Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Discuss anatomy of the neonatal hip
Describe normal movements of the hip
Describe sonographic evaluation of the neonatal hip, including technique and protocol
Describe the normal sonographic appearance of the neonatal hip
Describe the sonographic evaluation of the neonatal hip for developmental displacement of the hip
Define the Barlow and Ortolani maneuvers
Differentiate between subluxation of the hip and dislocation of the hip
Sonographic evaluation of the neonatal hip allows for a dynamic view of the soft tissues and cartilaginous structures, with the added advantages of being low cost and free from ionizing radiation, contrast media, and sedation. It plays an important role in the diagnosis and management of developmental displacement of the hip (DDH) in the infant, which is among one of the most common causes of disability in children. Sonography can also easily detect fluid within the joint space, providing clinicians a quick way to assess for joint effusions or septic arthritis in the child with a painful hip.
Until the femoral head ossifies around 4 to 6 months of age, sonography is optimal for evaluating DDH in the neonatal/infant hip compared with other imaging modalities. Although magnetic imaging can provide excellent anatomic detail of the hip anatomy in the young infant, it does not capture live movement of the hip joint, requires a long scanning period, is expensive, and requires sedation. Computed tomography is also non-dynamic and requires gonadal ionizing radiation and sedation but may be helpful in infants confined to a cast. Radiography, although it was originally used to diagnose DDH in young infants, is not reliable in detecting the soft cartilaginous structures of the hip, not yet ossified in this population.
