Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Induction of labour, which is defined as the process by which labour is started (or attempted) prior to its spontaneous onset leading to active labour and birth, is one of the two options available to women and their caregivers when the continuation of a pregnancy poses a greater risk to either the mother or the fetus than the consequences of interrupting the pregnancy; the remaining option being caesarean section. As such, induction of labour is an essential intervention that is employed on a daily basis throughout the world. In the UK, there is an abundance of national guidance regarding induction of labour from the National Institute for Health and Care Excellence (NICE) and the Royal College of Obstetricians and Gynaecologists (RCOG), to which the reader is referred via the respective websites.
Induction of labour dates back to antiquity, and various methods, many bizarre and some extremely dangerous, have been employed. Some very early methods have since been shown to have some scientific basis, whereas others bordered on witchcraft. Literature from the 16th century contains long lists of ‘medications’ said to be effective in stimulating labour, including juniper berries, castor oil, cinnamon, white amber in white wine and many others. In 1735 Dr Henry Bracken recommended ‘some softening, unctuous application such as sweet almonds be applied warm with a brush of feathers to the privities and vagina’ in his text Midwives Companion – wherein the Whole Art is Explained. Massage of the breasts has been employed for centuries, as the relationship between breast and uterus, via oxytocin, has long been appreciated, and even now some still employ a modification of this technique for induction of labour in the form of breast massage and nipple stimulation with some degree of success. Insertion of various objects into the cervix has been utilized for induction as far back as the 6th century when Aetius inserted cervical sponges to induce labour following intrauterine death. The 1800s saw the introduction of other mechanical methods of induction. Kraus’s bougies were introduced on a wide scale. These were used to forcibly dilate the cervix, separate the membranes from the uterine wall high up into the uterine cavity, after which the bougie was left in place until labour ensued – a method used for many years, but which has now fortunately been laid to rest because of its relative inefficiency, sepsis rate, and the not insignificant risk of injury to the placenta. Cohen described the injection of fluid under the fetal membranes in 1846, a method which was reinvestigated in the 1990s. Laminaria have also been used since the 1800s and their use has seen a recent resurgence. Another mechanical method previously employed which again has seen an increase in popularity is the use of a balloon catheter inserted through the cervix into the lower uterine segment and inflated. It appears that any success related to these mechanical methods may be secondary to the release of prostaglandins following the mechanical disruption of the tissues, as is almost certainly the case in sweeping of the membranes. Another ancient method was the use of ecbolics, which have been used throughout history for abortion as well as induction of labour. The ingredients and methods of administration have varied throughout the years, but the ‘medical induction’ regime used most recently was standardized by Watson in the 1920s, more recently referred to as the OBE, and consisted of oral castor Oil followed by a hot Bath and a soap and water Enema, which was said to be ‘high, hot and a hell of a lot’. This practice ceased in the past few decades with the advent of more successful and less unpleasant methods of induction. Other forms of medical induction were tried, all with limited success. Towards the end of the 1800s quinine was used successfully to induce labour but the detrimental effects on the fetus were recognized and this method therefore fell from favour, although its use in intrauterine death persisted for some time. In the 1900s, various other substances were tried, with inconsistent and often unconvincing results. These included oestrogens, urea, hyaluronidase, steroids, relaxin and sparteine, to name a few. However, the three major methods of induction of labour that have stood the test of time in terms of acceptability, safety and efficacy are amniotomy, intravenous oxytocin and prostaglandins, although mechanical methods in the form of cervical balloons and laminaria are seeing a resurgence.
