Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter is focused on injuries of extracranial, cranial, intracranial, spinal cord, and peripheral nervous system structures. In particular, the emphasis is on those disorders that appear to be related primarily to mechanical trauma. Adverse mechanical events occur principally during labor and delivery. Unfortunately, such events often lead to criticism of obstetrical management. Such criticism generally is unwarranted, because the mechanical factors are most often beyond the control of the obstetrician. Indeed, in many well-documented instances, apparent “traumatic” lesions are related to unknown antepartum events or to developmental or acquired lesions evolving in utero. Nevertheless, perinatal mechanical traumatic events do occur, result in well-defined clinical syndromes and require recognition and appropriate management. The chapter is organized into extracranial, cranial, intracranial, spinal cord, and peripheral nervous system lesions.
A brief caveat concerning terminology is important to note in the introduction to this chapter. The terms “perinatal trauma” and “birth injury” have been given definitions so broad as to be confusing and nearly meaningless. Indeed, a commonly used definition of birth injury is considered to be any condition that affects the fetus adversely during labor or delivery. In this discussion, however, “perinatal trauma” refers to those adverse effects on the fetus during labor or delivery and in the neonatal period that, as noted earlier, appear to be caused primarily by mechanical factors. Thus specifically excluded are the disturbances of labor and delivery that lead principally to hypoxic-ischemic brain injury (see Chapter 21, Chapter 22, Chapter 23, Chapter 24, Chapter 25 ). (Nevertheless, potential overlap between mechanical trauma and the occurrence of hypoxic-ischemic cerebral injury is important to recognize because perinatal mechanical insults may also result in hypoxic-ischemic cerebral injury, perhaps secondary to disturbances of placental or cerebral blood flow. However, the precise mechanistic relationships remain largely unknown.)
The incidence of traumatic brain injury is difficult to establish conclusively. Nevertheless, it is clear that there have been drastic reductions in the occurrence of traumatic injuries to central and peripheral nervous structures, primarily because of improved obstetrical management. Specific examples are apparent in the subsequent discussions, but recurring themes are the rational use of cesarean section and improved techniques of manual and instrumental vaginal deliveries.
The major varieties of perinatal trauma are outlined in Table 40.1 . These include extracranial hemorrhage, skull fracture, intracranial hemorrhage, cerebellar contusion, spinal cord injury, and several types of injury to the peripheral nervous system; for example, nerve roots and cranial or peripheral nerves. The injuries to extracranial, cranial, and central nervous system structures are discussed first.
| Extracranial Hemorrhage | Cerebellar Contusion |
|---|---|
|
Spinal Cord Injury |
| Peripheral Nervous System Injury | |
|
|
| Skull Fracture | |
|
|
| Intracranial Hemorrhage | |
|
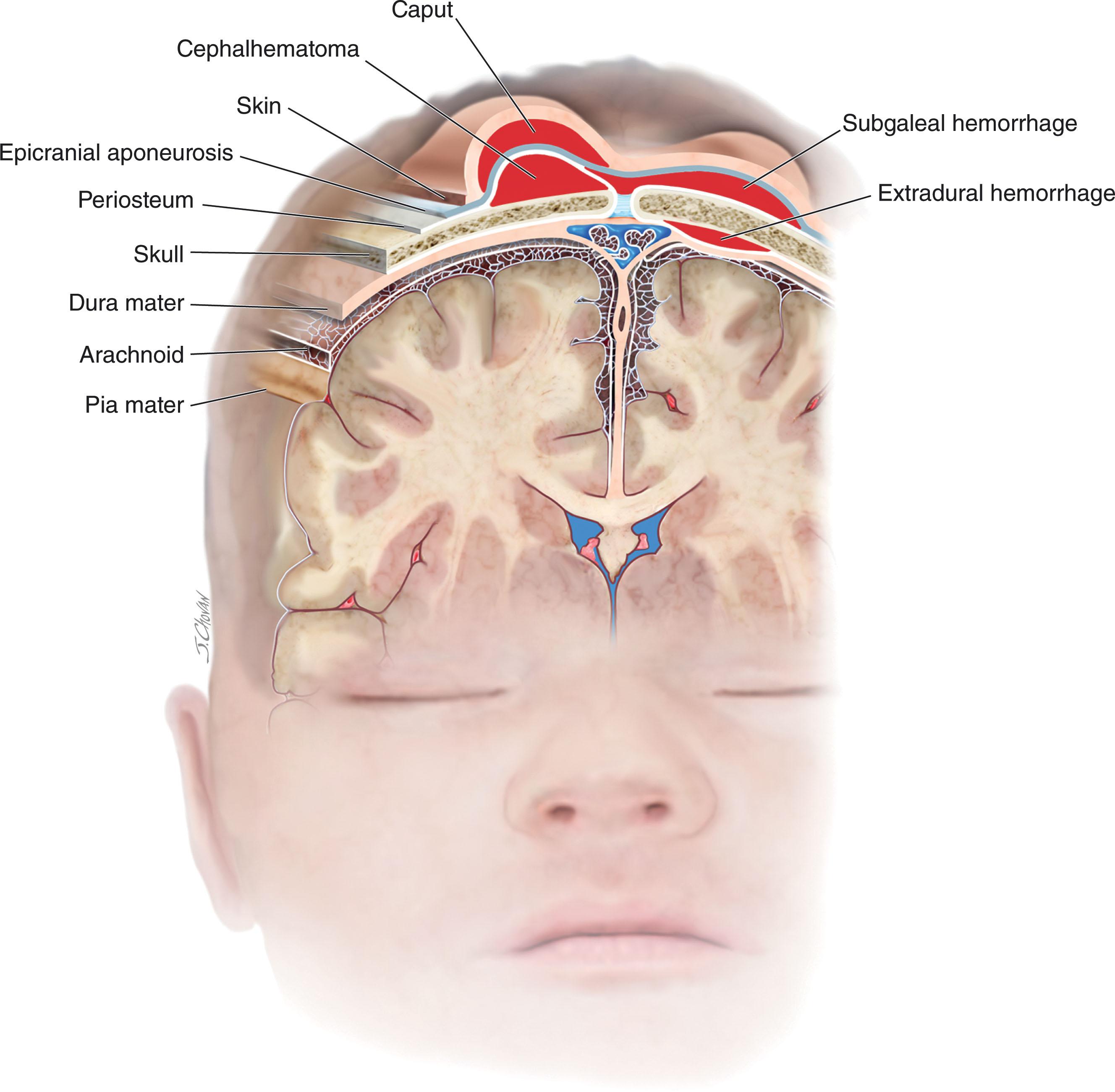
The three major varieties of extracranial hemorrhage are caput succedaneum, subgaleal hemorrhage, and cephalhematoma. These lesions occur in different tissue planes between the skin and the cranial bone ( Fig. 40.1 and Table 40.2 ).
