Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intestinal and multivisceral transplantation have evolved significantly over the last three decades. A better understanding of the pathophysiology, improvements in surgical techniques and perioperative management, availability of effective immunosuppression (IS), and above all the experience of the last few decades has resulted in fairly standardized management of these patients. The effect of these improvements is reflected in the overall outcomes of these patients, with many series reporting outcomes similar to or better than parenteral nutrition (PN). Broadly, patients with irreversible gastrointestinal (GI) failure, who can no longer be maintained on PN or have had life threatening complications of PN are candidates for isolated small bowel transplantation (ISBTx) or liver, small bowel, and pancreas transplantation (LSBPTx).
In this chapter we provide a comprehensive overview of ISBTx and LSBPTx, covering topics of indications, patient selection, surgical technique, management of perioperative and postoperative challenges, rejection, long-term complications, and outcomes.
The initial developments in the field of intestinal transplantation were pioneered by Lillehei and Starzl, who attempted small bowel transplantation procedures in the 1950s and 1960s in canine models. Lillehei et al in 1959 reported their initial work on the physiological response of the small bowel to ischemia and in vitro preservation with successful replacement and survival. Starzl et al reported on the technical feasibility of simultaneous homotransplantation of multiple visceral organs, including the liver, spleen, pancreas, omentum, and the entire GI tract. After these early attempts the field of intestinal transplantation was dormant for about 25 years primarily because of a lack of good immunosuppressive agents. With the introduction of calcineurin inhibitors (CNIs), renewed interest developed in the field of intestinal transplantation in the 1980s. Despite improvements in IS, acute rejection (AR) and infectious complications were the two main challenges in the recipients of intestinal allografts and continue to be so even in the current era. In 1989 Starzl et al reported the first two cases of multivisceral transplantation in children with short gut syndrome and liver failure. One of these patients died in the immediate perioperative period. The other patient survived 193 days, eventually dying secondary to complications of posttransplantation lymphoproliferative disorder (PTLD).
The first long-term survivor of a small bowel transplant with enteral autonomy was reported by Grant et al in 1990. During the same time period the introduction of a new immunosuppressive medication, tacrolimus, significantly altered the scenario, allowing for intestinal transplantation to evolve into a more widely performed procedure. Multiple series have since been published from active transplant centers in Pittsburgh and Omaha to help define this new field. The combined liver and small bowel transplantation procedure as originally described by Grant et al was associated with significant surgical complications that added to the overall morbidity of the procedure, at times questioning the utility of the procedure. In the original technique, essentially a pancreaticoduodenectomy was performed on the en bloc composite allograft to remove the pancreatic-duodenal complex. The liver and small bowel were connected to each other by the portal vein with the arterial inflow provided by the celiac axis and the superior mesenteric artery (SMA) on a common aortic patch. In addition, Roux-en-Y hepaticojejunostomy was required to restore biliary-enteric continuity. Not only was the back-table preparation of the allograft technically difficult, especially in pediatric donors, there was a high incidence of torsion of the portal vein and biliary complications. This technique was modified, as reported by Sudan et al, in the “Omaha technique,” in which the pancreas or a rim of pancreatic tissue was left attached to the composite allograft, thereby eliminating the need for dissection and biliary reconstruction. This not only made the back table and the implantation technically easier, but also significantly decreased the morbidity from biliary and pancreatic complications. Another advantage was virtual elimination of portal vein thrombosis secondary to prevention of torsion of the portal vein.
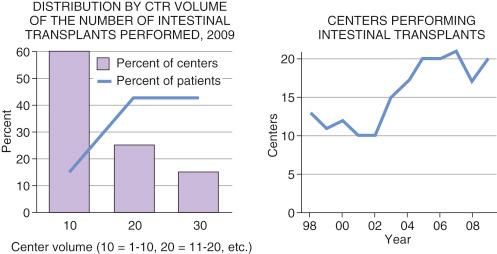
Despite the challenges of surgical technique, perioperative management, rejection, and lymphoproliferative disorders; ISBTx and LSBPTx have shown steady growth in volume as well as centers of expertise over the last couple of decades. Compared to 13 centers in 1998, the number of centers performing intestinal transplants increased to 20 by the end of 2009. Out of these 20, nearly two thirds of the centers performed from 1 to 10 transplants in 2009, and three centers performed from 21 to 30 transplants ( Fig. 66-1 ).
Intestinal failure is a condition, either temporary or permanent, characterized by inability to maintain protein-energy, fluid, electrolyte, or micronutrient balance. Several definitions, both anatomical and functional, have been proposed to describe this entity. Functionally it is characterized by critical reduction in gut mass below the minimum amount necessary for adequate digestion and absorption to satisfy protein-energy nutrition, fluid, electrolyte, and micronutrient requirements.
