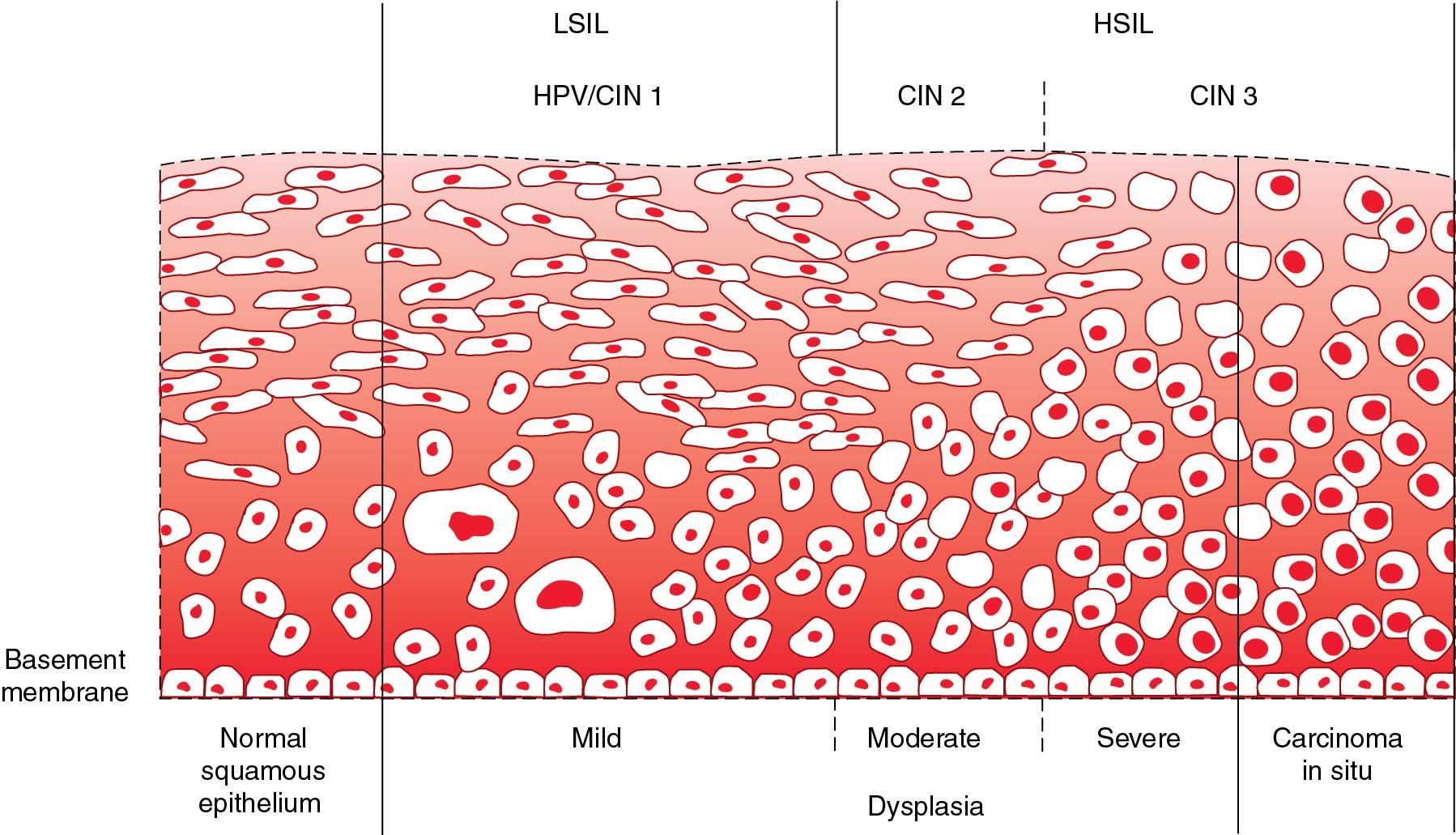
In some cases an HPV infection can lead to a precancerous lesions of the cervix, called cervical intraepithelial neoplasia (CIN) or squamous intraepithelial lesion (SIL). CIN is graded as 1, 2, or 3 depending on the depth of the epithelial thickness involved.
CIN 1 should be observed rather than treated because it usually regresses spontaneously.