| LESION | FEATURES OF EXTERNAL SWELLING | INCREASES AFTER BIRTH | CROSSES SUTURE LINES | MARKED ACUTE BLOOD LOSS |
|---|---|---|---|---|
| Caput succedaneum | Soft, pitting | No | Yes | No |
| Subgaleal hematoma | Firm, fluctuant | Yes | Yes | Yes |
| Cephalhematoma | Firm, tense | Yes | No | No |
This term refers to the hemorrhagic edema that is observed very commonly after vaginal delivery. Compression on the presenting part, exerted by the uterus or cervix, is the most common pathogenesis. Caput and related scalp injuries have been reported in 10% to 20% of deliveries by vacuum extraction. The usual site of caput formation is the vertex, and marked molding of the head is a common accompaniment. The edema is soft, superficial, and pitting in nature and crosses sites of suture lines (see Table 40.2 ). The lesion steadily resolves over the first days of life, and no intervention is necessary.
Subgaleal hemorrhage refers to hemorrhage beneath the aponeurosis covering the scalp and connecting the frontal and occipital components of the occipito-frontalis muscle (see Fig. 40.1 ). (Understandably, this lesion also is termed “subaponeurotic” hemorrhage.) Blood may spread beneath the entire scalp and even dissect into the subcutaneous tissue of the neck.
Pathogenesis of subgaleal hematoma is related to a combination of external compressive and dragging forces, occasionally aided by a coagulation disturbance (e.g., vitamin K deficiency or hypoxic-ischemic encephalopathy). A strong association with delivery by vacuum extraction is suggested by available data. In one series, approximately 90% of the lesions were associated with vacuum extraction. In a prospective series of 71 infants with subgaleal hemorrhage and delivery by vacuum extraction, a strong relationship was observed with maternal nulliparity and placement of the vacuum cup over the sagittal suture or <3 cm from the anterior fontanel. The latter two factors would cause the vacuum extractor to exert traction forces with slanting or shearing effects on the scalp, considered to be central to the rupture of the emissary veins in the subgaleal space.
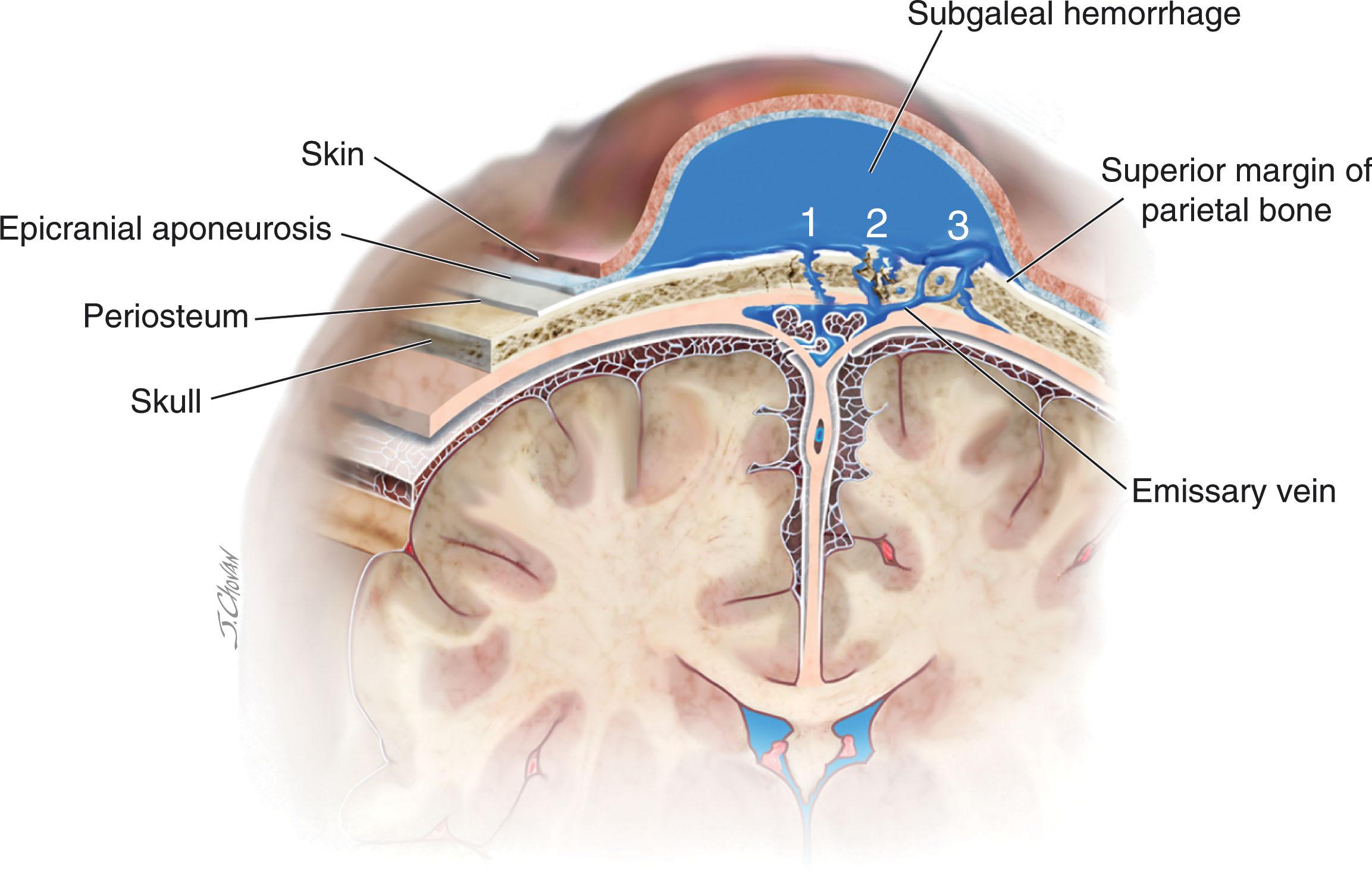
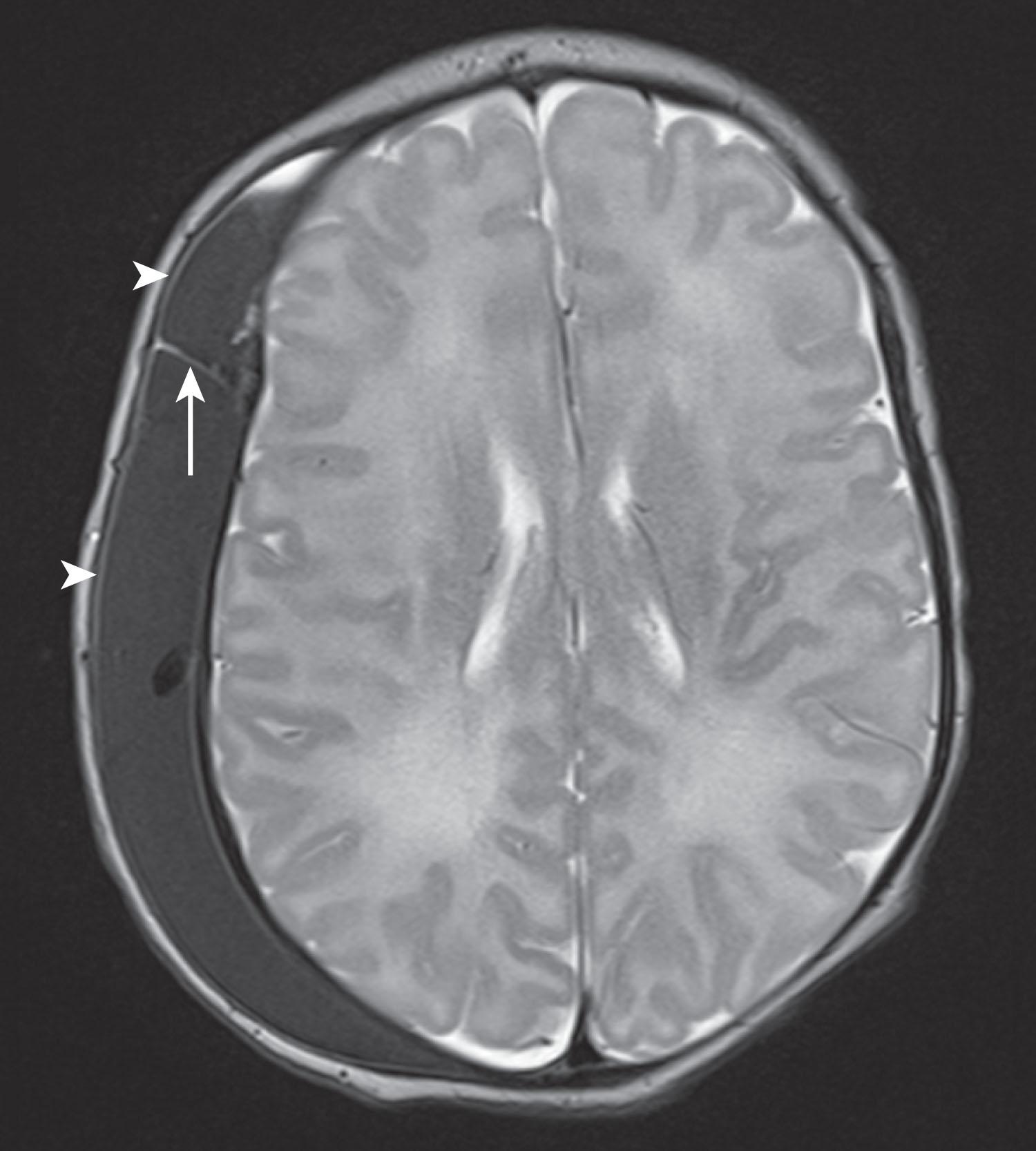
The clinical features of those infants with subgaleal hemorrhage associated with vacuum extraction began at 1 hour of age and had an appreciable incidence of hypovolemic shock (10%), requirement for volume expansion or inotropic support (35%), need for transfusion for anemia (35%), secondary coagulopathy (50%), and hyperbilirubinemia (35%). An association with hypoxic-ischemic encephalopathy, although relatively uncommon (23% of