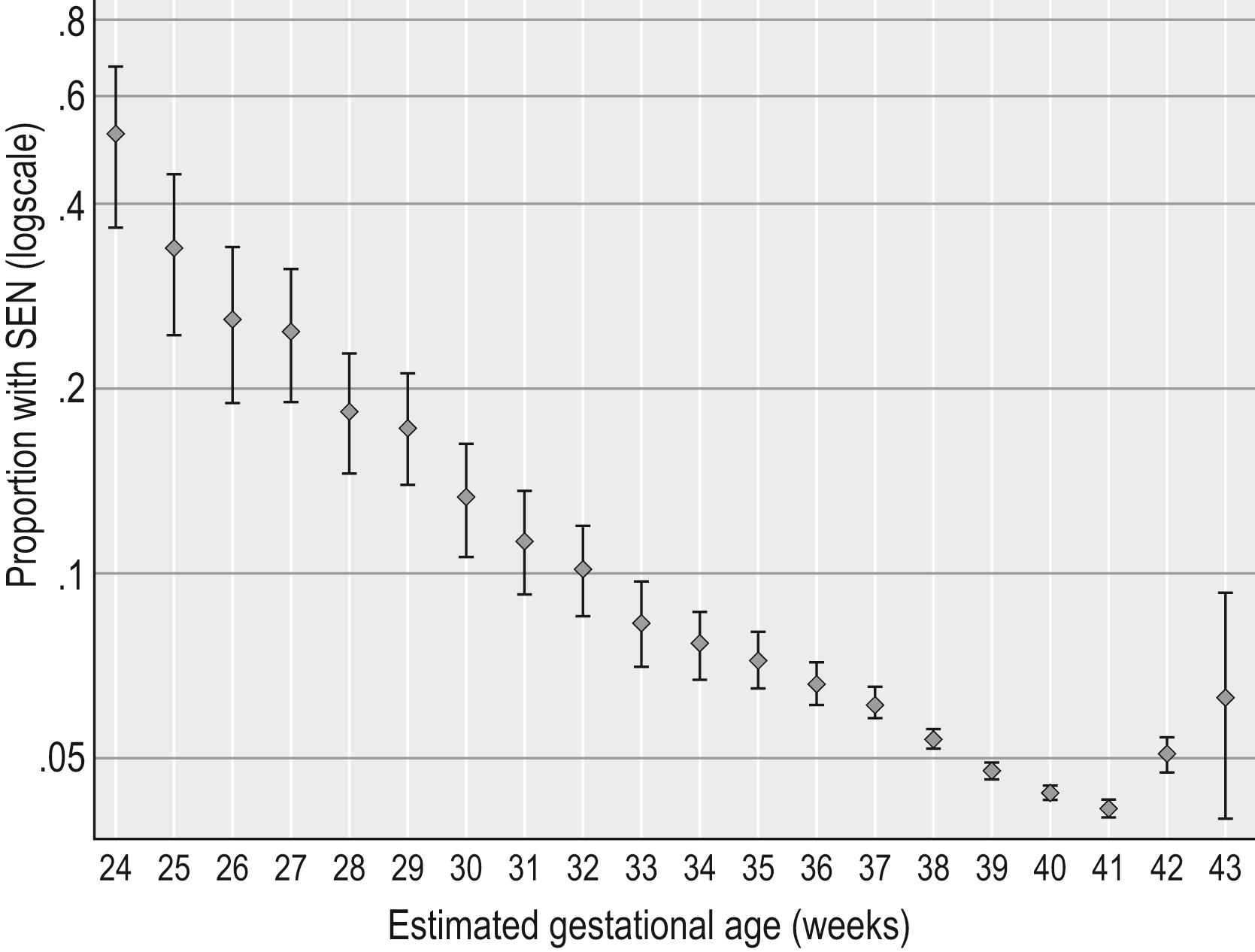
When considering any intervention, it is important to be clear about the balance between risks and benefits ( Fig. 7.1 ). With induction of labour, the objective is safe vaginal birth, and the intended benefit on the whole is avoidance of perinatal and/or maternal morbidity and mortality. The risks and benefits are often different for the mother and the baby and as such need to be balanced against each other. If delivery is advocated to reduce maternal risk, the proposed benefit must be weighed against any risks associated with the induction process, including but not limited to potentially increasing the risk of caesarean section, including both immediate risks and those in subsequent pregnancies. For the fetus/baby, the proposed benefit is often avoidance of stillbirth or significant morbidity, but the risks include the consequences of early delivery, both short and long term. In the short term, induction of labour prior to 41 weeks’ gestation is associated with an increased risk of admission to a neonatal facility. In addition, fetal brain development continues throughout pregnancy, and population data demonstrate that the risk of a child having special educational needs (SEN) is lowest in those delivering at 40–41 weeks gestation ( Fig. 7.2 ). After adjusting for maternal and obstetric characteristics and expressed relative to delivery at 40 weeks, when the subsequent risk of SEN was 4.4%, the risk of SEN was increased by 36% (95% confidence interval [CI] 27–45%) at 37 weeks, by 19% (95% CI 14–25%) at 38 weeks and by 9% (95% CI 4–14%) at 39 weeks. Because of these risks, it is important not to offer early delivery to pregnancies not at increased risk, or where the risks of early delivery outweigh the benefits.
