Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The spine and the peripheral nervous system remain diagnostically challenging to image owing to the extensive bony canal, relatively small size of the neural elements, and multiplicity of clinical symptoms.
A wide variety of techniques are available for imaging the spine. MRI is the procedure of choice for evaluation of many of the musculoskeletal and neurologic diseases of the spine. The musculoskeletal system includes the vertebral bodies, intervertebral discs, intervertebral foramina, ligaments, and facet joints. The portions of the nervous system evaluated include the spinal cord, spinal roots, and caudal portion of the brain stem and cerebellum. Conventional radiographs, bone radionuclide scans, positron emission tomography (PET), CT, CT myelography, and CT angiography are additional modalities that provide complementary information with indications depending on the disease entity being evaluated—degenerative disease, infection, tumor, and trauma—all of these modalities are instrumental when evaluating the spine in a surgical patient.
Radiographic correlation of symptoms in patients with back pain is a difficult task. A number of findings are not significantly more frequent in patients with back pain compared with controls. Incidental findings may include transitional vertebrae, spina bifida occulta, asymmetric facet joint orientation, facet joint osteophytes, Schmorl's nodes, and increased lordosis.
Demonstrating inflammatory changes and the relationship of pain to disc protrusions on MRI is controversial. No correlation has been demonstrated between the size, side, or level of herniation and the degree of disability, pain, or frequency of neurologic symptoms, even in patients with concomitant central or foraminal stenosis.
The use of a contrast agent has not clarified the relationship between disc herniation, inflammation, and symptoms. Nerve root enhancement may be seen in symptomatic and asymptomatic patients with and without disc herniations. In one study of asymptomatic volunteers, 63% demonstrated nerve root enhancement that was found likely to be related to caudally draining veins accompanying the nerve root.
A high prevalence of disc bulges and protrusions has been demonstrated on lumbar spine MRI in asymptomatic patients. In addition, Schmorl's nodes, annular defects, and facet arthropathy were also found to be present in patients without back pain. These findings therefore may frequently be coincidental, and a patient's clinical situation must be evaluated in conjunction with the findings on MRI.
Development of functional spine imaging may greatly facilitate the evaluation of spondylostenosis, radiculopathy, and myelopathy and aid the surgeon in the diagnosis and treatment of the patient with spine pain.
Central canal stenosis is characterized by distortion or compression of the thecal sac or obliteration of the adjacent epidural fat. This is predominantly due to impingement by osteophytes, facet joints, thickening of the ligaments, and bulging of the intervertebral discs. Although the size of the central canal has a wide range of normal values and MRI can overestimate the degree of stenosis, specific quantitative data have been published.
Within the cervical spine, the most accurate assessment of spinal canal size can be obtained from sagittal T2-weighted (T2W) fast spin-echo sequences. CT has been considered the study of choice for assessing cervical foraminal stenosis because the margins of the normal foramen, central canal, and osteophytes are so well demonstrated. On MRI, gradient-echo sequences can be used, although there is some degree of motion and magnetic susceptibility artifact. In the cervical spine, the normal diameter of the canal is greater than 13 mm in the sagittal plane. A sagittal measurement of 10 to 13 mm is considered borderline spinal stenosis.
Central stenosis in the lumbar spine has been characterized numerically as an area less than 1.5 cm 2 or an anteroposterior diameter of less than 11.5 mm. In clinical practice, the degree of stenosis is usually described qualitatively as mild, moderate, or severe rather than quantitatively. The thecal sac is distorted from a typically round morphology to a horizontally flattened, oblong shape. In severe cases, a trilobed configuration may result.
A limitation in evaluation of spinal stenosis is due to the fact that patients are routinely imaged in the supine position. Routine spine imaging in the static-recumbent position precludes evaluation of the effects of gravity and associated increased mass effect on the spine and discs. Patients experience signs and symptoms during dynamic-kinetic maneuvers. This is not possible to assess with standard conventional imaging of the spine with the patient in static recumbency.
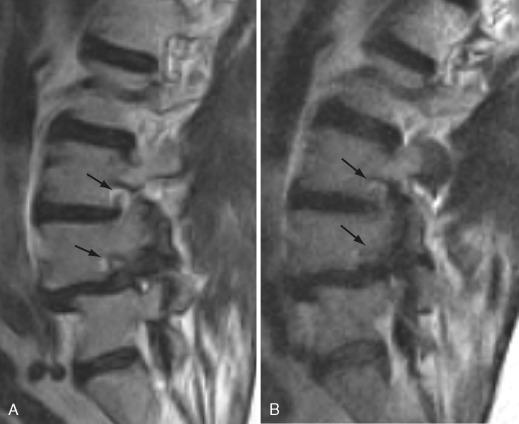
Open MRI scanners with upright and recumbent imaging capabilities facilitate partial or full weight bearing and simultaneous kinetic maneuvers that can reveal radiologically occult but clinically relevant weight bearing–dependent disease not visible on a static-recumbent examination and unmasked by positional imaging technique with relative potential decreased sensitivity in demonstrating relevant pathology of central and lateral stenoses ( Figs. 22-1 and 22-2 ).

Because upright MRI scanners are not widely available, axial loading devices may be another approach for functional imaging of the spine patient. Axial loading devices apply forces that are a percentage of a patient's weight on the patient's spine. This is done with a harness compression device that the patient wears. The increased axial load simulates the patient in an upright position and may reveal central and lateral stenoses not evident on conventional supine spine imaging.