subgaleal hemorrhage in one series of 56 cases ), is notable, because such infants have a higher risk of complications associated with blood loss and an unfavorable outcome. In a unique study of 27 affected infants by computed tomography (CT) scan, 14 infants demonstrated various angulation abnormalities of the parietal bones; such abnormalities suggest that the lesion can result from bleeding caused by one or more of three mechanisms (linear skull fracture, suture diastasis, fragmentation of the superior margin of the parietal bone) illustrated in Fig. 40.2 . This lesion is much less common than caput succedaneum, although precise incidence of the former is unknown. In a recent study of infants ≥35 weeks gestation, the incidence of subgaleal hemorrhage was approximately 1 per 1000 (56 cases among 54,048 live births). In contrast to uncomplicated caput, subgaleal hematoma presents as a firm, fluctuant mass; increases in size after birth; and may be present in the subcutaneous tissue of the posterior neck (see Table 40.2 ). Diagnosis of a subgaleal collection can be confirmed by cranial ultrasonography by demonstrating fluid crossing suture lines in the subgaleal space. Though neuroimaging is not generally indicated, one recent study demonstrated that a majority of subgaleal collections had either no or minimal blood products on magnetic resonance imaging (MRI).
Management consists of close surveillance for signs of blood loss, coagulopathy, and the development of hyperbilirubinemia. Urgent blood transfusion may be necessary. Notably, however, these complications are rare in the absence of accompanying encephalopathy (see earlier). After the acute phase, the lesion resolves over 2 to 3 weeks.
Cephalhematoma refers to a circumscribed region of hemorrhage overlying the skull and confined by cranial sutures (see Fig. 40.1 ).
Cephalhematoma occurs in approximately 1% to 2% of live births. The lesion is nearly twice as common in males as in females and is more frequent in children of primiparous than multiparous mothers. The use of forceps or vacuum extraction in delivery sharply increases incidence. In one large earlier series the incidence of cephalhematoma after the use of outlet forceps was 4.3%, after low forceps, 7.4%, and after midforceps, 9.5%. More recent data indicate that these incidences have declined considerably. Vacuum extraction increases the likelihood of cephalhematoma over threefold relative to the incidence with forceps deliveries. In one careful series of term infants, cephalhematoma occurred in approximately 10% of vacuum-assisted deliveries. Among premature infants the incidence was 20%.
