Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
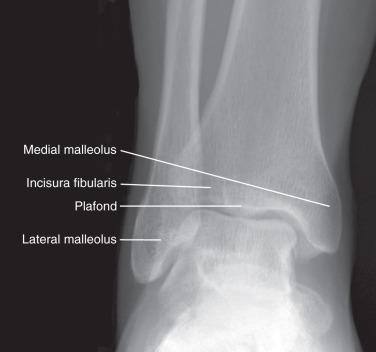
Radiographs are often the initial imaging study performed for any patient presenting with a problem related to the foot and ankle. Radiographs are clearly beneficial when evaluating for suspected arthritis, osteonecrosis, tumors, nonunion, or trauma. In addition, the alignment of the ankle and foot may contribute to the presenting complaint even if the radiographs being viewed are free of pathologic abnormalities. To appropriately evaluate the osseous structures and alignment of the foot, the radiographs should be obtained with weight bearing in all cases, except when a fracture may be suspected ( Figs. 112.1–112.3 ). Specifically, in the setting of a suspected Lisfranc injury, if the initial non–weight-bearing radiographs are negative, follow-up weight-bearing films should be ordered to evaluate for diastasis of the tarsometatarsal joints.


The most current generation of multidetector computed tomography (CT) scanners are capable of providing high-resolution images in all imaging planes and are superb for evaluating the extent and location of intra-articular fractures in the area of the ankle and hindfoot. Given the difficulty in assessing joint congruity in the hindfoot, follow-up CT imaging is recommended in this setting to better appreciate the fracture pattern and joint congruity. Cystic osteochondral defects of the talus are excellently visualized with this modality to accurately calculate the size of the lesion and guide preoperative planning. It is also an excellent method of assessing bony healing, including evaluation of fractures and arthrodeses. Sufficient data are available to suggest that determination of the percentage of bony trabeculation across an arthrodesis site in the ankle and hindfoot is grossly underestimated with plain radiography. The administration of intra-articular contrast material followed by CT imaging through the ankle (CT arthrography) is an accurate means of assessing internal derangement in patients who have a contraindication to magnetic resonance imaging (MRI). CT technology has now evolved into obtaining weight bearing scans of the lower extremity which can provide the surgeon with functional information regarding joint biomechanics. This technology can be extremely useful in situations where radiographs are not able to provide information due to overlap of bones. For example, in patients with midfoot arthrosis, weight-bearing CT is able to isolate each joint in the midfoot and assess for bone-on-bone apposition during weight bearing. It also provides accuracy and ease of assessing syndesmotic alignment as well as degree of subfibular impingement in hindfoot valgus deformity.
The primary advantage of ultrasound compared with MRI is the ability to evaluate the tendinous structures in a dynamic fashion. Ultrasound is the imaging modality of choice for the evaluation of peroneal tendon subluxation. The evaluation for tendon apposition in the setting of an Achilles tendon rupture or for evaluation of flexor hallucis longus (FHL) stenosing tenosynovitis are examples of when the ability to perform a dynamic examination is critical. Advantages include a relative cost saving compared with MRI and improved localization of soft tissue structures for injection. A limitation of ultrasound is that visualization of the affected structure may prove more difficult in patients with a high amount of subcutaneous fat. Additionally, the clinician is reliant upon the interpretation of the radiologist and the skill of the ultrasonographer for the determination of the pathologic findings. Good communication between the clinician and the radiologist is critical to ensure that the radiologist has an understanding of the exact clinical concern so the examination can be tailored appropriately.
MRI is well accepted as the primary noninvasive imaging modality for providing a global assessment of the foot and ankle and is very accurate for the evaluation of cartilaginous, tendon, ligament, and bony abnormalities. MR arthrography of the ankle can be used to obtain a more precise evaluation of articular cartilage injuries to the talar dome or tibial plafond. T1-weighted fat-saturated images are key to evaluate the gadolinium contrast material in the joint. These images show the contrast to the greatest advantage. Because evaluation of bone marrow is also critical, T1-weighted non–fat-saturated images are also essential. T1-weighted images in general are superior to evaluate the anatomy, bone marrow, hemorrhage, masses, fat, and fatty infiltration of muscles. Proton density or intermediate images are high resolution and therefore important in the evaluation of ligaments, tendons, and small structures such as cartilage. T2-weighted images are the best sequence to evaluate for fluid, edema, joint effusions, muscle, and soft tissue injuries. Fluid sensitivity is increased with use of fat saturation.