This chapter provides the necessary anatomy, sonographic findings, and techniques to better assess the hip conditions for which sonography offers advantages over other imaging modalities: (1) developmental dislocation or dysplasia of the hip, which is seen in the first 6 months of life, and (2) hip pain, which is seen in the young child and may be caused by inflammatory or traumatic conditions.
The anatomy assessed in the pediatric hip consists of the bony pelvic girdle, superior portions of the femur, hip joint (including the acetabulum and acetabular labrum), and supporting ligaments and muscles.
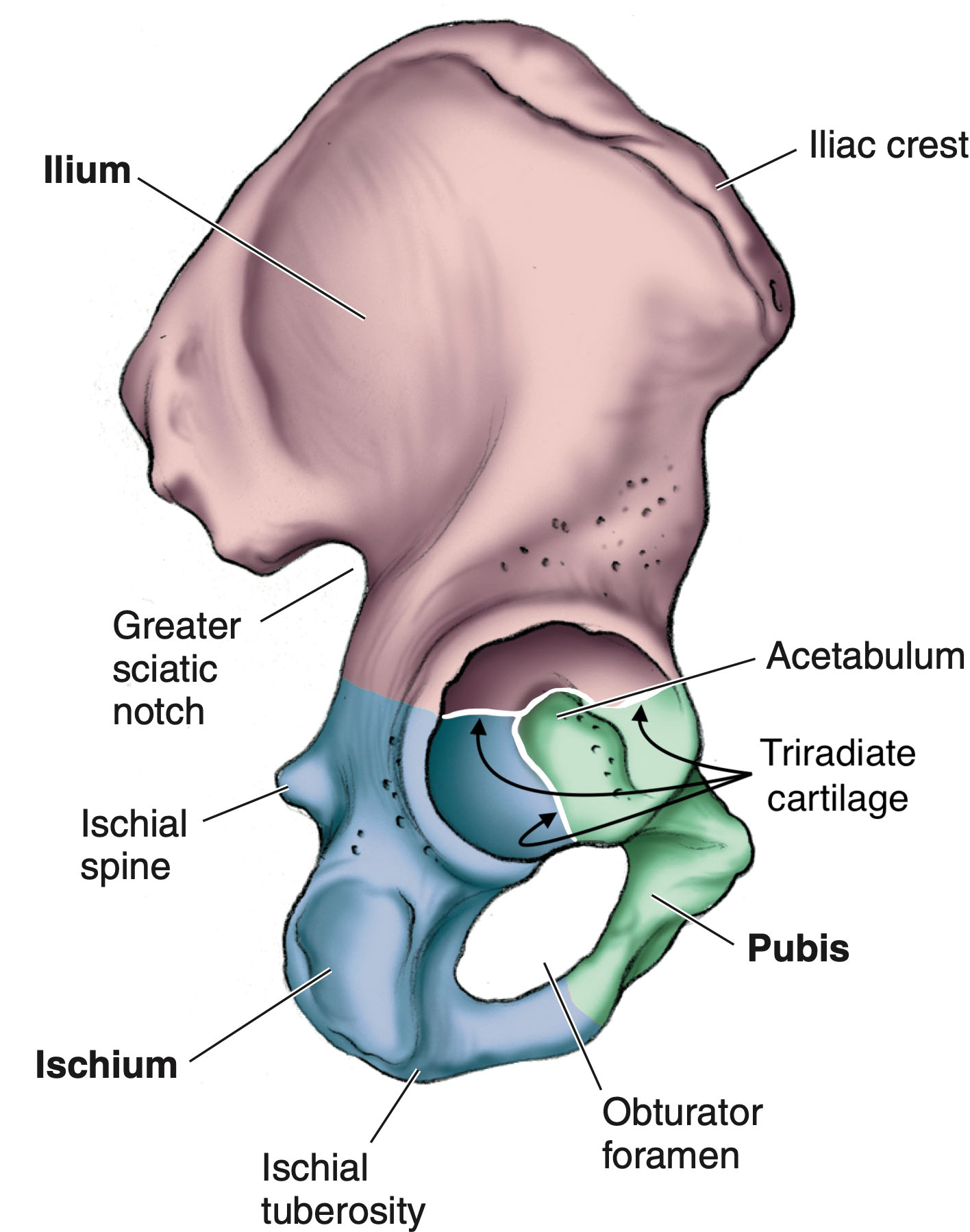
The bony pelvis is a ring-like bony structure composed of two hipbones (or pelvic bones), the sacrum, and the coccyx. The sacroiliac joints unite these two hipbones with the sacral part of the vertebral column. The pubic symphysis is where these two hipbones unite with each other anteriorly. The two hipbones (also referred to as the pelvic girdles or hip girdles) serve as attachment sites, one for each side of the lower limbs, to the axial skeleton. Each pelvic girdle is made up of a single hip (or coxal) bone and, collectively, may be referred to as the innominate bones or os coxae. The pelvic girdle is ossified at birth and consists of three joined bones, individually identified as the ilium, ischium, and pubis.
Within the pelvic girdle, these bones join and form the bony acetabulum. The acetabulum makes up the hip socket and is normally a deep, cup-shaped structure. In childhood, the triradiate cartilage connects these three bones and is made of three distinct growth plates, or physes, that do not ossify until around puberty. The cartilage, once ossified, becomes part of the adult bony acetabulum, or hip socket ( Fig. 28.1 ).
The bone of the upper thigh is the femur, which is surrounded by muscles, ligaments, and tendons. The upper part of the femur, the head, articulates with the hipbone to make the hip joint ( Fig. 28.2 ). The shaft (or diaphysis) of the femur is ossified at birth and sonographically appears hyperechoic, casting an acoustic shadow.