The hemorrhage is subperiosteal in cephalhematoma, as opposed to the edema and blood in caput succedaneum and subgaleal hemorrhage, which are located over the periosteum in either the subcutaneous or subaponeurotic spaces (see Fig. 40.1 ). The subperiosteal locus explains the confinement of the hematoma by cranial sutures (see Table 40.2 ). By far the most common locus of cephalhematoma is over the parietal bone and unilateral. The rare occipital cephalhematoma, midline in location because of confinement by the lambdoid sutures, may mimic occipital encephalocele. (Cranial ultrasound scan is a convenient means to make this distinction.) An underlying linear skull fracture is detected in 10% to 30% of cases of cephalhematoma. The presence of a skull fracture increases the possibility of accompanying intracranial hemorrhage. In one series 9 of 10 infants with cephalhematoma associated with skull fracture also had intracranial hemorrhage, including subdural and epidural hemorrhage.
Cephalhematoma is caused by mechanical forces; that is, is clearly a traumatic lesion in nearly all cases. The most reasonable formulation for pathogenesis implicates generally unavoidable obstetrical factors, relating to the size of skull and birth canal and to the use of forceps or vacuum, causing tight apposition of subcutaneous structures to the periosteum but separation of periosteum from bone by external dragging forces.
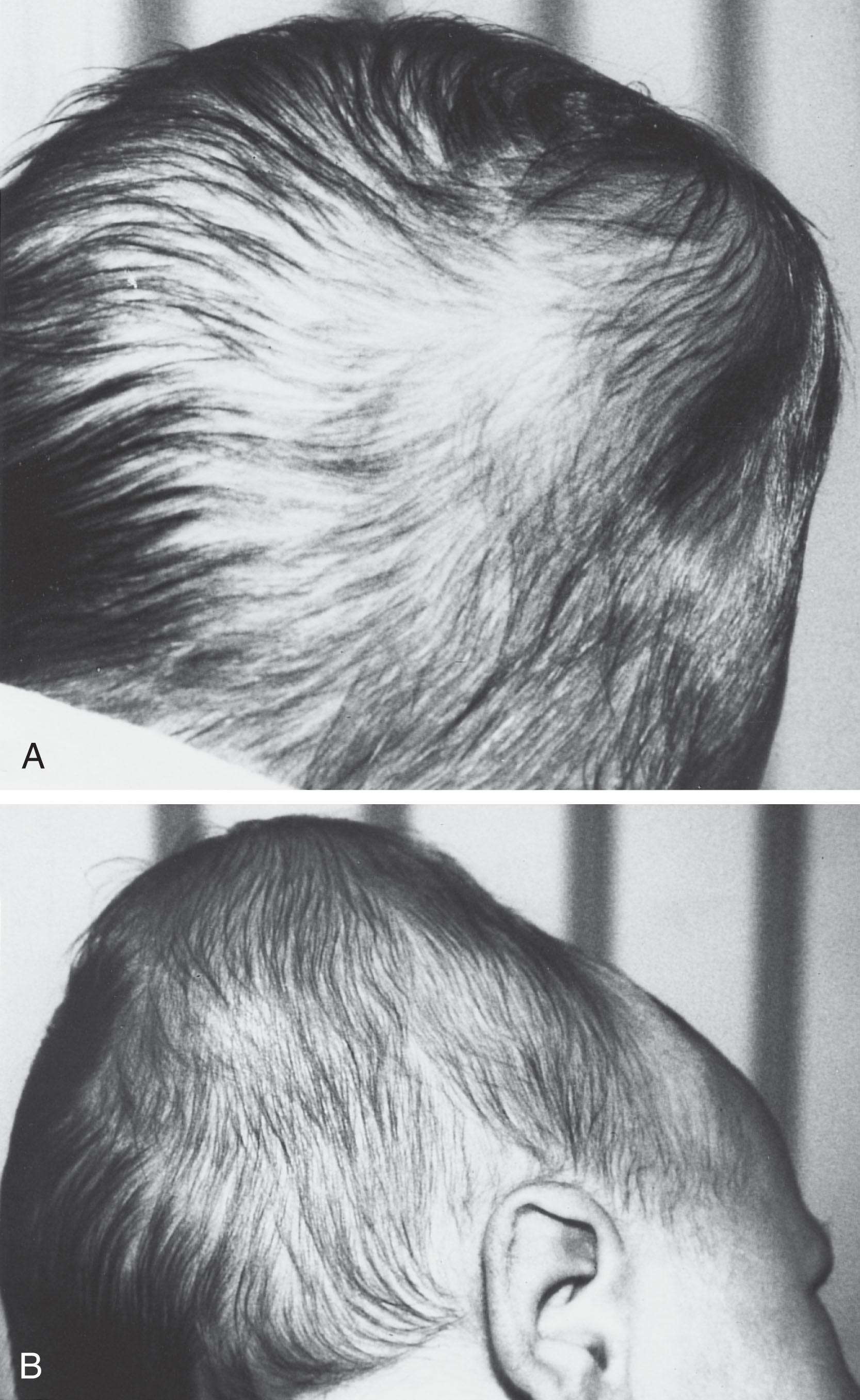
The lesion usually increases in size after birth and presents as a firm, tense mass that does not transilluminate (see Table 40.2 and Fig. 40.3 ). The elevated periosteum palpable at the margin of the hematoma causes the palpating finger to appreciate a ridge at the margin of the lesion and a recessed center. This finding is mistaken readily for a depressed skull fracture. Rarely, contiguous cephalhematomas will appear to cross suture lines and thus will be mistaken for subgaleal hematoma ( Fig. 40.4 ). Cephalhematoma is rarely of clinical significance from the neurological standpoint unless a complicating intracranial lesion is present. As noted earlier, linear skull fracture is an occasional accompaniment of cephalhematoma, and in this setting there is a clear association of linear skull fracture and intracranial hemorrhage. I have seen one infant with an infected cephalhematoma and meningitis. Rare additional complications are hyperbilirubinemia, late-onset anemia, and osteomyelitis.
Essentially all cephalhematomas resolve in a few weeks to months. The few that calcify and result initially in hard skull protuberances usually gradually disappear over many months of skull growth and remodeling. Rarely, a cephalhematoma may ossify and result in a persistent disfiguring protuberance; such lesions require surgical repair.
No specific neonatal therapy is indicated. The degree of acute blood loss rarely requires urgent intervention. Evacuation of the lesion is contraindicated. Treatment of the unusual neonatal complications, especially large intracranial hemorrhage, may be necessary.
Three principal bony lesions of the newborn are categorized appropriately under the designation skull fracture. These lesions are linear and depressed skull fractures and occipital osteodiastasis (see Table 40.1 ). In fact, only with linear skull fracture is there loss of bony continuity and, therefore, true fracture.
