Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Modern neurosurgical care is a complex, multidisciplinary enterprise, involving a broad consortium of providers and occurring in diverse settings, from preoperative clinics to postoperative rehabilitation facilities. Even so, the operating room (OR) remains the core of neurosurgery. Events in the OR have a profound impact on the patient's outcome and life thereafter.
While modern neurosurgery is remarkably safe and effective, errors in the OR remain common. For example, a prospective study documented one or more intraoperative errors in 93.5% of neurosurgical cases. Other studies showed similarly high rates, ranging from 25% to 85% of neurosurgical cases. While some errors are minor, like dropping a suture needle that is later recovered, others are devastating, like wrong-sided surgery.
Recognizing this importance, countless efforts have been undertaken to improve patient safety in the OR, from checklists to team training exercises. In this chapter, we review these efforts, first describing general strategies for improving safety, and then strategies designed for specific complications, like surgical site infections or pressure ulcers.
A safe surgeon is an experienced surgeon. In most surgical specialties, surgery becomes safer when it is performed more often. This correlation is termed a volume - outcome relationship . Volume-outcome relationships have been demonstrated for nearly all neurosurgical subspecialties: for example, spine, tumor, epilepsy, vascular, and pituitary surgery.
The source of volume-outcome relationships comes partly from improved technical performance by the surgeon, which comes with repeated practice. However, it is not just the surgeon who benefits from high surgical volumes—experience is shared among nurses, technicians, anesthesiologists, administrators, and other staff. The contributions of other staff are a crucial component of volume-outcome relationships, since technical errors by the surgeon comprise only ~ 25% of medical errors in neurosurgery—the remaining 75% of errors involve the rest of the hospital system. In other words, even if a surgeon perfects his or her craft, only 1 of every 4 errors might be prevented.
The acknowledgment that many errors are outside of one individual's direct control is part of systems thinking —to understand complex systems like health care, one must understand not only the various components but also their connections. To improve patient safety, it is not enough to isolate a single component of the system (e.g., the surgeon). The system as a whole should be studied—nurses, anesthesiologists, surgeons, administrators—along with their interactions.
Communication is the most effective means to mitigate systems issues. Poor communication can have dire consequences. For example, some wrong-sided craniotomies have been directly attributed to nurses feeling they could not openly challenge a surgeon's actions. It is therefore incumbent on all OR staff to allow and encourage free communication during surgery. There should be no hierarchy preventing a member of the team from voicing their concerns. For example, a nurse should never feel like he or she cannot speak openly with a surgeon. The OR hierarchy should be flat.
The aviation industry has faced similar problems, with fatal airline crashes attributed directly to hierarchies impeding free communication. The airlines' response, crew resource management (CRM), is a set of techniques designed to foster communication and teamwork within complex systems like aviation and health care. Attention in CRM is directed toward enabling team members to communicate effectively with supervisors and respectfully question their decisions when appropriate. CRM is usually introduced to employees with intensive team training sessions, and includes structured communication practices like briefings, checklists, debriefings, and handoffs—all items that are being studied à la carte as patient safety adjuncts in neurosurgery.
One popular implementation of CRM for health care is Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), developed by the Agency of Healthcare Research and Quality. Though it has not been applied to neurosurgery, the application of TeamSTEPPS in other surgical services resulted in statistically significant reductions in patient safety issues, morbidity, mortality, and case durations. A similar team training program, when tested in over 70 Veterans Affairs hospitals, resulted in a relative 50% reduction in mortality, attesting to the power of systems thinking in protecting patients.
While CRM programs like TeamSTEPPS have numerous components, one of the most important is structured communication. A widespread tool for structured communication is SBAR (Situation, Background, Assessment, and Recommendation), which was originally developed by the military for use on nuclear submarines ( Box 10.1 ). SBAR trains users to first present a major problem concisely, then provide pertinent background information, followed by a provisional assessment of the problem's causes, and lastly a recommended course of action. Numerous communication mnemonics have followed SBAR, all with slight twists (e.g., SHARQ, DeMIST, GRRRR, JustGoNUTS).
Situation —Communication begins by concisely describing the main problem. This orients the listener and helps them process the subsequent details.
Dr. Smith, the patient has become hypotensive and has a reduced end-tidal CO 2 .
Background —After the primary problem is presented, pertinent background information is supplied.
All vital signs were stable until the craniotomy flap was turned. This patient has a known patent foramen ovale.
Assessment —The speaker then provides their provisional diagnosis of the situation.
I believe the patient has a symptomatic air embolus.
Recommendation —The speaker suggests a course of action.
Can you begin irrigating the field, and can I place the patient in the Trendelenberg position ?
Regardless of the exact method utilized, there are some generalities for communication that should always be enacted. First, communication should be directed—the name of the person being spoken to should be used, capturing their attention. Second, communication should be concise. Lastly, communication should be closed-loop—that is, the listener should acknowledge the speaker and confirm they understood their message.
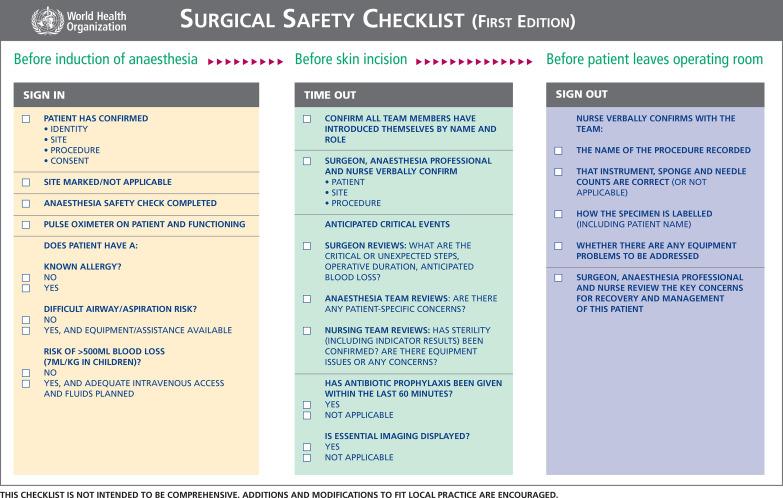
CRM promotes the use of checklists to organize and align teams before critical events. Checklists, like the WHO surgical safety checklist ( Fig. 10.1 ), are used routinely in neurosurgery. The WHO checklist is divided into three phases of care: (1) before anesthesia induction, (2) before skin incision, and (3) before the patient leaves the OR. Each section has only a few items, but all help unify the surgical team and prevent adverse events. When reviewing the application of the WHO checklist to tens of thousands of surgical patients, a ~ 40% reduction in postoperative complications was observed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here