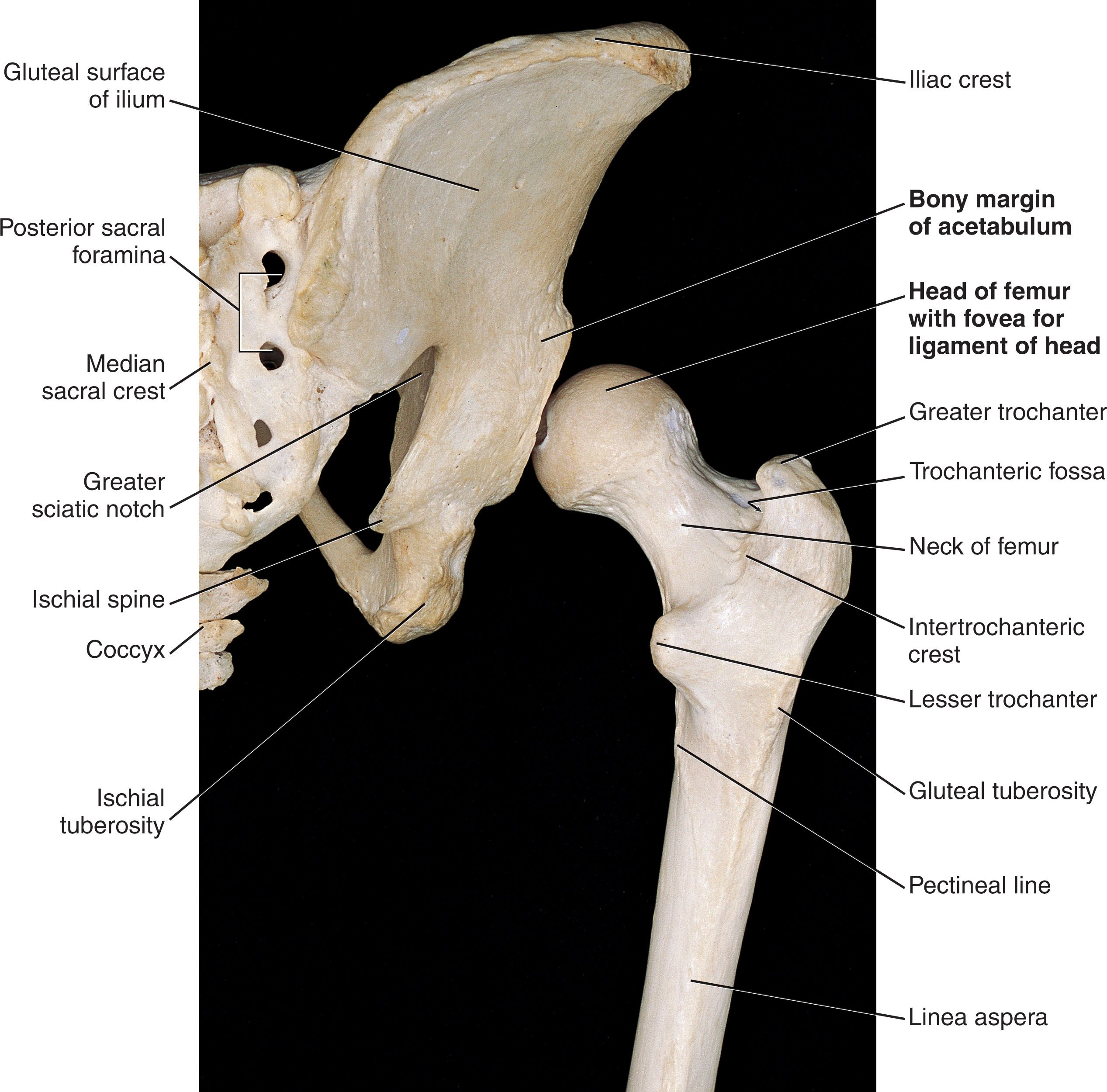
The greater and lesser trochanters, as well as the neck and head of the femur, are cartilaginous at birth and seen well with sonography. The greater trochanter sits superolateral, whereas the lesser trochanter projects from the posteromedial proximal femoral shaft. The neck of the femur tapers medial, superior, and anterior toward the femoral head.