Dedicated foot and ankle coils or smokestack coils are critical in obtaining high-quality imaging of foot and ankle disorders. Images are performed in the sagittal, axial, and coronal imaging planes. When ordering an MRI, the specific area of concern should be communicated to the radiologist. Given that the smallest field of view optimizes image quality, an MRI scan that captures the entire foot and ankle will compromise the quality of the foot images. Additionally, specific protocols may exist for the forefoot versus the hindfoot, and therefore the specific site of the pathologic condition should be stated to ensure that the appropriate MRI protocol is used.
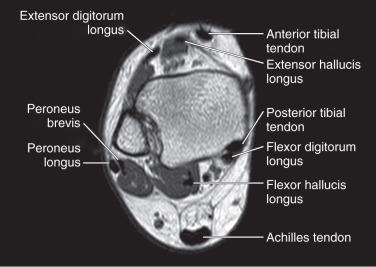
Given a tendon's lack of fluid, a normal tendon has low signal intensity on all imaging sequences ( Fig. 112.4 ). Axial cuts are the most useful to determine the presence and extent of tenosynovitis and tendinosis. Coronal imaging, although complementary, provides the least information. An area of focal thickening is not a normal finding.
Disorders of the Achilles tendon are diagnosed with relative ease as a result of the subcutaneous nature of the tendon. The presence of tendinosis is noted by focal thickening of the tendon that moves in conjunction with the tendon, as opposed to paratenonitis. The primary utility of MRI is to determine the precise location and affected volume of the tendon for preoperative planning. Increasingly, with nonoperative management of Achilles tendon ruptures demonstrating good results with functional rehabilitation, MRI is very useful to determine if adequate apposition is obtained with plantar flexion of the ankle after the cast has been placed as an alternative to ultrasonography.
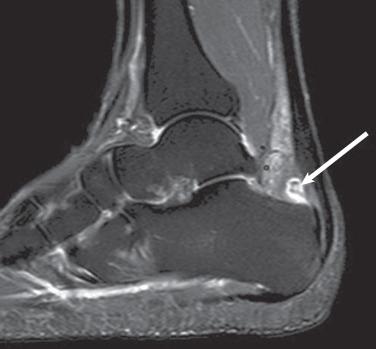
The primary evaluation of the Achilles tendon is performed with use of a combination of T1- and T2-weighted axial and sagittal images. The tendon has a near uniform thickness and flattens out distally as it inserts into the calcaneus. The tendon should be taut and parallel when comparing the anterior and posterior margins of the tendon ( Fig. 112.5 ). A flat or concave anterior margin is normal. The normal anteroposterior diameter on axial or sagittal imaging is 7 mm.

Intermediate or high signal intensity on either a T1- or T2-weighted image with continuity of the tendon is indicative of Achilles tendinopathy. Fusiform thickening of the tendon noted on T1-weighted sagittal imaging is diagnostic of Achilles tendinosis ( Fig. 112.6 ). High signal intensity on a T2-weighted image that is as bright as fluid is suggestive of a more acute process and is sometimes referred to as a “partial tear.” Calcification of the Achilles insertion is easily visualized on T1-weighted sagittal images and is diagnostic of insertional Achilles tendinopathy. A teardrop fluid signal (high intensity) anterior to the Achilles tendon at the level of the calcaneus is suggestive of retrocalcaneal bursitis ( Fig. 112.7 ). Fluid signal (high intensity) posterior to the Achilles tendon itself is suggestive of retro Achilles bursitis. A fluid signal defect (high intensity) within the Achilles tendon on both T1- and T2-weighted fat-saturated images is indicative of an acute rupture ( Fig. 112.8 ).

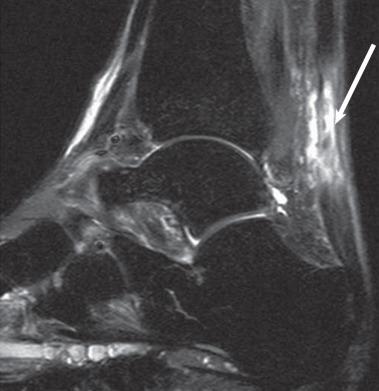
High signal intensity on T1- or T2-weighted fat-saturated imaging of the Kager fat pad is suggestive of paratenonitis. A wavy or retracted appearance of the tendon on T1- or T2-weighted fat-saturated imaging is highly suggestive of an Achilles rupture.
