Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In contrast with the right common iliac vein, which ascends almost vertically to the inferior vena cava (IVC), the left common iliac vein takes a more transverse course beneath the right common iliac artery, which may compress it against the lumbar spine before entering the vena cava. This compression causes stasis of the blood, which is one element of Virchow's triad that may precipitate deep venous thrombosis (DVT).
In approximately 40% of patients, the precursor to iliac vein obstruction is not thrombosis, but rather, a nonthrombotic iliac vein lesion (NIVL). Also known as May-Thurner syndrome or iliac vein compression syndrome, it is caused by web formation and obstruction. A nonthrombotic blockage is defined as an absent clinical history of DVT coupled with absent findings on imaging studies, such as contrast venography and ultrasound. This lesion is classically found in the left common iliac vein of younger females; but, it is not uncommon in males or in elderly patients, and may involve the right limb. At least 15% of the limbs with primary disease have been shown to have stenosis of both common and external iliac veins.
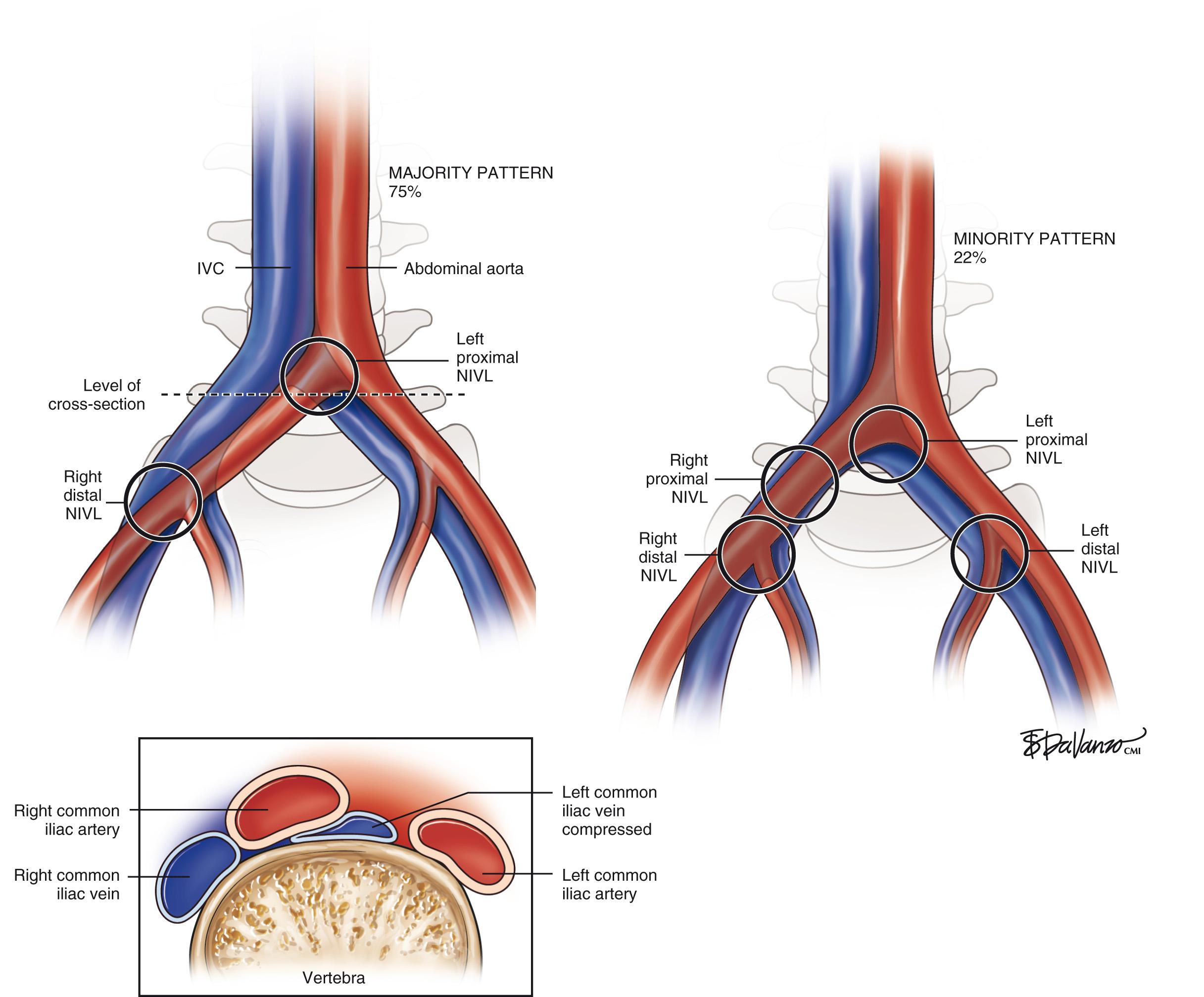
As depicted in Fig. 18.1 , the right common iliac artery always crosses the left common iliac vein at the confluence of the IVC and is where classic proximal left NIVL occurs. In 75% (majority pattern), the right iliac artery continues its course to cross near the external iliac vein level, in which case, it may induce right distal NIVL. In the minority pattern (22%), the right, common iliac artery crosses the right, common iliac vein, and then down over a longer length of the external iliac vein and can thus induce either a proximal or distal right NIVL. The left distal lesion may be related to the crossing of the vein by the left hypogastric artery. These anatomic variations may explain why proximal NIVLs occur much more frequently on the left side than on the right side, why the left lesion is focal and the right less so, and why the distal NIVL occurs equally on either side.