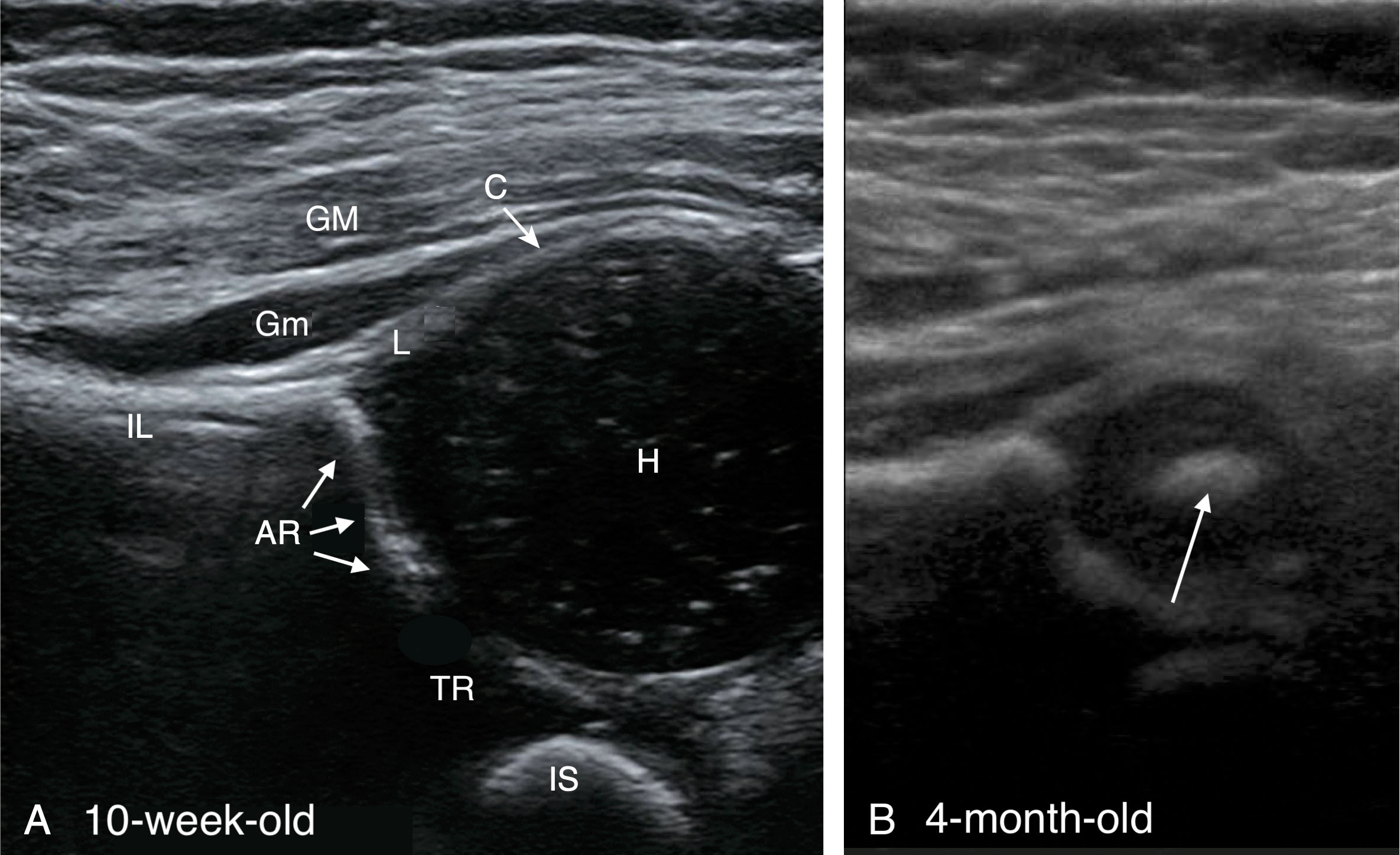
The femoral head appears as a large hypoechoic circle and typically ossifies between 3 and 8 months of age. Ossification begins centrally (which may be seen as early as 2 to 4 weeks of age), with girls often showing earlier ossification than boys. The sonographic value in evaluating the hip greatly decreases as the femoral head ossifies. Ossification as the infant ages, combined with structures located deeper in the body, equates to a substantial diminishment in image quality around 4 to 6 months of age. Once the femoral head is completely ossified, it is difficult to obtain adequate sonographic images because of the beam artifact interference ( Fig. 28.3 ). Radiography is the preferred modality after 4 to 6 months of age unless the acetabulum and triradiate cartilage can be adequately identified with ultrasound.
The rounded femoral head and the cup-shaped bony acetabulum form the freely movable “ball-and-socket” hip joint . The hip joint is not directly palpable because it is surrounded and protected by muscles of the upper thigh. The greater trochanter of the femur forms a palpable knob at the side of the region.