Excisional treatment is preferred for histologic HSIL (CIN 2 or CIN 3) in the United States and is recommended for adenocarcinoma in situ (AIS).
Cervical cancer is one of the leading causes of cancer and cancer-related deaths among women worldwide, with an estimated 570,000 new cases and 311,000 deaths annually ( ). In May 2018, the director-general of the World Health Organization (WHO) announced a global call to action toward the elimination of cervical cancer ( ). The focus of this initiative is on low- and middle-income countries (LMICs), where more than 85% of cervical cancer cases and deaths occur primarily because of a lack of organized screening programs ( ). Cervical cancer was previously the leading cause of cancer-related death among women in the United States; however, the incidence and mortality has decreased by approximately 70% over the past 40 years. This decline largely is due to the introduction in 1941 of the Papanicolaou (Pap) test, which led to a systemic effort to detect early cervical cancer and precancerous lesions ( ); however, cervical cancer continues to be the first or second leading cause of cancer and cancer-related death among women in LMICs and many underserved parts of the United States because of the lack of organized screening and early detection programs. Cervical cancer is a preventable disease, with excellent tools for prevention (vaccination) and screening (Pap and human papillomavirus [HPV] testing). Furthermore, there is a treatable preinvasive phase that lasts several years before progressing to invasive cancer.
Virtually all cases of cervical cancer are caused by persistent infection with high-risk types of the HPV ( ). HPV is the most common sexually transmitted infection, and it is estimated that approximately 80% of women will be infected with HPV at some point in their lifetime. The initial infection usually occurs during adolescence or early adulthood, with the majority of women clearing the infection within 18 to 24 months ( ; ; ); however, in 3% to 5% of women the HPV infection persists and they develop significant preinvasive disease, and in less than 1% of all women invasive cancer develops. HPV infection is therefore necessary but not sufficient for cervical cancer development. HPV infection is also the causative agent of other malignancies, including cancer of the oropharynx, anus, penis, vulva, and vagina.
HPV is a double-stranded DNA virus that replicates within epithelial cells ( ; ). To date more than 120 HPV types have been identified, and approximately 40 HPV types are known to infect the genital tracts of men and women. Of these, approximately a dozen are considered high-risk types, with HPV-16 and -18 being responsible for more than 70% of cervical cancers. High-risk HPV causes neoplastic cellular changes when viral DNA becomes integrated into the host cell genome. When this happens, certain repressor areas of the viral genome are lost. Consistently, the loss of these control mechanisms allows for the expression of the viral E6 and E7 genes. The production of oncoproteins results in the inactivation of the p53 and retinoblastoma tumor suppressors ( ). These changes are believed to lead to cell immortalization and rapid cell proliferation; however, in most cases the transformed cells are managed by the individual’s immune system and the infection clears or intraepithelial neoplasia regresses. In some women the transformed cells replicate, and if left untreated, a cancer can develop after a period of several years.
In the United States, cervical cancer is most commonly diagnosed between ages 35 and 44 years ( ). The lifetime risk of developing cervical cancer by age 74 is 0.9% in high-income countries (HICs) compared with 1.6% in LMICs. Similarly, the lifetime risk of death from cervical cancer is 0.3% in HICs compared with 0.9% in LMICs ( ). Despite widespread infection with HPV, most women do not develop cervical cancer ( Fig. 29.1 ). The search for a predictive measure to distinguish between women who are infected and will clear the virus and those in whom the infection will persist and who will develop cancer has been difficult. Although it is clear that women who have a compromised immune system from any cause (e.g., genetic, iatrogenic, infectious) have a greater risk of developing a persistent HPV infection ( ), there is no way to predict which healthy women are unable to clear the virus spontaneously. The risk factors associated with cervical cancer include HPV infection, immunosuppression, smoking, parity, increased number of sexual partners, and oral contraceptive use ( ).