Cervical spondylotic myelopathy is the most common cause of spinal cord dysfunction in older individuals. Controversy remains in terms of the optimal timing and indications for surgical intervention. It would be of benefit to define clinical and MRI predictors of outcome. A crucial question regarding when to perform spinal decompression relies on the evaluation for myelopathy. When clinical examination and electrodiagnostic studies are equivocal and there is radiographic evidence of significant stenosis, an important question is whether surgical decompression should be performed to prevent irreversible damage to the spinal cord. Conventional radiographic MRI evaluation of spinal cord compromise due to spondylotic changes may be insensitive and relatively delayed. When increased T2 signal is evident within the spinal cord, the patient's symptoms may be irreversible. Intramedullary spinal cord changes in signal intensity in patients with cervical spondylotic myelopathy can be reversible (hyperintensity on T2W imaging) or nonreversible (hypointensity on T1-weighted [T1W] imaging). The regression of areas of hyperintensity on T2W imaging is associated with a better prognosis, whereas the T1W hypointensity is an expression of irreversible damage and, therefore, the worst prognosis. Patients with high intramedullary signal change on T2W imaging who do not have clonus or spasticity may experience a good surgical outcome and may have reversal of the MRI abnormality. A less favorable surgical outcome is predicted by the presence of low intramedullary signal on T1W imaging, clonus, or spasticity. These data suggest that there may be a window of opportunity to obtain optimal surgical outcomes in patients with cervical spondylotic myelopathy.
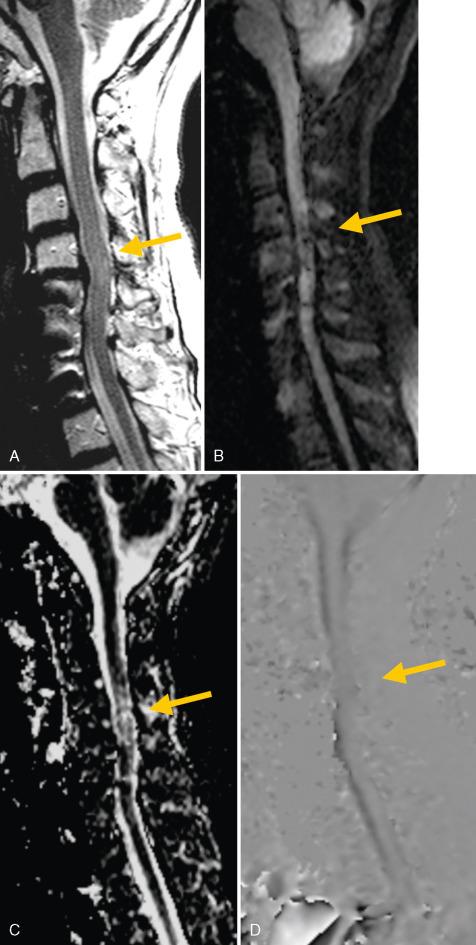
Diffusion-weighted imaging (DWI) is more sensitive and has a higher negative predictive value than T2W imaging for the early detection of cervical spondylotic myelopathy. Because the results of surgical treatment are better in mildly affected patients than in severely affected patients, the diagnosis of cervical spondylotic myelopathy must be made as early as possible and with highly sensitive tools.
DWI has been extremely helpful in evaluating lesions in the brain such as acute infarction, abscess, and neoplasm. The image contrast it provides is dependent on detecting random microscopic molecular water motion, which can be significantly altered in various disease states. Its use in spine imaging is being developed for evaluation of the spinal cord and potential causes of myelopathy.
The lesion formation in the spinal cord is not precisely understood. Increase in pressure from cord compression may induce chronic hypoperfusion, with ischemic or hypoxic injury leading to subsequent vacuolization of gray and white matter. DWI of the spinal cord may be more sensitive than conventional T2W imaging for evaluation of patients with cervical myelopathy and demonstrating spinal cord changes compatible with an increase in water diffusion and changes in diffusion direction. The underlying pathologic process may represent water increase in myelomalacia, chronic ischemia, inflammation, and cavitation. Changes may be located primarily in the interstitial space where molecules may flow from the subarachnoid space into the central spinal cord or destruction of cell membranes may result in increased water diffusion. Demyelination may also result in increased water diffusion.
Given the high sensitivity and high negative predictive value of DWI, this technique may facilitate decision making and make adequate treatment possible, especially for patients in whom clinical examination reveals discrete symptoms.
Various hydrodynamic changes occur in cerebrospinal fluid (CSF) flow in cervical spinal stenosis. Dynamics of CSF flow are altered in areas of canal stenosis. Spinal stenosis does not alter the cord or CSF velocities at the C2 level but increases the velocity of CSF in the anterior CSF space below the stenotic segment when the stenosis is assessed by cord and dural sac area measurements. When the stenosis is assessed by relating the cord area to the dural sac area, a statistical correlation between narrow spinal canal and high velocities in the anterior CSF space below the stenotic segment is found. Phase-contrast CSF flow imaging and the sensitivity to demonstrate abnormal CSF dynamics in patients with stenoses may therefore be a helpful imaging tool in evaluating patients with stenosis and equivocal clinical examination findings of myelopathy ( Fig. 22-3 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here