Although traditional venous corrective surgery concentrated on the correction of superficial and deep venous reflux below the inguinal ligament, the introduction of minimally invasive venous stenting using venography and intravascular ultrasonography (IVUS) provides the ability to treat the “obstructive” component of the disease above the inguinal ligament. The emphasis on IVUS as the key diagnostic tool was promulgated by Raju and Neglén who have shown that iliac venous stenting alone is sufficient to control symptoms in most patients with combined outflow obstruction and deep reflux.
The iliac vein is the common outflow tract of the lower extremity, and chronic obstruction of this segment can result in severe symptoms. The most frequent precursor to chronic pelvic venous outflow obstruction is iliofemoral DVT. Only 20% to 30% of iliac veins completely recanalize spontaneously after thrombosis, whereas the remaining veins recanalize partially and develop varying degrees of collaterals. This may result in significant residual obstruction to the venous outflow of the lower extremity. In the iliofemoral segment, collateral vein formation is relatively poor, and thus results in more severe symptoms than lower segmental blockage. Distal obstructions are more readily compensated for because of robust femoral-popliteal collaterals, profunda-popliteal vein connections, deep muscular tributaries in the thigh, and saphenosaphenous venous connections.
Kibbe et al. performed a retrospective analysis of medical records and helical abdominal computed tomography scans conducted on 50 consecutive patients evaluated in the emergency department because of abdominal pain. It was surprising that 24% ( N = 12) of patients had greater than 50% compression and 66% ( N = 33) had greater than 25% compression. Mean compression of the left common iliac vein was 35.5% (range, 5.6%–74.8%). The structure most often compressing the left common iliac vein against the vertebral body was the right common iliac artery (84%).
The high prevalence and pathologic role of NIVLs in symptomatic chronic venous disease (CVD) patients must be balanced with the frequent prevalence of NIVLs in the asymptomatic general population. These apparent contradictions can be resolved if the NIVL is viewed as a permissive condition predisposing to the development of CVD. Permissive conditions are pathologies that may remain silent until additional insult or pathology is superimposed. Symptom expression in many NIVL obstructions remain asymptomatic, because it probably is a slowly progressive condition. Additional insult or pathology such as trauma, cellulitis, distal thrombosis, secondary lymphatic exhaustion, or reflux, may render the extremity symptomatic. The general principle in these complex pathologies is to treat the permissive condition first, which alone may provide relief, and to prevent recurrence. Correction of secondary pathology may be required only in recalcitrant and advanced cases.
In Raju's series, 75% of limbs with NIVLs and concurrent reflux experienced a good or excellent outcome with stent placement alone, even when the reflux component, severe in many, was uncorrected. These results support the concept that the NIVL plays a permissive role in the genesis of CVD symptoms. NIVLs are ubiquitous in CVD with severe symptoms, and use of IVUS and stent correction when detected is recommended. Even patients with significant distal reflux benefit, thus avoiding or postponing open, reflux-corrective procedures, which are not precluded if the stents were to fail later. An alternative explanation for the observations presented here is to consider NIVLs and distal reflux as a continuum in progressive hemodynamic deterioration of the venous system; symptomatic decompensation occurs when the hemodynamics cross a certain critical threshold. However, no connection between NIVLs and distal reflux has yet been established. It should be emphasized that the hemodynamics of obstructive and reflux pathologies are poorly understood, and their measurement even less so.
Of particular interest is the subset with NIVLs with reflux that became symptom free with stent correction of the NIVL alone, even when the reflux component remained uncorrected. Notably, 67% of stasis ulcers in this subset also healed and remained healed at 2.5 years. CVD symptoms, including stasis ulcers, are not caused by reflux alone; the NIVL plays a role in ways yet to be understood. Ulcers also occur in NIVLs without reflux, although the incidence is higher with reflux.