Three preventive vaccines are commercially available. The bivalent vaccine (Cervarix) targets two high-risk HPV types (16 and 18) that account for 70% of the cervical cancer cases worldwide and is no longer available in the United States. The quadrivalent vaccine (Gardasil) targets high-risk HPV types 16 and 18, as well as two low-risk HPV types (6 and 11) that cause genital warts. The nonavalent vaccine (Gadasil-9) targets the same HPV types as the quadrivalent vaccine (6, 11, 16, and 18) and also types 31, 33, 45, 52, and 58 ( ; ; ). In randomized clinical trials all three vaccines have been shown to have 93% to 98% efficacy in the prevention of cervical dysplasia (and presumably cervical cancer) in women not previously infected with HPV-16 and -18. In addition, several studies have shown the vaccines to be safe, with no scientific evidence that HPV vaccination increases the risk of serious adverse events. The vaccines are most effective if given before sexual debut and exposure to HPV ( ; ; ). Only Gardasil-9 is available in the United States.
The Centers for Disease Control and Prevention (CDC) recommends that the HPV vaccine be given to both boys and girls between the ages of 11 and 12 years, but it can be administered as early as 9 years ( ). If given before age 15 years, only two doses are now required (0 and 6 to 12 months). If given at age 15 years or older, or in immunocompromised individual, three doses are required (0, 1 to 2 months, and 6 months). Catch-up vaccination should be offered for females and males aged 13 to 26 years who have not been previously vaccinated ( ). In 2018, the U.S. Food and Drug Administration (FDA) approved the use of Gardasil-9 up to the age of 45 years for both men and women ( ); however, the Advisory Committee on Immunization Practices (ACIP) and the CDC stated that vaccination of men and women between ages 27 and 45 is not recommended for all individuals but should be considered on a case-by-case basis through shared clinical decision making between patient and doctor ( ).
Unfortunately, the uptake of HPV vaccination in the United States has been poor, with only 50% of eligible children receiving all the recommended doses ( ). The uptake in other HICs (Canada, Australia, the United Kingdom) has been much higher, approximately 70%, likely because of government-supported, school-based programs. Several LMICs have instituted HPV vaccination programs because the Global Alliance for Vaccination and Immunization (GAVI) has made the HPV vaccine available to low-income countries for $4 to $5 per dose (compared with approximately $150 per dose in the United States); however, economic, political and logistical barriers in many LMICs have limited universal mass vaccination programs. It is not yet known whether vaccination protection is lifelong or whether a booster dose will be required. Because the vaccines available do not provide protection against all cancer-associated HPV types, and because the duration of immunity is not yet known, routine cervical screening is still recommended in vaccinated women.
Cervical cytologic testing (Pap test) became available in the 1950s after the studies of Dr. Papanicolaou demonstrated that cancer and its precursors could be identified by examining a properly prepared and stained cellular sample scraped from the uterine cervix. The 1941 monograph by Papanicolaou and Traut remains one of the sentinel breakthroughs in the history of preventive medicine. Their work led to the demonstration that local therapy of precancerous lesions can prevent the development of cancer. Despite the fact that it has a low sensitivity, widespread Pap testing has reduced the incidence of cervical cancer by 50% to 70%. In part, the success of this screening technique relies on the fact that it takes many years for invasive cancer to develop after a persistent HPV infection and development of dysplasia and that most women are tested repeatedly ( ). Generally, in the United States, women who develop invasive cervical cancer have never been tested, have not been tested for many years, or had an abnormal Pap test but were unable to return for diagnostic or treatment services.