A small amount of increased signal intensity near the insertion of the Achilles tendon represents interposed fat and is normal; it should not be confused with insertional tendinosis. The plantaris tendon can be intact in the presence of an Achilles rupture and should not be confused with a partial tear or intact Achilles tendon.
Routine use of advanced imaging to determine of the presence of posterior tibial tendon disease is not required. Given the associated flatfoot deformity and subcutaneous position of the tendon, physical examination plays the major role in the diagnosis. However, in cases of suspected tenosynovitis or posttraumatic or sudden-onset flatfoot, and in patients in whom possible debridement and retention of the tendon is being considered, MRI is an excellent adjunct. Isolated debridement and retention of the tendon is typically considered only in the setting of tenosynovitis without intrinsic disease. In the setting of tendinosis, retention of the posterior tibial tendon with an associated tendon transfer will improve the postoperative inversion strength but carries the risk of persistent pain and should be performed with caution.
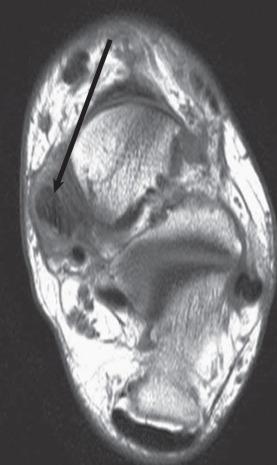
Axial cuts are the most useful in evaluating the posterior tibial tendon. Ideally the patient should be positioned prone with the foot plantar flexed to place the tendons in a more linear position and reduce the “magic angle” effect. The posterior tibial tendon should be of uniform thickness throughout its length ( Fig. 112.9 ).
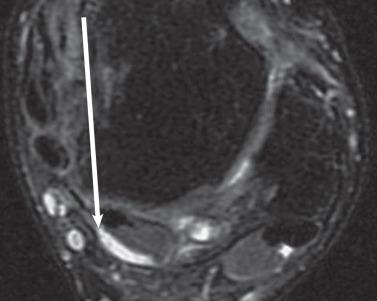
The presence of fluid (high signal intensity) adjacent to the posterior tibial tendon on T2-weighted imaging is sensitive for tenosynovitis ( Fig. 112.10 ). This finding is not specific and is seen in 22% of asymptomatic persons. A focal area of increased signal on T2-weighted images, known as a punctate signal , corresponds to a small intrasubstance tear. A focal area of increased signal intensity within the substance of the tendon that extends to the tendon surface on T1-weighted imaging and corresponding high signal intensity on T2-weighted imaging is consistent with a tear. Complete absence of the posterior tibial tendon or replacement of the normal tendon location with high signal intensity on T2-weighted imaging indicates a rupture. Replacement or infiltration of the normally low signal intensity of the tendon with intermediate (gray) signal is consistent with tendinosis ( Fig. 112.11 ). A small tendon caliber (smaller diameter than the flexor digitorum longus) is consistent with atrophic tendinosis and can be seen on any axial imaging sequence.
Periretinacular soft tissue edema and thickening of the flexor retinaculum on any imaging sequence is suggestive of disease. Soft tissue edema adjacent to the flexor retinaculum can be seen on T2-weighted imaging. High signal intensity within the medial malleolus without a prior history of trauma may also be seen. High signal intensity noted on T2-weighted imaging within the accessory navicular can be present.
A small amount of fluid within the tendon sheath can be normal; correlation with intrasubstance increased signal intensity is more specific for tendon disease.
FHL tendinopathy has classically been described as a disorder in female ballet dancers, in whom constant ankle hyper plantar flexion can cause FHL irritation at its entrance to the flexor retinaculum. Recently it has been noted to affect other patients with chronic foot or ankle pain who often initially were diagnosed with other foot or ankle pathologic conditions. Ultrasound can be effective in determining the presence of dynamic entrapment of the FHL within the fibro-osseous tunnel. MRI is also particularly useful to evaluate for synovitis, the extent of tendon degeneration, and edema within the os trigonum, which can be associated with this condition.