When symptoms recur after initial remission following stent placement, often stent malfunction is found. Distal migration of the stent with recurrence of the lesion at the iliocaval junction, missed or incomplete treatment of the distal lesion, or, less commonly, in-stent restenoses were found in Raju's series. When corrected, the patient is usually returned to the status of symptom remission.
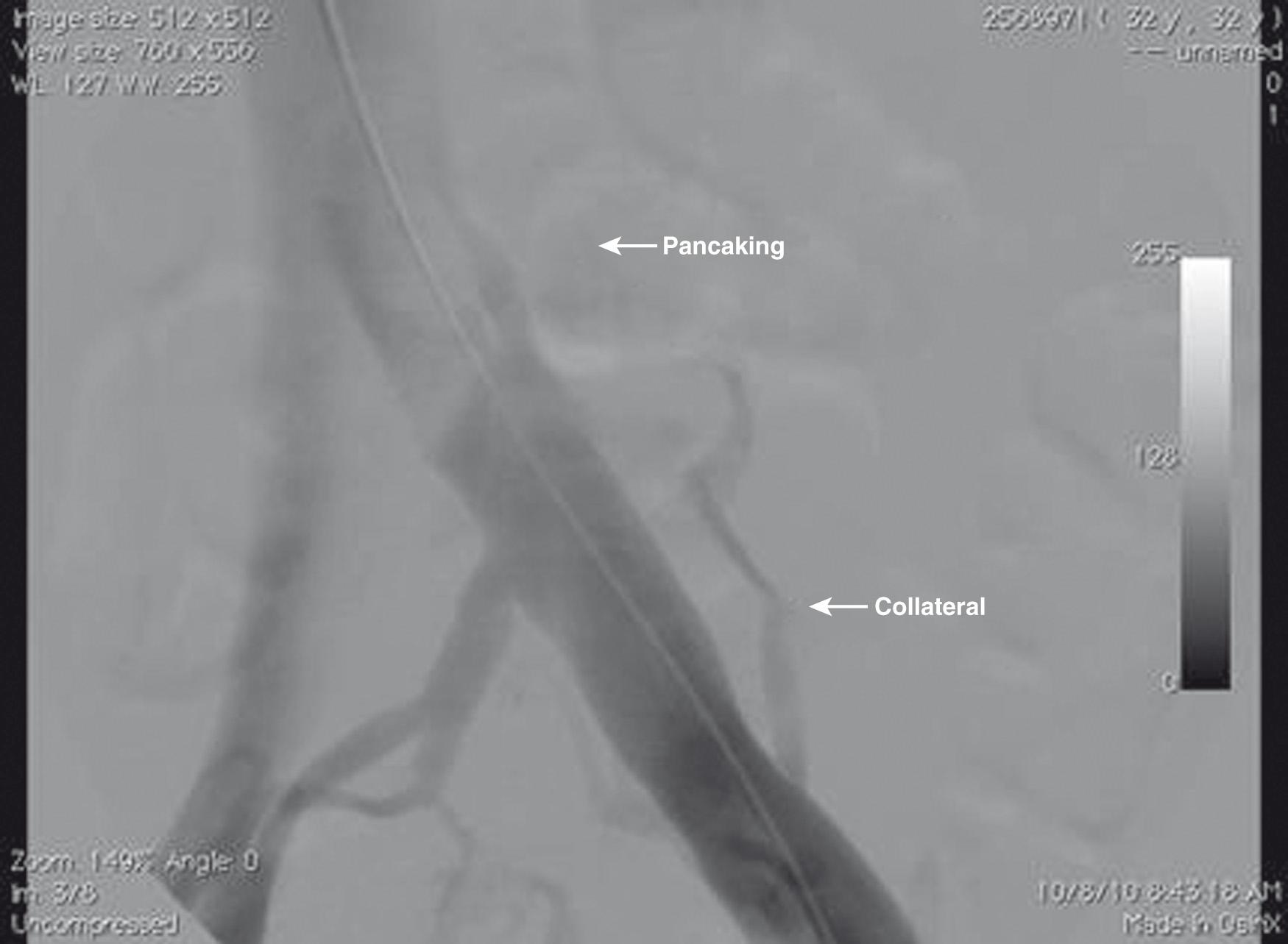
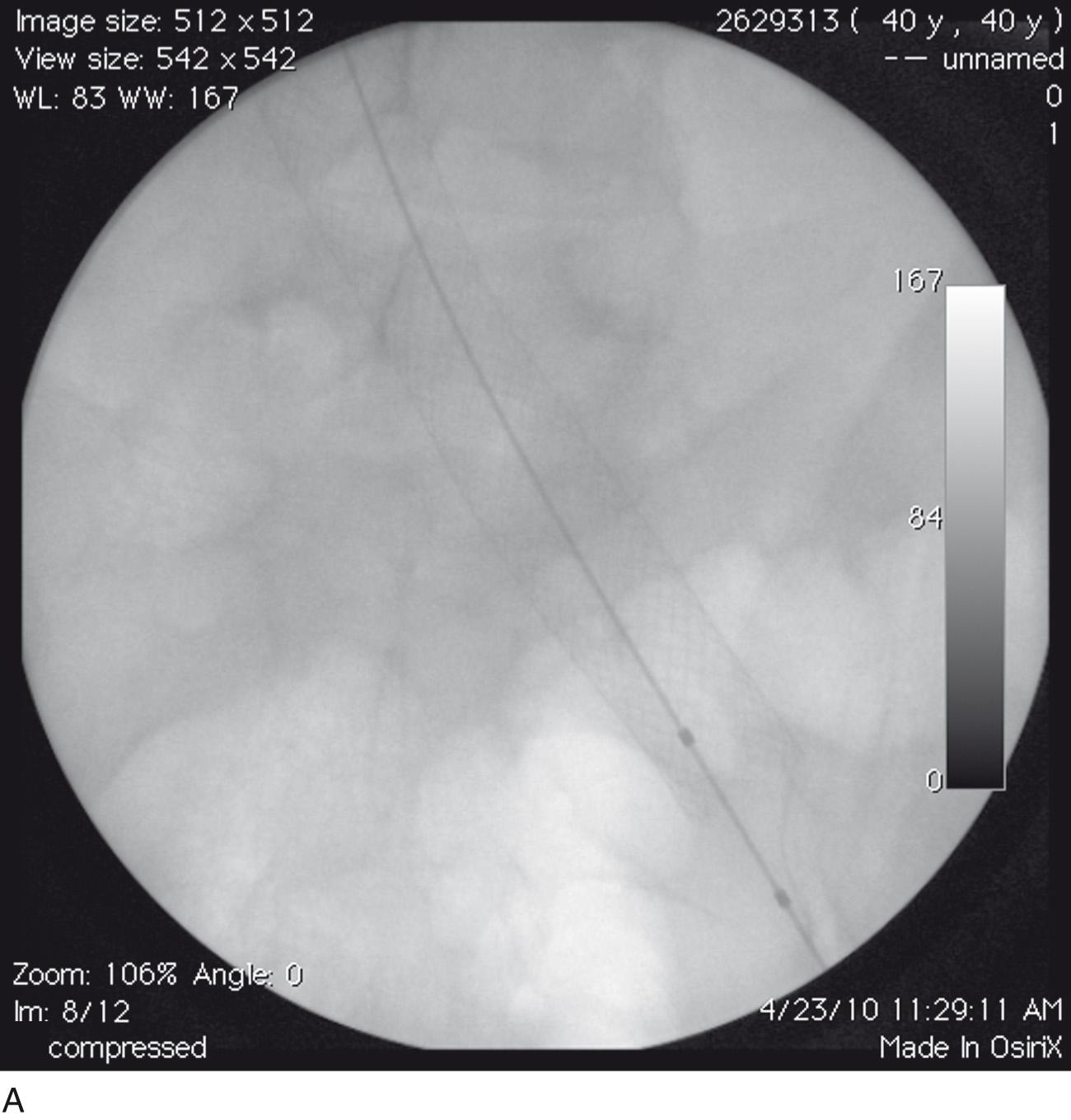
When planning an invasive procedure on a patient, a surgeon preferably enters the operating room with an imaging study demonstrating a pathologic lesion. In the case of iliac vein occlusive disease, this is often not possible. The group out of Mississippi has one of the largest experiences in the world with iliac vein occlusive disease, and they have emphasized the value of intraoperative IVUS for diagnosis and treatment. Their vascular laboratory runs a battery of preoperative noninvasive tests on patients with signs and symptoms of venous disease, and their data demonstrate the insensitivity of these examinations to identify lesions ( Table 18.1 ). Magnetic resonance venography is very operator dependent, and its routine use has not elevated this technique as the gold standard for diagnosis. Perhaps the most interesting phenomenon is the insensitivity of intravenous contrast venography. Although anterior-posterior and oblique views may suggest some “pancaking” of the proximal iliac vein ( Fig. 18.2 ), oftentimes, the common iliac vein appears normal. The poor diagnostic sensitivity of venography was well documented by Negus et al. Of practical importance is that up to half of the cases can be missed if frontal projection venograms alone are relied on for diagnosis.