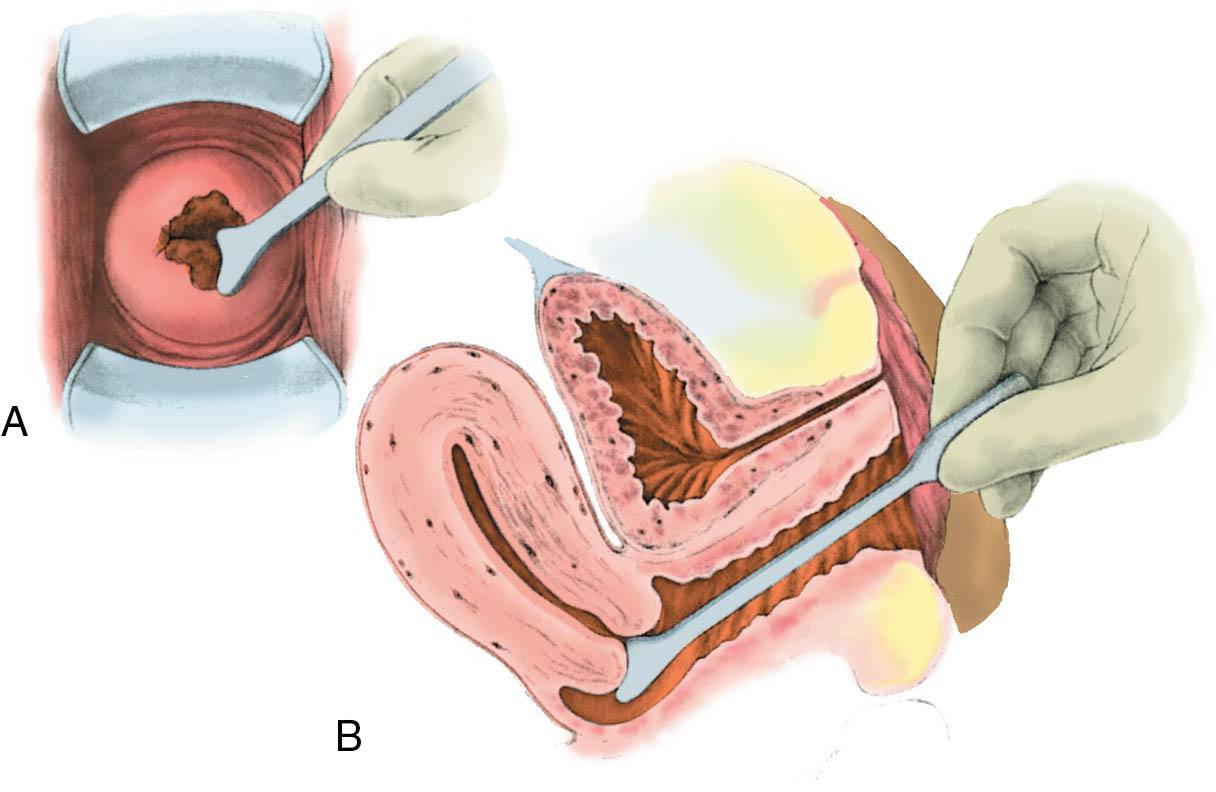
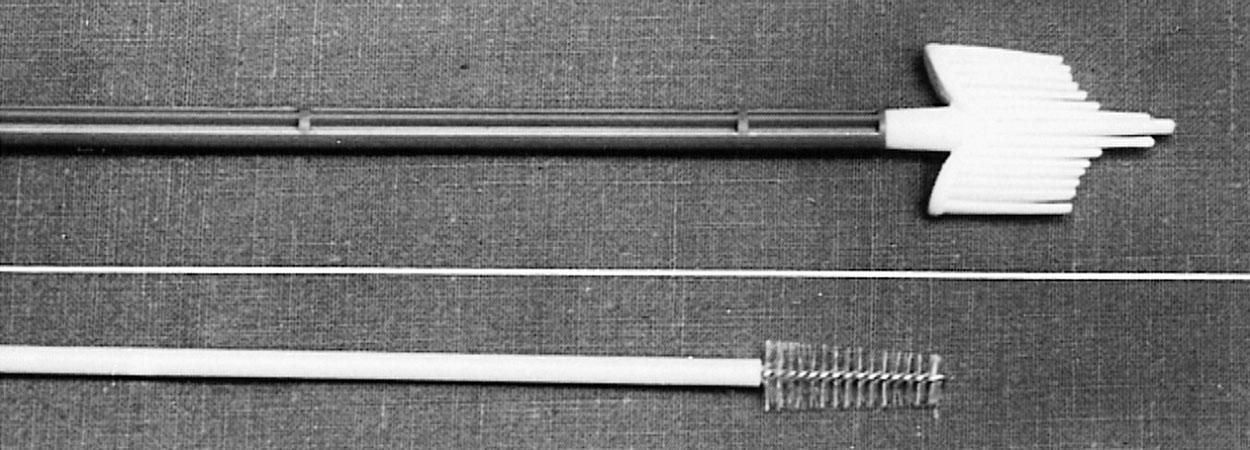
The Pap test (conventional Pap smear) is performed by scraping cervical cells using a spatula and endocervical brush ( Figs. 29.2 and 29.3 ). Cells are sampled from the transformation zone (TZ), which is the area of the cervix where cervical cancer develops. The TZ includes the squamocolumnar junction, which is the area where the squamous epithelium of the ectocervix meets the columnar epithelium of the endocervix, and is dynamic throughout a woman’s lifetime; the squamocolumnar junction migrates from the ectocervix into the endocervical canal as women age and reach menopause. In the past the collected sample was placed on a glass slide and fixed with alcohol. In recent years in the United States and some HICs, this method has been replaced by a liquid-based approach, where the sample is placed in a liquid medium that also can be used for HPV DNA testing.
