Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Plain radiographs offer an indirect evaluation of the rotator cuff and soft tissue of the shoulder joint, and this imaging modality is an important tool in the diagnosis of shoulder pathology. There are multiple imaging findings that can provide indirect information on the status of the rotator cuff and shoulder joint. This is a good first-line evaluation for shoulder pathology.
It is our preference to obtain initial radiographs on all patients with concern for rotator cuff pathology due to the ease with which these images are acquired, the relative low cost of this modality, and the ability to evaluate for other conditions, such as arthritis or evidence of previous trauma or surgical interventions.
A complete radiographic evaluation of the shoulder, when concerned about potential rotator cuff pathology, includes anteroposterior (AP), Grashey, supraspinatus outlet, and axillary lateral views ( Fig. 6.1 ). We will also add an AP active-abduction view when we have suspicion of large rotator cuff tears or concerns with advanced shoulder osteoarthritis.

The Grashey view is a true AP of the glenohumeral joint and is obtained with the patient rotated posteriorly 35–45 degrees so that the plane of the scapula is parallel to the imaging cassette.
The axillary lateral image provides an orthogonal image to evaluate the condition of the glenoid, humeral head, and acromion.
The supraspinatus outlet view shows acromion morphology, which is classified according to Bigliani.
The AP active-abduction image is obtained with the patient holding a 1–2 lb weight in 45 degrees of abduction to better evaluate for humeral head migration and joint space narrowing. Patients with anterior-superior escape or dynamic instability will show very clear superior migration of the humeral head on this view ( Fig. 6.2 ).

The acromiohumeral interval (AHI) can be measured ( Fig. 6.3 ). An AHI less than 7 mm is associated with rotator cuff pathology. In one cohort of patients, for patients with an AHI less than 7 mm, 90% had a supraspinatus tear, 67% had an infraspinatus tear, and 43% had subscapularis tears.

An increased critical shoulder angle, defined as a combined measurement between the glenoid inclination and lateral extension of the acromion, has been associated with rotator cuff pathology ( Fig. 6.4 ). Conversely, a decreased critical shoulder angle was associated with primary glenohumeral osteoarthritis. A group of asymptomatic patients had a critical shoulder angle of 33.1 degrees, while for those with rotator cuff tears it was 38.0 degrees and for those with glenohumeral arthritis it was 28.1 degrees.

The acromion shape may have an association with presence of a rotator cuff tear. In one retrospective analysis, 88.9% of patients with a type 3 acromion had an associated rotator cuff tear.
Patients with calcific tendonitis, which is visible on radiographs, may present with symptoms similar to impingement syndrome or rotator cuff pathology ( Fig. 6.5 ).