When trying to balance these risks and benefits for both the mother and the baby, many factors need to be taken into consideration. Firstly, the evidence confirming benefit of early delivery is not translatable from one group to another, and evidence of benefit is often absent or weak. For example, it is common practice to offer induction of labour to women who present with reduced fetal movements (RFM) at term. In the AFFIRM trial, which assessed the introduction of a care package for women with RFM with a reduction in stillbirth as the primary outcome, the intervention did not reduce the incidence of stillbirth but did increase the rates of induction of labour and caesarean section, and was associated with an increased risk of prolonged neonatal unit admission: essentially the benefit was not realized but the risks were increased. From the baby’s perspective, delivery removes the risk of stillbirth but, as discussed above, early delivery carries different risks, and it is important to consider the risk to the baby of the pregnancy continuing in that particular situation against the known short-term and long-term risks of early delivery, which change with gestation. It is important, therefore, that timing of intervention also needs to be considered both in terms of risk and successful induction.
With regards to success (safely achieving a vaginal birth), the two main factors which influence this are a history of a previous vaginal birth and the cervical score ( Table 7.1 ). If a woman has delivered vaginally in the past, the chance of vaginal birth following induction is high, whereas in nulliparous women and those with a previous caesarean section the incidence of caesarean section is generally increased. The cervical score reflects how close the woman is to spontaneous labour, and the chance of successful induction is positively correlated to the cervical score. These factors should also, therefore, be taken into account when discussing the risks and benefits of induction in terms of the likely outcome, as in some cases the decision to deliver may be deferred based on the chances of success weighed against the actual risk of prolonging the pregnancy, or the decision may be to perform a caesarean section rather than aim for vaginal birth.
| Cervical Score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Dilatation (cm) | <1 | 1–2 | 2–4 | >4 |
| Length of cervix (cm) | >4 | 2–4 | 1–2 | <1 |
| Station (cm) | −3 | −2 | –1/0 | +1/+2 |
| Consistency | Firm | Average | Soft | – |
| Position | Posterior | Mid; anterior | – | – |
It is accepted that induction of labour has an impact on the birth experience of women. It may be less efficient and is usually more painful than spontaneous labour, and epidural analgesia and assisted delivery are more common when compared with spontaneous labour. A major concern with induction of labour has been the perceived increase in caesarean section rates following induction, although there is now evidence that in certain groups this is not the case, with some trials showing no increase or a reduction in caesarean section rates. The recent publication of the ARRIVE trial has created much discussion regarding timing of induction of labour, having found that planned induction of labour at 39 weeks’ gestation in low-risk pregnancies was associated with a reduced incidence of caesarean section (18.6% vs. 22.2%; relative risk [RR] 0.84; 95% CI 0.76–0.93), although the trial did not demonstrate any difference in the primary outcome of composite perinatal morbidity, i.e. the trial showed no evidence of benefit to the baby. Importantly, long-term outcomes for the baby were not assessed and the impact of early delivery on long-term outcomes for the baby is therefore unknown. Based on the outcome of this study, the American College of Obstetricians and Gynecologists issued a Practice Advisory statement that
‘it is reasonable for obstetricians and health-care facilities to offer elective induction of labor to low-risk nulliparous women at 39 weeks gestation. However, consideration for enactment of this elective induction of labor intervention should not only take into account the trial findings, but that this recommendation may be conditional upon the values and preferences of the pregnant woman, the resources available (including personnel), and the setting in which the intervention will be implemented’.
It should be noted that the trial took place in the USA where practice is different, and the results may not translate to the UK. Before the results of these studies are applied to all women, further evidence is needed to determine benefit in all groups of women and, more importantly, to assess the long-term outcomes for the baby.
For all these reasons, the most important decision is not how to induce labour, but whether early delivery is warranted. In order to ensure that women are aware of the risks and benefits as they apply to their individual case, results from one group of women must not be extrapolated to other groups, and we must ensure, where possible, that we can give accurate individualized information to women to enable them to make informed choices about intervention in their particular circumstances, especially as post-Montgomery there have been cases of litigation for unnecessary induction of labour. People perceive and interpret risk differently, and our role as practitioners is to present the evidence and its limitations to women in an understandable way to enable them to make an informed decision regarding their care ( Table 7.2 ).