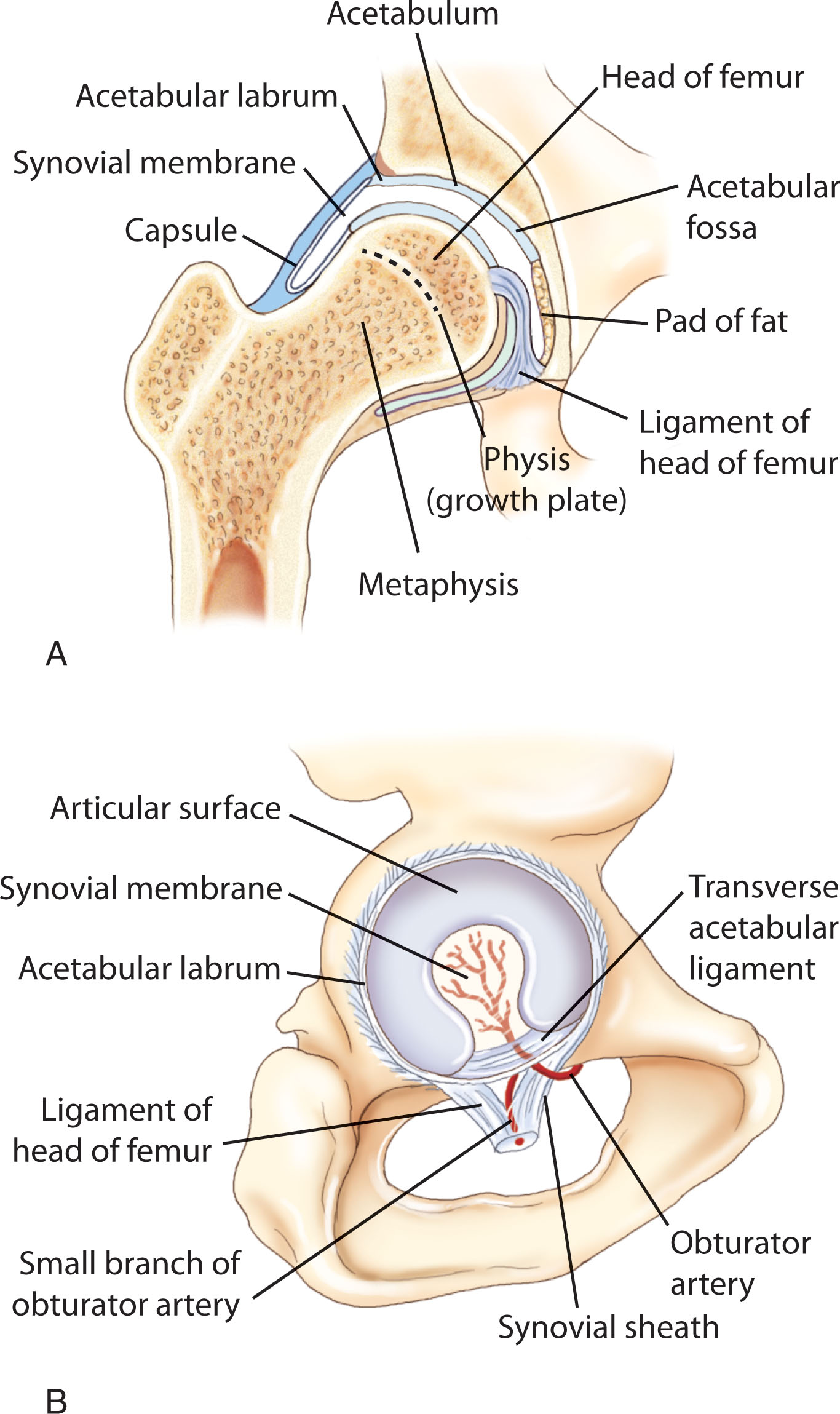
Within the hip joint, the bony acetabulum has a smaller articular surface than the femur’s articular surface and is often referred to as the bony acetabular roof . The acetabulum is made deeper by a rim of cartilage that surrounds it, called the acetabular labrum . The labrum is mostly composed of hyaline cartilage and is hypoechoic, except at the lateral marginal tip, where it changes to fibrocartilage and appears echogenic and triangular. Furthermore, this lateral margin forms an extension of the acetabular roof (often referred to as the cartilaginous roof ). The acetabular labrum narrows the acetabulum and increases its depth, functioning to stabilize and support the femoral head articulation within the acetabulum. Normally, the labrum, or cartilaginous acetabulum, covers two-thirds of the femoral head. Sonographically, the labrum is best depicted from a coronal view and appears superolateral to the femoral head, adjacent to the ilium. Both the bony and cartilaginous roofs are evaluated and may be measured.