Linear skull fracture refers to a nondepressed fracture and is most commonly parietal in location ( Fig. 40.5 ).
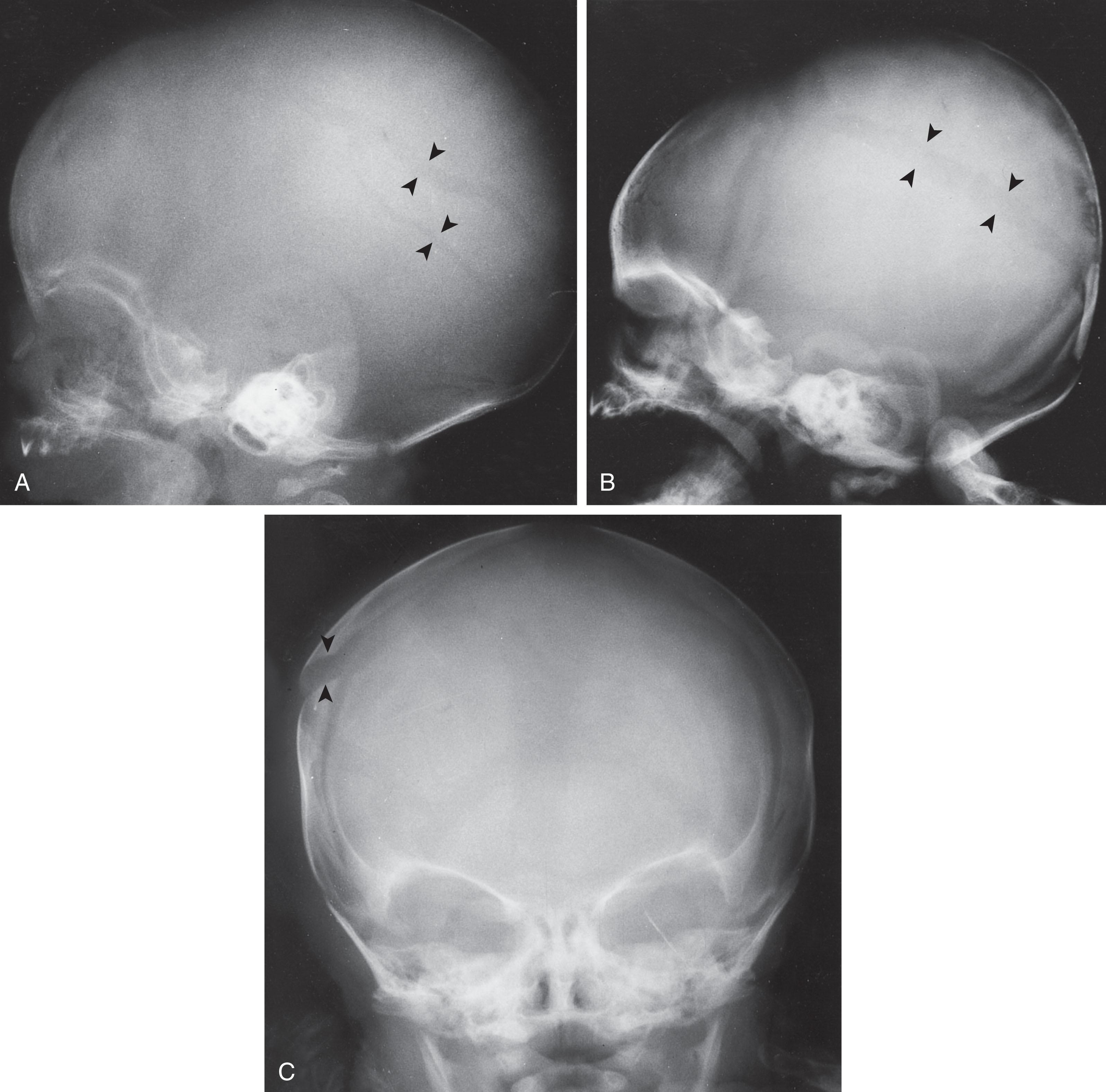
Linear skull fractures are relatively common in newborns; however, the incidence is difficult to determine precisely because identification of the lesion depends particularly on the frequency of radiographic studies and the diligence of examination. In one older series (1975) the incidence was 10%, but more recent data indicate an incidence less than 3%. The incidence after vacuum-assisted delivery is approximately 5%.
Linear skull fracture may be associated with extracranial (e.g., cephalhematoma) and intracranial (e.g., epidural and subdural hemorrhage) complications. It should be emphasized, however, that the more serious, intracranial complications are uncommon concomitants of linear skull fracture in the newborn. Also rarely, the fracture is associated with a tear of the dura and subsequent development of a leptomeningeal cyst. Leptomeningeal cyst also may occur after an unusual type of linear fracture; that is, coronal suture diastasis, particularly secondary to vacuum extraction.
Linear skull fracture is principally a traumatic lesion. Direct compressive effects are probably most important in genesis of the fracture. An increasingly recognized pathogenetic factor is accidental fall; in a recent series, skull fracture in 7 of 13 infants resulted from accidental neonatal falls.
No clinical feature is associated with the fracture per se. The important clinical point is that the fracture should alert the physician to the possibility, however remote, of a more serious intracranial traumatic lesion, such as epidural or subdural hemorrhage. Low-dose CT scan can provide a rapid early assessment but is not recommended unless it is the only available imaging modality. Although ultrasound is a good alternative in older infants, its role in newborns has not been fully studied. The development of a leptomeningeal cyst over the weeks or months subsequent to fracture can be suspected at the bedside by the finding of increased transillumination of the affected region and defined in more detail by MRI scan.
No therapy is indicated. Follow-up skull radiographs at several months of age are useful to document that healing has occurred and that a widened defect indicative of an enlarging leptomeningeal cyst has not developed.
Depressed skull fracture in the newborn usually refers to the “ping-pong” lesion associated with inward buckling of the unusually resilient neonatal bone, usually without loss of bony continuity ( Fig. 40.6 ).