| Maternal Benefits | Maternal Risks | Baby Benefits | Baby Risks | Other Factors to Consider |
|---|---|---|---|---|
| Lower morbidity from existing medical conditions exacerbated by pregnancy | Hyperstimulation | Avoidance of stillbirth | Neonatal unit admission | Accurate gestational age |
| Lower risk of pre-eclampsia | ?CS – short- and long-term risks of CS | Reduced risk of infection if ruptured membranes at term | Increased rates of neonatal jaundice | Parity |
| ?Reduced risk of CS – short- and long-term risks of CS | Increased pain | Reduced risk of shoulder dystocia and fractures in big babies | Lower cognitive function with early term delivery compared with late term delivery | Previous CS |
| ?Less vaginal trauma as baby smaller | Uterine rupture | Increased frequency of special educational needs with early term delivery compared with late term delivery | Cervical score | |
| Increased operative vaginal birth | Higher rates of hospital admissions in childhood with early term delivery compared with late term delivery | Organizational ability to facilitate induction | ||
| Increased risk of PPH | ||||
| Increased epidural use | ||||
| Failed induction | ||||
| Poorer birth experience | ||||
| Delays in care |
In 2011 the World Health Organization published recommendations for induction of labour, which included the following general principles:
Induction of labour should be performed only when there is a clear medical indication for it and the expected benefits outweigh its potential harms.
In applying the recommendations, consideration must be given to the actual condition, wishes and preferences of each woman, with emphasis being placed on cervical status, the specific method of induction of labour and associated conditions such as parity and rupture of the membranes.
Induction should be performed with caution since the procedure carries the risk of uterine hyperstimulation and rupture and fetal distress.
Whenever induction of labour is carried out, facilities should be available for assessing maternal and fetal wellbeing.
Women receiving oxytocin, misoprostol or other prostaglandins should never be left unattended.
Failed induction of labour does not necessarily indicate caesarean section.
Wherever possible, induction of labour should be carried out in facilities where caesarean section can be performed.
Figures from the National Maternity Dataset (England) in 2018 show that over 30% of women now have their labour induced, compared with around 20% 10 years ago. This is because of changes in national guidance in a variety of scenarios in which induction of labour is recommended. In addition, the implementation of the Saving Babies’ Lives Care Bundle (SBLCB) in England has resulted in a significant increase in both induction of labour and caesarean section. These increases are felt to be largely due to fetal growth restriction (FGR) and RFM, and there is concern that some of the intervention prompted by the introduction of the SBLCB is unwarranted with no evidence of benefit. Overall, this substantial increase in the rate of induction of labour has resulted in significant challenges for service delivery, which in turn impacts on the birth experience. There are widespread reports of delays in care regarding induction due to workload, sometimes with disastrous consequences, and staff are regularly faced with trying to prioritize the induction workload based on clinical risk in the absence of a robust tool to individualize actual risk in different cases. Women are often very unhappy with sometimes long delays in the induction process that often sees them in hospital with nothing happening, separated from their families, or waiting anxiously at home for a bed to become available after being told that there are increased risks with continuation of the pregnancy and that induction was therefore indicated. It is therefore extremely important that induction is not embarked upon without a robust indication, as well as taking into account the impact of increased induction rates on a unit’s ability to ensure a safe service for all.
The indications for induction are many and varied. Traditionally the most common reason was prolonged pregnancy, but increasingly growth restriction and diabetes, amongst others, prompt induction. The evidence supporting these clinical indications is of variable quality and at times there is no evidence to inform our clinical decision-making. However, in such cases the balance is between the known risks of induction of labour with the uncertain and unpredictable risks of complications in a continuing pregnancy, in particular the risk of stillbirth and its devastating consequences for the individual families.
The evidence regarding prolonged pregnancy is robust. A Cochrane systematic review was updated in 2018 to include 33 studies including 12,479 women. Induction of labour before 42 weeks’ gestation was associated with reduced perinatal morbidity as well as reduced risks of stillbirth and caesarean section. There was no difference in length of hospital stay or postpartum haemorrhage. NICE recommends that women with uncomplicated pregnancies should be offered induction between 41 +0 and 42 +0 weeks. Those women who decline induction after 42 weeks should have twice-weekly cardiotocography (CTG) and weekly liquor volume measurement.
In approximately 3% of women, rupture of membranes occurs at less than 37 weeks’ gestation. Routine induction of labour before 37 weeks is not recommended unless there are specific indications such as infection or suspected fetal compromise, as the risks of preterm birth outweigh the risks of infection. After 37 weeks it is recommended that the risks to mother and baby along with the availability of local facilities are discussed before making a decision regarding induction. In this situation, expectant management is associated with a small increase in the risk of infection with no significant differences in caesarean section rates or overall perinatal or neonatal outcomes. The RCOG Green-top Guideline on early onset group B streptococcal (GBS) disease is concordant with this NICE guidance. It recommends that at less than 34 weeks’ gestation, the risks of preterm delivery outweigh risks of infection even in known carriers of GBS; however, at more than 34 weeks it may be of benefit to consider delivery in women colonized with GBS, although evidence is not robust and care should therefore be individualized. If induction is carried out under 37 weeks, intrapartum antibiotic prophylaxis (IAP) for GBS should be administered.