Anatomically, intestinal failure is defined as reduction in the amount of small intestine, leading to a shortened intestinal remnant that is unable to maintain the protein-energy, fluid, electrolyte, and micronutrient requirements of the body on a conventional diet. Also known as short bowel syndrome (SBS), this condition accounts for nearly three quarters of cases of intestinal failure in adults and roughly half of such cases in children.
The most common causes of intestinal failure in infants are necrotizing enterocolitis, intestinal atresia, gastroschisis, and volvulus ( Table 66-1 ). The common denominator in all these conditions is the reduction in the small bowel length, leading to intestinal failure. Other causes of intestinal failure in this patient population include neuromuscular diseases of the GI tract such as intestinal aganglionosis or congenital disorders affecting the intestinal epithelium. Of note, congenital enteropathies are increasingly being recognized as an important cause of intestinal failure in the pediatric population. These patients present with intractable diarrhea of infancy, which usually begins in the first 2 years of life. The only congenital enteropathies for which intestinal transplantation is indicated are microvillous atrophy and tufting enteropathy. Additional causes of SBS include trauma, malignancies, and postoperative SBS, including inflammatory bowel disease.
| Infants |
| Necrotizing enterocolitis |
| Intestinal atresia |
| Gastroschisis |
| Midgut volvulus |
| Children |
| Cancer |
| Postoperative complication |
| Trauma |
| Motility disorders |
| Adults |
| Iatrogenic complication |
|
|
| Ischemia |
|
|
|
| Infiltration |
|
|
|
|
| Obstruction |
|
|
|
| Functional problems |
|
|
|
Intestinal failure in the adult population is most commonly due to massive resection of healthy bowel or a lesser resection of inherently diseased bowel (see Table 66-1 ). The most common cause of SBS in adults is resection performed for complications of previous abdominal operations. Other causes include mesenteric vascular thrombosis and ischemia, hypercoagulable states, malignancy, irradiation, trauma, and inflammatory bowel disease.
GI motility disorders constitute a wide spectrum of disease conditions that are associated with substantial morbidity. They can be classified as primary, when the disorders are restricted to the gut alone, and secondary, when the GI involvement is secondary to systemic disease. The more severe kinds of motility disorders, like chronic intestinal pseudo-obstruction (CIP) and Hirschsprung’s disease, may have intestinal transplantation as the only option for definitive long-term management.
CIP is a rare syndrome characterized by repetitive episodes of bowel obstruction without any evidence of mechanical obstruction. Many of these patients have associated phenotypic features of mitochondrial myopathies, associated urological abnormalities, and intestinal malrotation. CIP may also arise acutely in adults (Ogilvie’s syndrome) characterized by acute colonic dilation. The chronic type of CIP in adults is mostly secondary to systemic diseases such as scleroderma, systemic sclerosis, or amyloidosis.
Although initially thought to be a disorder exclusively of the distal colon, Hirschsprung’s disease can affect the motor function in other areas of the GI tract, including the small bowel, esophagus, and duodenum. Patients with GI motility disorders are candidates for ISBTx if they are PN dependent, have recurrent episodes of sepsis, or lack central venous access or for LSBPTx if they have developed intestinal failure–associated liver disease (IFALD) (see the next section).
IFALD, also known as parenteral nutrition–associated cholestasis , is defined as a persistent (more than 2 weeks) elevation of liver function test results 1.5 times above the reference range. Nearly 50% of children and 30% of adults have evidence of IFALD after 4 to 12 weeks of PN. Early histological changes are similar to those seen with biliary atresia, neonatal hepatitis, or extrahepatic biliary obstruction and are characterized by bile duct proliferation, periportal inflammation, and fibrosis. With advanced disease, cholestasis is the predominant finding in the pediatric population with rapid progression to end-stage liver disease. On the other hand, the principal change seen in the adults is steatosis with both microvesicular and macrovesicular changes. This can over time progress to steatohepatitis, periportal inflammation, and fibrosis.
IFALD is multifactorial in origin. Specific factors in the PN that have been studied as inciting and/or contributing factors include the phytosterols (present in high concentration in soy-based lipids), which are known to paralyze the bilirubin transport mechanisms across the hepatocyte membrane. Other risk factors associated with IFALD include prematurity, SBS, history of central venous catheter infections, necrotizing enterocolitis, manganese toxicity, and lack of enteral stimulation. The rapidity of its onset and progression in the pediatric population suggests that the immaturity of the liver also play an important role.