There is increasing evidence that HPV testing is effective for cervical cancer screening. A number of studies have demonstrated that HPV testing is more sensitive than Pap testing, with only a small loss in positive predictive value ( ; ; ; ). Although the Pap test is still the most widely used screening test in developed countries, cotesting with HPV is now also recommended. The HPV DNA testing has been recommended in countries or regions of the world with any level of available resources ( ; ). Ogilvie and colleagues conducted a large randomized study in Canada that included 19,009 women screened for cervical cancer with HPV testing versus liquid-based cytologic examination. They concluded that HPV primary testing had a significantly lower likelihood of identifying CIN 3+ at 48 months than liquid-based cytologic examination ( ).
The American Society of Colposcopy and Cervical Pathology (ASCCP) guidelines in the United States recommend screening women for cervical cancer between ages 21 and 65 ( ). Cervical cancer screening should not be performed in women younger than 21 years, regardless of age of onset of sexual activity. The screening guidelines are as follows:
21 to 29 years: Pap testing every 3 years; no HPV testing.
30 to 65 years: Cotesting with Pap and HPV every 5 years (preferred) or Pap testing alone every 3 years.
Screening is NOT recommended for women older than 65 years who have had three consecutive negative Pap tests or two consecutive negative HPV tests, provided they have no history of high-grade dysplasia (cervical intraepithelial neoplasia [CIN] 2/3) or cancer (CIN 2+) in the past 20 years; however, women presenting at age 65 years or older who have not had previous screening should undergo Pap and HPV testing.
Screening with a Pap test and/or HPV testing is NOT recommended for women who have had a hysterectomy with removal of the cervix and who do not have a history of CIN 2+.
Of note, these guidelines do not apply to those special populations with additional risk factors and other complicating history.
Primary high-risk HPV screening test has been recommended by the U.S. Preventive Services Task Force (USPSTF) as an alternative screening method in the United States, starting at the age of 30 years. The USPSTF recommends that this group of women could be screened with cervical cytologic testing alone every 3 years, high-risk HPV testing alone every 5 years, or cotesting (cervical cytologic and high-risk HPV testing) every 5 years ( ).
In 1988, the National Cancer Institute convened a conference in Bethesda, Maryland to develop a uniform terminology for the reporting of Pap test results; the result is known as the Bethesda System (TBS) ( ). Almost all laboratories in the United States and those in many countries throughout the world use this terminology. Fig. 29.4 shows how TBS, CIN, and dysplasia categories correspond to tissue changes.
The first part of a TBS report states whether the sample is satisfactory or unsatisfactory. A sample may be unsatisfactory if there is lack of a label, loss of transport medium, scant cellularity, or contamination by foreign material. Few samples are reported as unsatisfactory if a liquid-based technique is used. The report next indicates whether the cellular material is normal. If other than normal, the abnormalities are further divided into squamous and glandular. The cytologist may also comment on whether there is evidence of infection, such as yeast, or changes consistent with a diagnosis of bacterial vaginosis.
In the current guidelines from the American Society of Colposcopy and Cervical Pathology (ASCCP), the recommendations are based on risk of CIN 3+ (CIN 3, adenocarcinoma in situ, or cancer) determined by current tests results combined with patient’s past history. If primary HPV screening is used and the results show positive HPV, it is recommended to perform both a reflex HPV genotyping test, if this is not previously done, and a reflex cytology test. If this is not feasible, referral for colposcopy is acceptable. If positive HPV 16 or 18 and negative cytology (negative for intraepithelial lesion or malignancy, NILM) is documented, a colposcopy is recommended. If minimally abnormal screening results (HPV positive and negative cytology, HPV negative and LSIL with unknown previous screening history) are found, the recommendation is for surveillance with close follow-up at 1 year ( ; ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here