Approximately 8–10% of women experience spontaneous rupture of the membranes at or beyond 37 weeks, and 60% of these will go into spontaneous labour within 24 hours. NICE guidance recommends that these women are offered either immediate induction or delayed induction (for 24 hours) to reduce the risk of neonatal infection, unless there is known GBS, in which case immediate IAP should be offered with induction as soon as possible. A Cochrane systematic review of 12 trials including 6814 women concluded that immediate induction compared with expectant management up to 96 hours in prelabour rupture of membranes at 37 weeks and beyond was associated with reduced risks of chorioamnionitis (226/3300 vs. 327/3311; RR 0.74; 95% CI 0.56–0.97) and endometritis (5/217 vs. 19/228; RR 0.30; 95% CI 0.12–0.74). There was no difference in delivery by caesarean section (333/3401 vs. 360/3413; RR 0.94; 95% CI 0.82–1.08), instrumental delivery (487/2786 vs. 502/2825; RR 0.94; 95% CI 0.82–1.08), or where assessed women were more likely to be happy with their care in the immediate delivery arm. At term, women who are known to be GBS positive should be offered immediate IAP and induction as soon as possible. This is based on the findings of the Term PROM trial which randomized women with rupture of membranes at term to either induction or expectant management. Babies of women with known GBS had three times the odds of neonatal infection compared with women with negative or unknown GBS status (odds ratio [OR] 3.08; P <0.0001). GBS status was the second most important predictor of neonatal infection after clinical chorioamnionitis. In women without confirmed GBS colonization, national guidance recommends offering immediate induction or delaying by 24 hours, based on increased risks of neonatal infection when delivery was delayed by 24–48 hours compared with <12 hours (OR 1.97; P =0.02) and a greater risk of infection when delayed by >48 hours (vs. <12 hours OR 2.25; P =0.01).
It is well established that FGR and small for gestational age (SGA) are two different entities, and that FGR is associated with a significantly increased perinatal mortality rate compared with SGA. Thus any ambition to reduce perinatal mortality must include strategies to accurately identify those fetuses with FGR, to facilitate timely delivery to reduce the well-established risk of intrauterine death. The difficulty comes with identifying (1) those fetuses that are small and (2) those that are at increased risk and would benefit from early delivery. The introduction of the Saving Babies’ Lives Care Bundle (SBLCB) in England has significantly improved SGA detection rates in England, from 33.8% to 53.7%, and guidance exists to help identify those with FGR and guide timing of delivery. The impending revised SBLCB aims to improve guidance on timing of intervention in SGA/FGR to try and reduce the number of unwarranted inductions in this group. In severe FGR with confirmed fetal compromise, induction should not be offered, as delivery by caesarean section is the intervention of choice.
Fetal movements are a reassuring sign of fetal wellbeing and women are advised to report any change in their pattern, as in numerous confidential enquiries into stillbirth, RFM has been associated with poor perinatal outcome. When a woman presents with RFM, investigation is aimed at confirming fetal viability and then identification of the fetus at risk of adverse outcome, particularly those with FGR, while avoiding unnecessary interventions. The risk of adverse outcome is increased in the presence of recurrent RFM and careful assessment of the fetus is required. The AFFIRM trial showed that induction of labour for recurrent RFM from 37 weeks did not reduce the stillbirth rate but did lead to increased rates of induction and caesarean section, and increased rates of prolonged neonatal admission with no reduction in perinatal mortality. In the absence of any concerns regarding fetal growth and wellbeing, there is no place for induction prior to 39 weeks.
The recommendations regarding timing and mode of birth are dependent on chorionicity, with monochorionic twins having significantly higher odds of stillbirth compared with dichorionic twins from 32 weeks onwards. Women with monochorionic twins should have the timing of birth discussed and be offered induction of labour from 36 +0 weeks with the administration of antenatal steroids, unless there is an indication to deliver by caesarean section or to deliver earlier. In pregnancies with treated twin–twin transfusion syndrome (TTTS) or type I selective growth restriction (sGR) with normal growth velocity and Dopplers, delivery is recommended at 34–36 weeks, with mode of birth being individualized taking other factors such as parity and presentation of the leading twin into account. In uncomplicated dichorionic twin pregnancies, delivery should be offered from 37 +0 weeks, again with mode of birth being individualized, taking other factors such as parity and presentation of the leading twin into account.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here