The acetabular notch is a bony deficiency at the inferior portion of the central acetabular depression and is covered by a band of fibrous tissue called the transverse acetabular ligament. The ligamentum teres of the femur runs from this acetabular notch through a foramen to the pit or fovea in the head of the femur, through which nerves and blood vessels pass. In the younger child, this ligament contains the branch of the obturator artery to supply the femoral head. The artery usually disintegrates by 7 years of age ( Fig. 28.4 ).
Within the hip joint evaluation, the triradiate cartilage is a useful landmark, lying posterior to the femoral head, and appears hypoechoic in the neonate. The posterior rim of the acetabulum, part of the triradiate cartilage in the immature skeleton, is often referred to as the posterior lip .
The hip joint is surrounded by a tough capsule , which attaches to the intertrochanteric line of the femur and is reinforced by outside ligaments and muscles. This fibrous capsule covers the labrum and appears sonographically to extend from it inferiorly. The psoas tendon crosses the center of the hip joint just inferior to the inguinal ligament. The iliacus muscle sits lateral to the psoas tendon and, along with the psoas muscle, flexes the hip.
The most important hip ligament is the iliofemoral ligament, which passes from the anterior inferior iliac spine to each end of the intertrochanteric line. It is one of the strongest ligaments in the body and is very important for standing and maintaining correct upright balance.
The large gluteus maximus muscle overlies other muscles superior and posterior to the hip joint. The gluteus maximus is a powerful extensor of the hip. The gluteus minimus muscle is the immediate cover for the upper part of the hip joint. The gluteus medius and gluteus minimus pass from the outer surface of the hipbone to the greater trochanter. Together they act as abductors of the hip joint. Their most important function is to prevent adduction and to keep the pelvis level while walking.
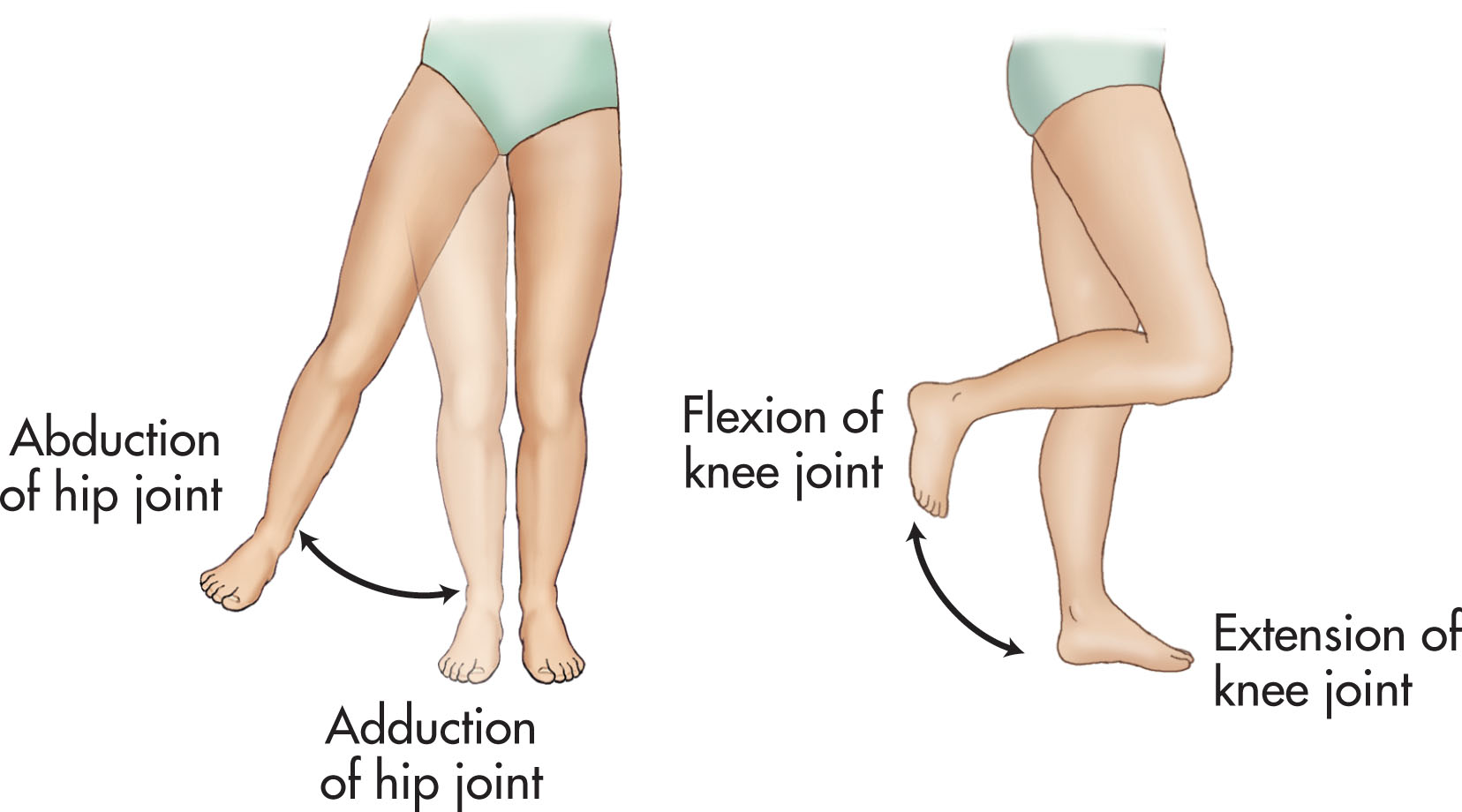
