Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thoracic injury is a common sequela of acute trauma and is the third most common injury in trauma patients, after head and extremity injuries. The overall mortality rate approaches 25%, with acute aortic, tracheobronchial, and cardiac injuries often having an even worse prognosis. Given the high mortality rate and the impact on clinical management, rapid and accurate assessment of thoracic trauma imaging is imperative.
There are conflicting data in the literature on whether routine chest CT should be performed in all cases of thoracic trauma. Chest CT is much more accurate than chest radiography in evaluating thoracic trauma, with at least 50% of pneumothoraces, rib fractures, and pulmonary contusions missed on routine anteroposterior chest radiographs. Some studies have shown that CT changes management in a significant proportion of patients, and potentially fatal injuries such as aortic laceration could be missed. Other studies have shown that with appropriate clinical assessment and use of other radiographic and demographic data, patients can be selected for whom chest CT would be more likely to identify injuries, thus saving cost and radiation. The American College of Radiology Appropriateness Criteria for blunt thoracic trauma in 2014 have suggested that CT should be strongly considered in patients with “high-mechanism injury, abnormal chest radiographs, altered mental status, distracting injuries, or clinically suspected thoracic injuries. CT angiogra[phy] should be routinely used in patients with suspected acute aortic laceration.”
Unless contraindicated due to allergy or renal failure, contrast should be used in all CT scans of thoracic trauma. This allows for much more accurate assessment of vascular injury, which is a significant cause of morbidity and mortality in thoracic trauma. In most cases, precontrast images are not necessary. It is also important to choose a reconstruction algorithm with some degree of overlap. This allows for high-quality multiplanar reconstructions, which can be very helpful in the detection of certain types of thoracic injury.
In the setting of trauma, gas and fluid can accumulate in different thoracic spaces, with different causes and clinical significance. It is important to be aware of each of these to direct the appropriate management of the trauma patient.
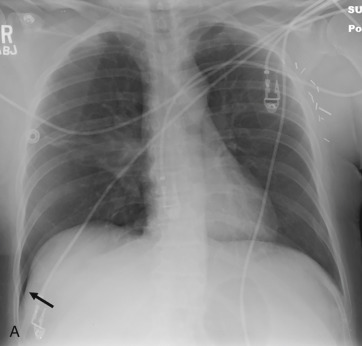
Pneumothorax or air within the pleural space occurs in up to 20% to 40% of blunt trauma patients presenting to the emergency department. Up to 50% of pneumothoraces may be missed with portable radiography ( Fig. 43.1A ). These are termed occult pneumothoraces and are rarely symptomatic. However, in the setting of positive end-expiratory pressure mechanical ventilation, they can significantly enlarge, and therefore are often drained with a chest tube.
On a chest radiograph, one should be careful not to mistake a skin fold for a pneumothorax. The pleural line in a pneumothorax is seen as a thin white line, with no lung markings beyond it, whereas a skin fold is often less dense, has lung markings beyond it, and can be seen projecting into the soft tissues. Mach bands, which are due to an optical illusion resulting in incorrect perception of density at the borders, of varying shades of gray, can also simulate pneumothorax on chest radiograph. On chest CT, use of a sharp kernel such as with a bone algorithm can result in an artifact mimicking pneumothorax.
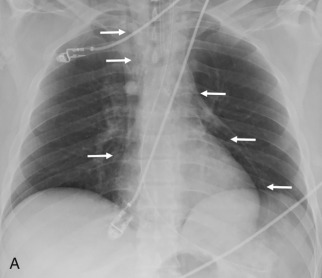
One of the most important findings to assess is whether there are signs of tension physiology because this can be lethal to the patient. Signs of tension in the pleural space from pneumothorax or hemothorax include contralateral mediastinal shift, flattening or inversion of the ipsilateral hemidiaphragm, and a hyperexpanded ipsilateral chest (see Fig. 43.1B and C ). If these signs are seen, emergent decompression is warranted because cardiovascular collapse can occur.
Rib fractures are commonly associated with pneumothorax, and careful attention should be given to the ribs when a pneumothorax is seen in the setting of trauma. Multiple contiguous segmental rib fractures are termed flail chest, which has a high (≈50%) association with injuries requiring surgical treatment and prolonged mechanical ventilation.
Most cases of pneumomediastinum in blunt thoracic trauma are due to the Macklin effect, which is alveolar rupture resulting in gas dissecting along the bronchovascular sheath into the mediastinum ( Fig. 43.2 ). This is typically due either to barotrauma or increased pressure against a closed glottis.
In the setting of trauma, one should always carefully assess the esophagus and tracheobronchial tree because direct injury to these structures can result in pneumomediastinum.
Pneumopericardium, or air within the pericardial space, implies a defect in the pericardium and is unusual after blunt thoracic trauma. Pneumopericardium in the setting of penetrating trauma, however, can be enough to warrant surgical exploration to assess for cardiac injury. When encountered, one should carefully assess for any pericardial defect and look for signs of cardiac injury. CT cannot exclude cardiac injury because the right ventricular free wall, the most anterior portion of the heart, is only 2 to 3 mm thick, and lacerations are often not seen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here