Early detection and aggressive multidisciplinary management are essential for the treatment of IFALD. Patient-related interventions include enterobiliary stimulation with feedings, choleretic agents, treatment of bacterial overgrowth, and correction of underlying causes of intestinal stasis. Other interventions include aggressive management of sepsis and improvement in the absorptive function of the GI tract with surgical techniques, including tapering enteroplasties, bowel-lengthening procedures (serial transverse enteroplasty [STEP]), and restoration of GI tract continuity. PN-related modifications include cyclical PN, limiting dextrose in PN to less than 75% of the nonprotein calories, minimizing manganese and aluminum toxicity, restricting the amount of lipids to less than 3.5 g/day in children and less than 1 g/kg/day in adults. Administration of pure omega-3 fish oil–based emulsions instead of soy-based lipids has been shown to improve cholestasis, especially in pediatric population. Although no current data are available to suggest a difference in outcomes, omega-3 fatty acid–based lipid emulsions may provide an additional asset in the management or prevention of IFALD.
Patients with end-stage liver disease secondary to IFALD need further evaluation for either isolated liver transplantation or LSBPTx depending on their age, length of remnant bowel, underlying disease process, potential for enteral autonomy, and associated comorbidities. Patients less than 2 years of age who have developed liver failure as a consequence of PN and have achieved intestinal autonomy are potential candidates for liver transplantation alone.
From a practical standpoint, the inability to maintain ideal body weight without PN or failure to wean off PN are indicative of irreversible intestinal failure. The mortality rate of patients requiring PN for intestinal failure has been estimated to be between 20% and 25% depending on the underlying cause. In addition, infants have the highest risk for IFALD, which is responsible for nearly half the mortality in this subgroup of patients.
All patients with a diagnosis of intestinal failure should have an early referral to a comprehensive intestinal rehabilitation center for evaluation of intestinal failure and to assess candidacy for transplantation. It has been shown that the wait-list mortality for intestinal transplantation is higher than that for other solid organ transplants, and patients who are transplanted while waiting at home have an approximately 15% higher survival rate than those who are transplanted while waiting in the hospital. Criteria for referral of patients with intestinal failure who are potential candidates for intestinal transplantation are listed in Table 66-2 . These are more inclusive and less restrictive than the listing criteria for intestinal transplantation ( Table 66-3 ), the rationale being that timely evaluation and listing are critical to improved survival. Many of the patients who are referred for evaluation can be managed by modifications of their medical management and surgeries like STEP, intestinal tapering, and takedown of fistulas to achieve enteral autonomy.
| Children with massive intestinal resection |
| Adults with small bowel length of 100 cm without the ileocecal valve |
| Children with severely diseased bowel and unacceptable morbidity |
| Microvillus inclusion disease or intestinal epithelial dysplasia |
| Two or more episodes of fungemia or life-threatening sepsis |
| Persistent hyperbilirubinemia (>6 mg/dL) |
| Thrombosis of two of the four upper body central veins |
| Continuing prognostic or diagnostic uncertainty |
| Request of the patient or family |
|
|
|
|
Broadly speaking, intestinal transplantation is indicated for patients with irreversible intestinal failure who no longer can be maintained on PN, have developed IFALD, have a complex abdominal visceral pathologic condition that cannot be effectively treated by other means, or have had life-threatening complications from PN. It has been argued, based on published literature from Pittsburgh, that because intestinal transplantation may achieve survival rates similar to or better than those of PN, intestinal transplantation should be offered to all patients who are PN dependent.
Contraindications to ISBTx and LSBPTx are essentially similar to those for other solid organ transplants. Patients with profound neurological disabilities, life-threatening or noncorrectable systemic illnesses, severe congenital or acquired immunodeficiencies, nonresectable malignancies, and multisystem autoimmune disorders are not candidates for transplantation. In addition, insufficient patent vasculature to guarantee easy central venous access for up to 6 months post transplantation is also a contraindication for intestinal transplantation.
Pretransplant evaluation is a multidisciplinary process wherein the primary objective is to assess the suitability of the candidate for the major surgical endeavor and also plan ahead for anticipated postoperative issues and long-term care. Broadly speaking, this evaluation process aims to address five issues. These include comprehensive evaluation of the patient’s clinical status before transplantation, exclusion of patients in whom transplantation can be avoided or is contraindicated, stabilization and improvement of the patient’s nutritional and clinical status, and ensuring that the patient and the family understand what to expect in the postoperative course and in the long term and how to best handle the issues, if and when they arise.