Chronic bony changes may be apparent in the setting of a chronic massive rotator cuff tear. The humeral head begins to undergo changes described as femoralization. The acromion also shows evidence of remodeling, known as acetabularization ( Fig. 6.3 ).
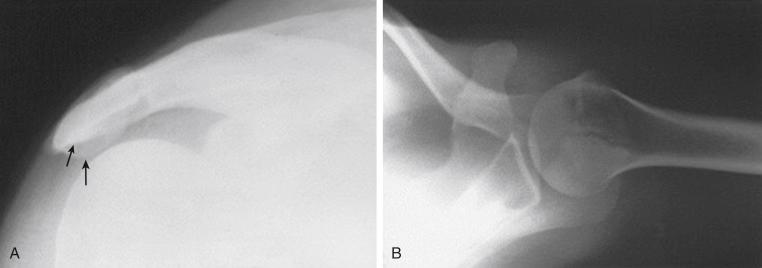
An os acromiale ( Fig. 6.6 ), which is a failure of fusion of one of the ossification centers of the acromion, is best seen on an axillary lateral radiograph. This finding has been associated with rotator cuff pathology.
In the setting of an acute traumatic injury, a radiographic evaluation will diagnose a proximal humerus fracture. An isolated greater tuberosity fracture may appear similar clinically to a patient with an acute rotator cuff injury ( Fig. 6.6 ).
Plain radiographs are relatively inexpensive and usually easy to obtain.
As part of an initial evaluation, radiographs can help exclude certain conditions that may present with symptoms that overlap with rotator cuff injuries, such as early osteoarthritis and calcific tendonitis.
Radiographs offer no soft tissue evaluation, so the information regarding the rotator cuff is limited with this imaging modality.
Most signs associated with rotator cuff pathology are present only in the chronic setting.
The evolution of musculoskeletal ultrasound over the past two decades has allowed for its successful use in thoroughly evaluating the rotator cuff. Ultrasound is very effective in evaluating the dynamic stabilizers of the shoulder, including the rotator cuff musculature, the biceps tendon, the deltoid, and the pectoralis muscles. Unique among other imaging techniques, ultrasound allows for both a static and dynamic evaluation of the shoulder anatomy, potentially providing for a better understanding of the function of the surrounding structures and musculature. Ultrasound is even useful for identifying secondary signs of rotator cuff pathology, such as greater tuberosity cortical roughening, and evaluating the integrity of rotator cuff repair after surgery. Lastly, ultrasound can be used to assist with nonoperative interventions for rotator cuff pathology or impingement. Such interventions include image-guided corticosteroid injections and needling procedures for rotator cuff calcifications.
Sound waves of a certain frequency are generated from an ultrasound transducer and reflected back from the underlying structures to the ultrasound transducer to generate an image.
Musculoskeletal ultrasound wave frequency averages 5–12 MHz (range 4–17 MHz).
High-frequency sonographic waves are attenuated more quickly as they pass through tissue, meaning that higher-frequency ultrasound transducers have less imaging depth but the benefit of higher resolution capabilities.
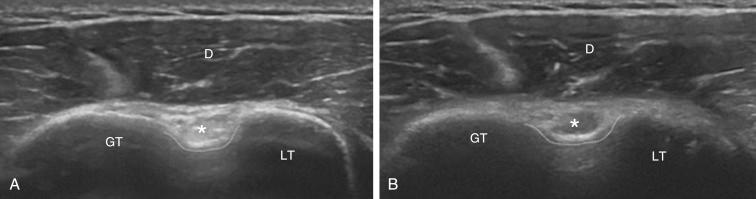
Sound waves best create an image when they are oriented perpendicular to the collagen fibrils that make up the particular tissue or tendon being evaluated. This perpendicular orientation produces the characteristic bright reflective echo that is seen on ultrasound images. Deviation from the perpendicular results in an area of decreased echogenicity, possibly giving the false impression of tendon pathology. This concept is termed anisotropy .
An example of anisotropy is seen in evaluating the biceps tendon in Fig. 6.7 .
The following parameters can be adjusted for better image quality:
Depth of field of view
Depth of focus
Gain and time gain compensation (i.e., change in amplitude)
Frequency of the probe
Convention for recording and viewing ultrasound images:
The left side of the screen represents posterior and superior
The right side of the screen represents anterior and inferior
Always obtain orthogonal views of the structure of interest
Label findings both in the long and short axes
Standard examination of the shoulder with ultrasound includes a systematic evaluation of the joint ( Table 6.1 ).
The rotator cuff is usually examined starting with the long head of the biceps anteriorly and working from anterior to posterior, completing the exam with evaluation of teres minor.
Each tendon should be evaluated in a short axis and long axis (i.e., orthogonal views).
| Sequential Protocol to Perform Dynamic Ultrasound Evaluation of the Shoulder | |||
|---|---|---|---|
| Step | Structures | Standard Scans | Dynamic Maneuver |
| 1 | Long head biceps tendon; pectoralis major tendon | Anterior transverse and longitudinal scan in neutral position | Active and/or passive external rotation of the humerus with 90-degree flexed elbow |
| 2 | Subscapularis tendon: long head biceps tendon subluxation-dislocation | Anterior transverse and longitudinal scan in maximal external rotation of the humerus | Active and/or passive external rotation of the humerus with 90-degree flexed elbow |
| 3 | Supraspinatus tendon: subacrominal-subdeltoid bursa; rotator interval; rotator cable crescent complex | Anterior transverse and longitudinal scan in Crass/Crass-modified position | Crass/crass-modified position with medical stress on the flexed elbow |
| 4 | Acromioclavicular joint: coracoacromial ligament; impingement evaluation | Superior/anterosuperior longitudinal scan in neutral position. | Abduction of the arm with 90-degree flexed elbow |
| 5 | Infraspinatus tendon: teres minor tendon: posterior glenoid labrum, suprascapular nerve | Posterior transverse and longitudinal scan with raised arm | External rotation of the arm with the elbow adherent to the chest |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here