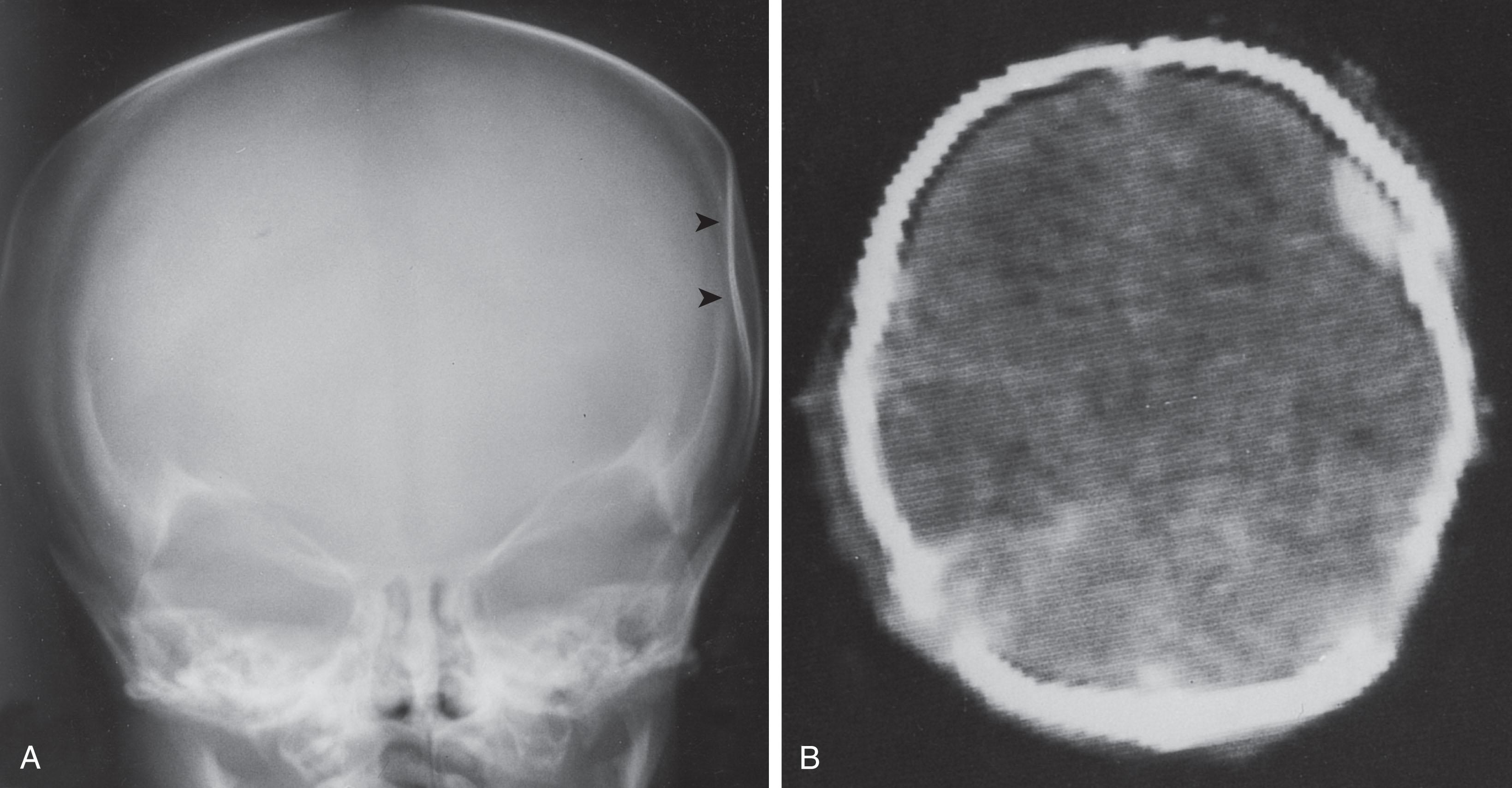
In one large series of 270 infants “injured at birth,” 32 exhibited depressed skull fracture. The use of forceps was common; thus in 28 of these 32, forceps were known to have been used. In a more recent series 50 of 68 cases of depressed skull fracture occurred after instrument-related delivery.
The most common site of depressed fracture is the parietal bone. Although in the vast majority of cases there is no visible fracture, occasionally bone fragments may be seen. Rarely, epidural or subdural hemorrhage or cerebral contusion is associated.
Depressed fracture is almost certainly a result of localized compression of skull. The compressing force is generated by either forceps or pressure against maternal pelvic structures during labor. Prolonged second stage of labor followed by forceps delivery was the most common sequence in one large series. Rarely, depressed skull fracture may occur in utero.
The obvious and palpable bony defect calls immediate attention to the lesion ( Fig. 40.7 ). Neurological accompaniments are unusual and relate to associated intracranial traumatic complications. Neurological complications are rare in spontaneous depressed skull fracture but are relatively common in those related to forceps deliveries. Indeed, in the latter group, epidural or subdural hemorrhage complicates 30% of cases and subsequent neurological sequelae occur in 4%.
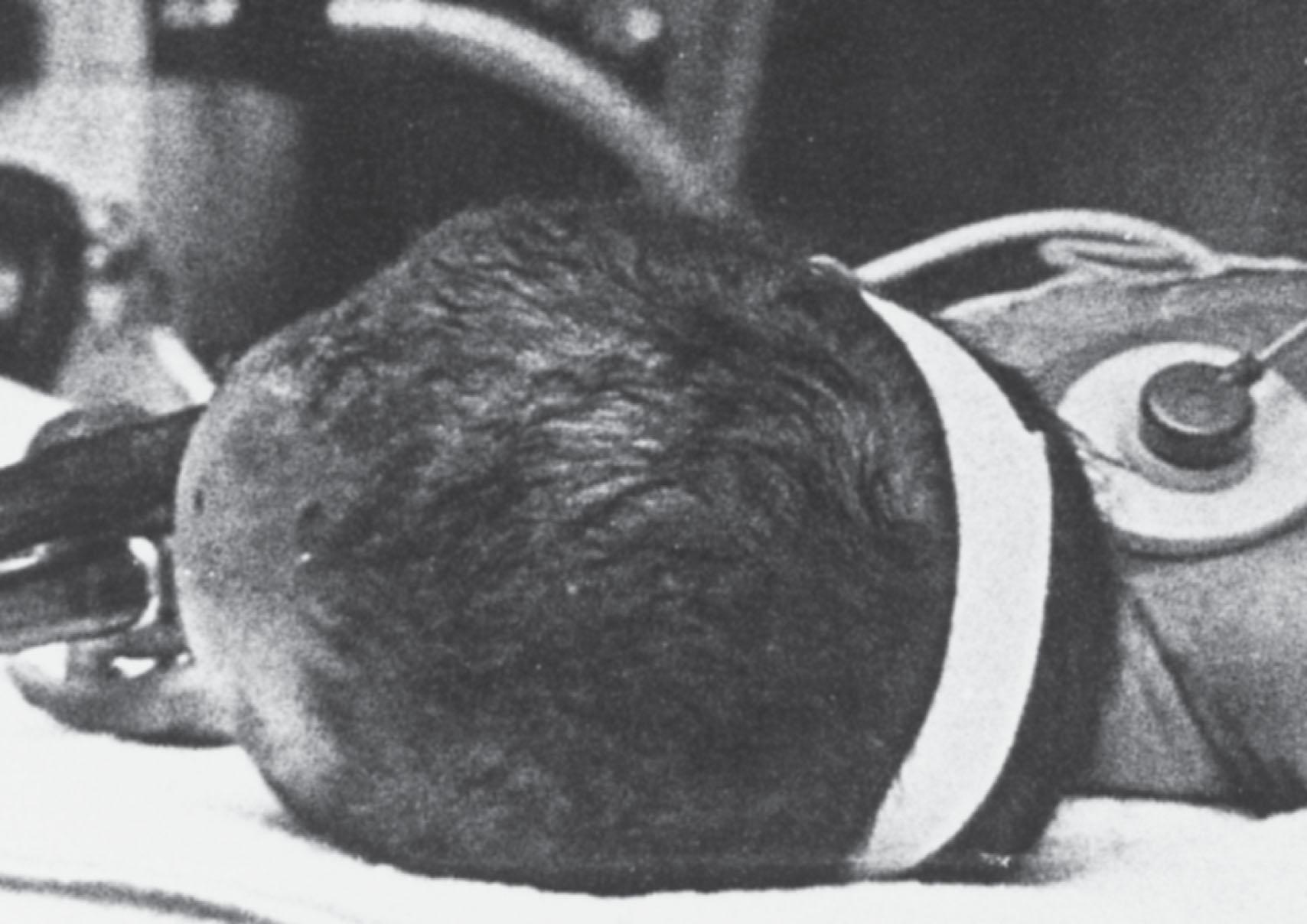