The initial evaluation of potential candidates for ISBTx or LSBPTx includes a complete and thorough understanding of the past medical and surgical history, comprehensive assessment of the patient’s nutritional status, including assessment of anthropometric and nutritional indices, and a complete physical examination. Baseline hematological, biochemical, and serological test results (cytomegalovirus; Epstein-Barr virus [EBV]; hepatitis A, B, and C; herpes simplex virus; human immunodeficiency virus; varicella zoster virus; measles; rubella; toxoplasmosis) are obtained to establish the initial reference point. It is important to note here that as and when abnormalities are detected during the evaluation process, attempts are made to correct these deficiencies promptly to prepare the patient for transplantation. Additional evaluation, including upper GI endoscopy and liver biopsy, may be necessary to evaluate the degree of liver dysfunction because this can alter the planned transplantation operation by estimating the necessity for a liver transplant.
The functional and anatomical assessment of the GI tract comprises radiological, endoscopic, and histological assessment. The simplest and one of the most informative studies in the initial evaluation is the barium or meglumine diatrizoate (Gastrografin) study of the entire GI tract. Additional radiological investigations include ultrasound and computed tomography (CT) scan of the abdomen in select patients and motility studies in patients with a history of pseudo-obstruction to assess the severity and extent of their disease. Patients with a history of vascular events such as mesenteric vascular thrombosis warrant a thorough workup to rule out an underlying hypercoagulable disorder. Doppler studies of the deep venous system are done to rule out deep venous thrombosis and ascertain the availability of central venous access. Occasionally, conventional venogram is required to roadmap the central venous system, especially in patients with history of multiple deep vein thromboses.
Additional tests are done to assess the suitability of the patient for major surgery. Depending on the age and the presence of comorbidities, these patients undergo chest x-ray, pulmonary function tests, electrocardiography, echocardiography, dobutamine stress echocardiography, mammography, colonoscopy, and psychological assessment. Estimation of glomerular filtration rate is done to establish the baseline renal reserve and rule out the need for preemptive kidney transplantation in patients with chronic renal insufficiency. Last but not least, the nurse coordinators, the social worker, and the financial counselor play a vital role in this entire evaluation process. They are the initial point of contact for the patients for all issues and play an important role in providing emotional support, coordinating care, and ironing out the financial issues that the patient or the family may have to deal with in the future.
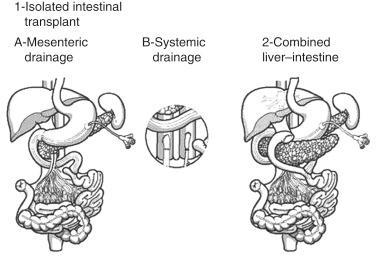
Patients with intestinal failure who are candidates for transplantation are a highly diverse group and need individualized assessment as to what type of allograft would be best for them. This is primarily dictated by the anatomical as well as functional status of their solid and hollow viscera. The options for these patients are ISBTx, liver transplant alone (LTA), or LSBPTx with or without foregut sparing ( Fig. 66-2 ).
ISBTx is indicated in patients on PN who have minimal associated liver failure or the liver failure is at a stage where it is potentially reversible. At times it may be difficult to make an accurate assessment of the degree of liver injury and can be challenging. Generally this decision is guided by the presence of portal hypertension or the presence of bridging fibrosis on liver biopsy. One should remember that the findings of portal hypertension may be subtle in patients with SBS secondary to reduced or absent mesenteric flow. The degree of mesenteric and splenic vein thrombosis also plays a crucial role in deciding on the type of allograft. For example, a patient with extensive thrombosis of the splenoportal axis would be suited for an LSBPTx, whereas a patient with isolated splenic vein thrombosis can be managed with ISBTx and splenectomy.
In some patients with intestinal failure, severe IFALD develops despite an adequate intestinal remnant with the potential for enteral autonomy except for the presence of liver failure. Not only does the associated liver failure hinder the process of intestinal adaptation, it contributes to failure to thrive by secondarily impairing nutrient and electrolyte absorption. LTA may optimize the conditions for enteral autonomy in these patients by removing the inhibitory influences of ascites, intestinal edema, gastrointestinal bleeding, and luminal deficiency of bile salts. LTA in these patients should not be performed as a bridge to ISBTx; instead it should be limited to carefully selected patients with the potential of future enteral autonomy but for the presence of IFALD. Overall, predictors of enteral autonomy after LTA for IFALD include maximum enteric caloric tolerance of more than 50% of requirements, at least 25 cm of normal-appearing small bowel from the ligament of Treitz, and age less than 2 years.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here