The movements of the hip are somewhat limited in range because of the tight fit between the femur and acetabulum and because the hipbone is immobile. The following are the hip movements and their actions. Note that sonographic evaluation is primarily concerned with the abduction and adduction motions.
Flexion—bending forward
Extension—bending backward
Abduction—moving sideways outward
Adduction—moving sideways inward
Medial rotation
Lateral rotation
Flexion (bending forward) and extension (bending backward): The primary flexors of the hip are the psoas major, iliacus, and rectus femoris. Extension is limited to 20 degrees and is brought about by the hamstrings and gluteus maximus.
Adduction (moving sideways inward) and abduction (moving sideways outward): An example of hip adduction is crossing your legs when in a seated position, an action performed by the adductor group of muscles. In abduction, the gluteus medius and minimus muscles open the limbs. The more important function of these muscles, however, is to prevent adduction, which is the function they perform when walking ( Fig. 28.5 ).
Medial and lateral rotation is related to the angle at which rotation occurs at the head of the femur, which is about 120 degrees angle to the shaft of the femur. When the trochanter moves forward, the femur rotates medially, and when the trochanter moves backward, the femur rotates laterally. Thus, the medial rotators are the anterior fibers of the gluteus medius and minimus. The lateral rotators are the small muscles at the back of the joint: piriformis, obturator internus, and quadratus femoris, with assistance from the gluteus maximus.
Sonography is the preferred imaging modality in the detection of DDH in infants. It is more sensitive than the physical examination and has been shown to change the diagnosis in over half of cases. Furthermore, it has changed the management plan in one-third of cases in infants presenting to pediatric orthopedist surgeons for suspected DDH. Given its ability to detect this condition, universal screening sonography has been recommended and implemented in some places. Unfortunately, screening has not been shown to decrease the rate of late diagnoses.