Sagittal cuts are a useful adjunct when evaluating the FHL as it passes under the sustentaculum tali to the forefoot. Ideally the patient should be positioned prone with the foot plantar flexed to place the tendons in a more linear position and reduce the “magic angle” effect. The tendon has a very low-lying muscle belly that is normally present at the level of the ankle.
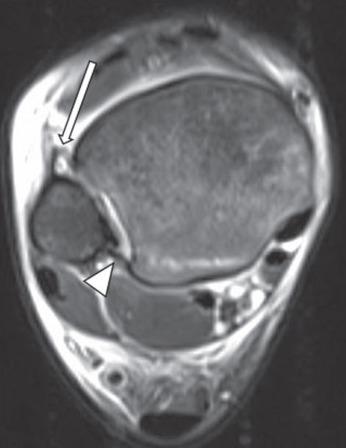
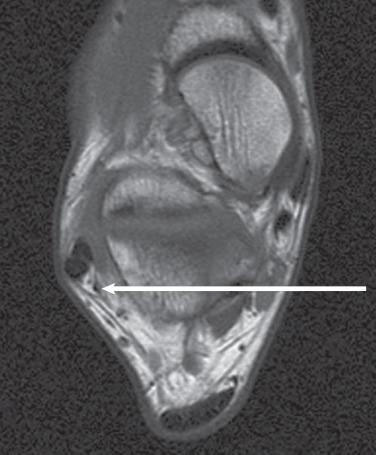
MRI findings of tendinosis as outlined previously, with increased signal intensity within the tendon or tears of the tendon, are rarely seen in the FHL. The presence of fluid (high signal intensity) on T2-weighted imaging is diagnostic of FHL tenosynovitis. The most common location is posterior to the talus within the fibro-osseous tunnel ( Fig. 112.12 ). However, it can also occur in the midfoot at the knot of Henry or distally at the level of the first metatarsophalangeal joint as it passes between the sesamoids. Careful inspection of the entire length of the FHL should be performed from the ankle to the insertion into the distal phalanx because compression can occur in the ankle, midfoot, and forefoot. The presence of fluid proximal and distal to the tendon at the level of the fibro-osseous tunnel posteriorly is diagnostic of stenosing tenosynovitis. The severe compression limits the fluid from entering the tunnel.
High signal intensity within the os trigonum on T2-weighted imaging should prompt close inspection of the FHL because both FHL synovitis and os trigonum syndrome can occur simultaneously.
Failure to inspect the entire length of the tendon can lead one to miss the less common but symptomatic compression of the FHL within the knot of Henry and sesamoid complex.
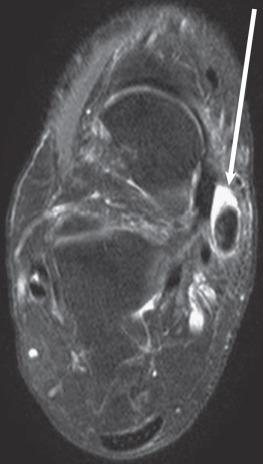
Intrinsic disorders of the peroneal tendons include tenosynovitis, tendinosis, tendon tears, and painful os peroneum syndrome. Additionally, symptomatic subluxation or intrasheath subluxation may be present, producing pain in addition to instability. Chronic subluxation of the tendons increases the risk of developing degenerative tears of the tendons as a result of the mechanical trauma from the posterolateral fibrocartilaginous ridge of the fibula. Ultrasound can be a very effective tool for examination of the peroneal tendons, specifically in the setting of intrasheath subluxation, where subjective “snapping” may be the only appreciable finding. MRI is very useful when considering operative intervention to determine the presence of synovitis, tendinosis, tears, a low-lying muscle belly of the brevis, and a peroneus quartus, in addition to visualizing the concavity of the fibular groove.
The primary evaluation of the peroneal tendons is performed using a combination of T1- and T2-weighted axial images. The peroneus quartus is a normal muscle variant encountered in 13% to 26% of patients. It will appear as a third tendon within the peroneal tendon sheath ( Fig. 112.13 ). The common insertion is the calcaneus, although multiple variants have been noted. A flat or convex fibular groove is associated with peroneal tendon disorders, but a flat groove is seen in more than two thirds of normal persons.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here