Traditionally, depressed fractures were considered an indication for neurosurgical elevation. This view was challenged later by the observation in several cases of spontaneous elevation of the deformity. Indeed, the natural history of neonatal depressed skull fracture is unclear and the incidence of spontaneous elevation unknown. This fact and the reports of elevation by digital pressure and use of breast pump or obstetrical vacuum extractor suggest that neurosurgical intervention may be indicated less commonly than is currently used. The combination of a transparent breast pump shield attached to a vacuum extractor appears to be particularly useful ( Fig. 40.8 ). Nevertheless 85% of 68 cases in one series were said to “require neurosurgery.”
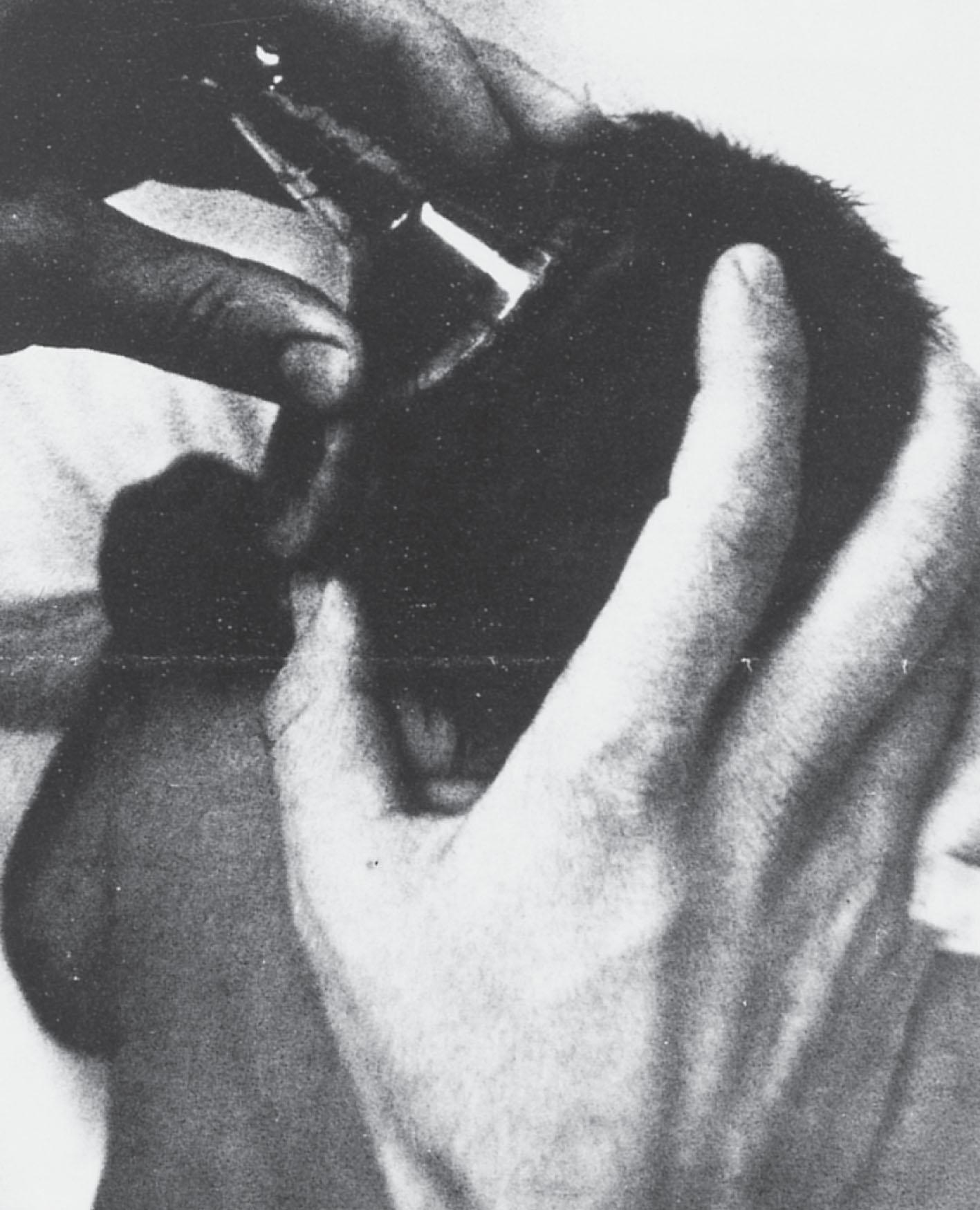
The most reasonable approach to depressed fracture is careful radiological assessment of the lesion, including low-dose CT or MRI scan, or both, to rule out the presence of extradural or subdural clot or bone fragments, and careful neurological surveillance to ensure that acute complications do not develop. This approach could then be followed by a trial of the nonsurgical modalities noted previously. If the latter is unsuccessful, consideration of neurosurgical intervention is then appropriate. However, small, uncomplicated “ping-pong” fractures, on the basis of current information, do not seem to warrant prompt neurosurgical intervention.