The most important factor influencing the outcome is the age at which the diagnosis is made and treatment initiated. Treatment should begin before the patient walks, and an early diagnosis is vital so that treatment can be instituted as early as possible. Currently, selective screening sonography is indicated in infancy after the neonatal period; if the physical examination is abnormal or unequivocal, risk factors, associated congenital anomalies, or neuromuscular conditions are present; or if there is a need to evaluate the response to treatment, often a Pavlik harness. Risk factors include female sex, breech presentation, oligohydramnios, or a family history of DDH.
The ultrasound examination may be repeated as often as necessary to follow the progression of treatment. However, if the patient is in a harness, do not remove the harness unless instructed to do so by the ordering physician or orthopedic doctor. Infants are often examined in the harness, and the stress maneuvers are not performed.
Sonography for DDH is practical for most infants from 4 to 6 weeks up 4 to 6 months of age. Exceptions may include older infants if the femoral head is not yet ossified. Neonates are not typically evaluated, and infants should be at least 44 gestational weeks of age, adjusted for prematurity. Typically, after 4 to 6 months of age, radiography is the preferred imaging modality.
The sonographic examination for DDH moves through a series of images in the coronal and transverse planes, taken at rest and with stress, allowing the sonographer to assess the position and stability of the femoral head in the hip joint.
Stability of the hip is determined through the guided motion and application of gentle stress. These gentle “push-pull” stress movements are the imaging counterparts of the Barlow (adduction) and Ortolani (abduction) physical screening maneuvers. Stability testing is reported as normal, lax, subluxable, dislocatable, and reducible or irreducible.
Position of the hip is determined by the degree to which the femoral head is covered by the labrum, as well as the position of the femoral head in the acetabulum. The sonographic appearance of the femoral head location is described as normal, subluxed, or dislocated.
Additionally, the development of the bony and cartilaginous acetabulum is sonographically described as normal, immature, or dysplastic.
Ideally, validation of the femoral head position is achieved through measurements quantifying the amount of femoral head coverage. Likewise, the acetabular morphology is assessed with drawn angles, which correspond to the degree of the bony acetabulum (alpha angle) and the labrum or cartilaginous acetabulum (beta angle).
To achieve a satisfactory examination, the infant should be relaxed and as comfortable as possible. Parental assistance is helpful to keep the infant calm. Having them stand on the opposite side of the bed allows the parent to be near the infant’s head. Feeding before or during the examination helps to soothe the infant. Make sure the room is warm, and keep blankets close for warmth. Toys and other distractions help to quiet the infant so that the examination may be performed.
Sonography of the neonatal hip is performed with a high-frequency linear-array transducer, often a 10 to 12 MHz ( Box 28.1 ). Sector or curved-array transducers will distort anatomy and are not recommended. This examination is always performed on both hips. Because ambidextrous scanning (commonly with the aid of a foot pedal) is a requisite, the sonographer often requires a good amount of experience before feeling fully competent. Scanning with the dominant hand first may be helpful. The right hip is examined with the transducer in the sonographer’s left hand and vice versa. The opposite hand is used for manipulation of the hip being examined, while a foot pedal comes in handy to freeze and capture images without having to constantly reposition the infant.
Premature infants: 12–15 MHz
Average-sized infant ≤3 months: 9–12 MHz
Infants 3–7 months: 6–9 MHz
The infant is placed in a supine or decubitus position perpendicular to the table with the feet toward the sonographer. In a decubitus view, rolled towels, bolsters, or even specialized cradles may help keep the child on his or her side. It is wise to leave the diaper on through the examination and expose only the side of the hip being examined.
The basic hip anatomy may be imaged in four different views. A two-word combination labels the view by both the plane of the body (coronal or transverse) and hip position (neutral or with flexion). While institutions may vary on which ones are performed, they include (1) coronal/neutral, (2) coronal/flexion, (3) transverse/neutral, and (4) transverse/flexion. Next, dynamic stress maneuvers from the flexed transverse position are then often performed. A coronal posterior lip view with stress may also be obtained. In the setting of pathology, a 3D acquisition of the coronal views is possible. Finally, measurements for a quantifiable evaluation are obtained from the coronal view(s) and may be performed by either the sonographer or radiologist, preferably by the latter.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here