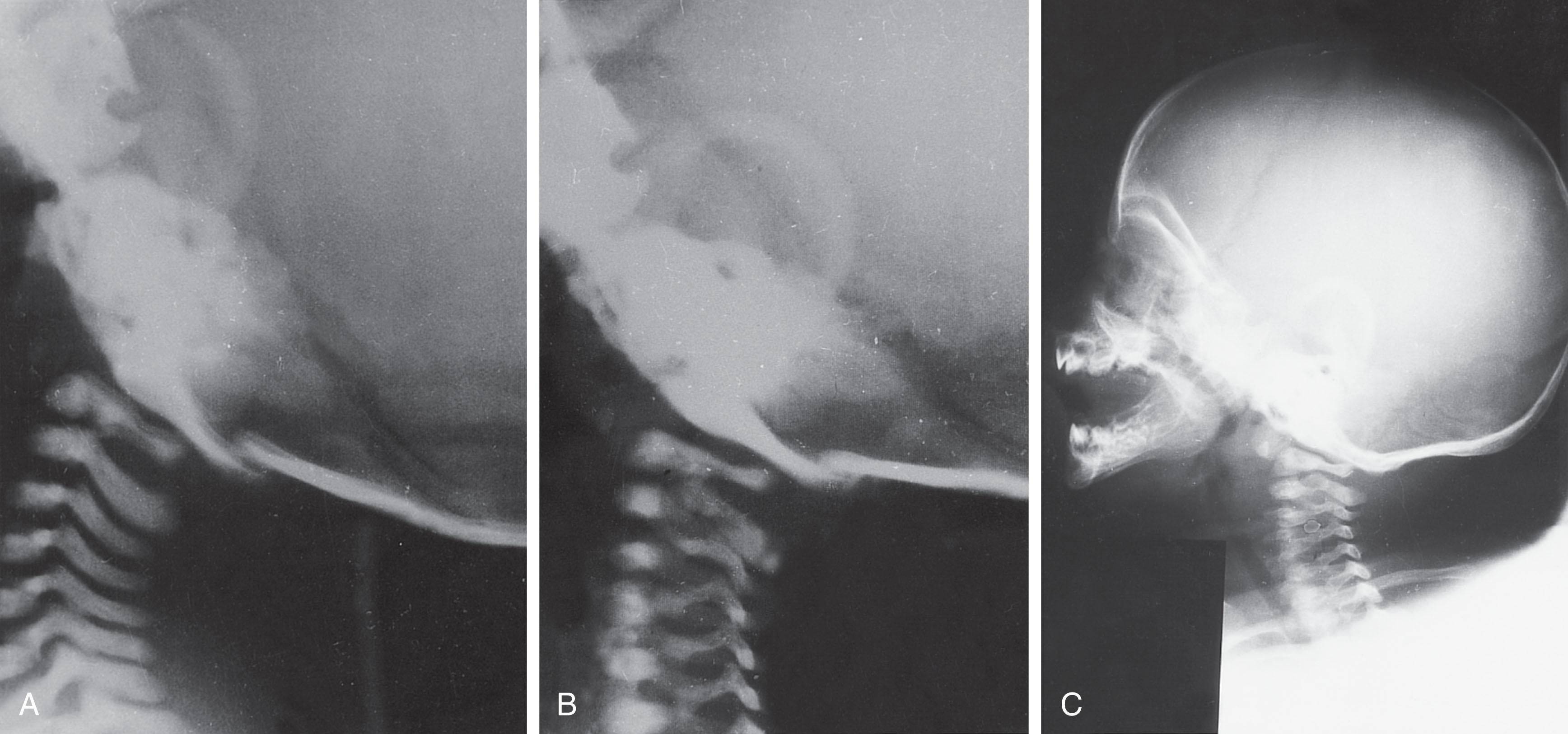
Occipital osteodiastasis, separation of the squamous and lateral parts of the occipital bone, may result in posterior fossa subdural hemorrhage, cerebellar contusion, and cerebellar-medullary compression without hemorrhage or gross contusion. The evolution of the lesion by skull radiography is shown in Fig. 40.9 . Its consequences are discussed primarily in Chapter 27 .
The major varieties of intracranial hemorrhage associated with cranial trauma in the perinatal period include epidural hemorrhage, subdural hemorrhage (acute, subacute, and chronic), primary subarachnoid hemorrhage, subpial hemorrhage, intraventricular hemorrhage, intracerebral hemorrhage, and intracerebellar hemorrhage (see Table 40.1 , Fig. 40.10 ). Pathogeneses other than trauma play more important roles in several of these varieties of intracranial hemorrhage. Trauma appears to play the dominant pathogenetic role in epidural and subdural hemorrhage and may contribute to pathogenesis of the other varieties of intracranial hemorrhage. Except for epidural hemorrhage, now a rare lesion, the neuropathology, clinical features, management, and other features of neonatal intracranial hemorrhage are discussed in detail in Chapter 26, Chapter 27, Chapter 28 .

Epidural hemorrhage refers to hemorrhage in the plane between the bone and the periosteum on the inner surface of the skull (see Fig. 40.10 ). It represents the intracranial analog of a cephalhematoma (which is often associated).
Epidural hemorrhage is a rare lesion in the newborn and constitutes only about 2% of all cases of neonatal intracranial hemorrhage observed at autopsy. This relative rarity may relate to the fact that in the newborn the dura is unusually thick and largely contiguous with the inner periosteum.
Bleeding into the epidural space is derived either from branches of the middle meningeal artery or from major veins or venous sinuses. Fractures across suture lines are likely to be associated with the venous sinuses. Linear skull fracture is present in the majority of cases but not all. Cephalhematoma is also a frequent accompaniment.
When epidural hemorrhage is accompanied by linear skull fracture, overriding of fracture segments and tearing of branches of the middle meningeal artery or a large venous sinus are the probable reasons for the hemorrhage. In the infant without fracture the reason for the hemorrhage is unclear. The dura can be separated from the bone when “the skull is bent inward or outward” at autopsy, and it is possible that this separation in vivo could cause tears of arteries running in the richly vascularized dural-periosteal layer of the neonatal cranium. Several cases have been associated with neonatal in-hospital falls.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here