| Parameter | NIVLs With Reflux ( N = 151) | NIVLs Without Reflux ( N = 181) |
|---|---|---|
| Age, years | 56 (20–85) | 51 (18–90) a |
| Female-male ratio | 110 : 36 (3.1 : 1) | 146 : 31 (4.7 : 1) b |
| Left-right limb ratio | 105 : 46 (2.3 : 1) | 136/45 (3 : 1) b |
| IVUS degree of stenosis (%) | 70 (0–95) | 70 (0–100) b |
| Stenotic area (cm 2 ) | 0.66 (0.15–2.00) | 0.53 (0.02–1.65) a |
| Ambulatory venous pressure | ||
| % drop | 77 (0–97) | 77 (0–99) b |
| venous filling time (s) | 23 (2–132) | 44 (0–165) c |
| APG:VFI 90 (mL/s) | 2 (0–12.3) | 0.9 (0.0–6.0) c |
| Hand-foot pressure differential (mm Hg) | 1 (0–8) | 1 (0–10) b |
| Dorsal foot hyperemia pressure differential (mm Hg) | 6 (0–26) | 5 (0–23) b |
IVUS has become the diagnostic imaging modality of choice. This coaxial technique allows the operator to examine the target lesion as sound waves are emitted from the catheter tip transducer, usually in the 10-MHz to 20-MHz range. A real-time ultrasound image of a thin section of the blood vessel is generated without radiation or nephrotoxic contrast. IVUS has also been used for placement of IVC filters; it is a more accurate method than contrast venography of localizing the renal veins and measuring vena cava diameter.
The patient is taken to the endovascular suite and prepped and draped in the usual manner ( Fig. 18.3A ). The preferred access site is the femoral vein at the upper third of the thigh with the thigh slightly externally rotated and the knee slightly bent. The femoral vein lies inferior to the superficial femoral artery and slightly lateral in most cases. If access is planned via a popliteal approach, then the prone position is preferable, but for the jugular of femoral vein access, the supine position is ideal.

Using ultrasound, a 21-gauge needle is inserted into the femoral vein and an 0.018-inch (0.045-cm) wire placed with Seldinger technique (see Fig. 18.3B ). The 4-Fr microintroducer sheath is placed and used to exchange for a 0.035-inch (0.088-cm) guidewire. Using fluoroscopy, the 0.035-inch (0.088-cm) wire is navigated into the IVC. If the 0.035-inch (0.088-cm) wire meets resistance and has difficulty entering the IVC, an intravenous contrast injection is performed to generate an anatomic roadmap. Most obstructive lesions can be crossed with a 0.035-inch (0.088-cm) glide wire.
To perform contrast venography, a larger sheath (8 Fr, 11 cm in length) is ideal. The power injector is prepared, and a digital subtraction contrast run is prepared by connecting high-pressure tubing from the injector to the side arm of the sheath. Eight mL per second for a total of 20 mL of nonionic intravenous contrast is injected. The resulting image is examined for areas of stenosis, obstruction, and/or the presence of collaterals.
The most common lesion encountered for these cases is a stenosis at the confluence of the left common iliac vein with the IVC. Usually a standard 0.035-inch (0.088-cm) J-tipped guidewire will cross the lesion easily. In cases where the wire does not cross, a 0.035-inch (0.088-cm), hydrophilic, angled-glide wire is selected. Hydrophilic glide wires are slippery by design; thus they are not ideal as working wires for tracking balloons, IVUS catheters, and stents. Therefore the lesion is crossed; a 5-Fr guide catheter is used to exchange the glide wire for a 0.035-inch (0.088-cm) Amplatz super-stiff wire. The super-stiff wire is parked into the subclavian or jugular vein. This maneuver is in anticipation of stent placement and will be explained later.
The IVUS catheter is brought into the field and mounted onto the 0.035-inch (0.088-cm) super-stiff guidewire (see Fig. 18.3C ). IVUS imaging of the entire iliofemoral and caval outflow tract is performed. Particular attention is paid to the caliber of the veins as demonstrated by IVUS. The classic May-Thurner lesion is located at the left, common iliac vein–IVC junction. This is the location where the right, common iliac artery can be visualized as it crosses the left common iliac vein ( Fig. 18.4A–D ). As mentioned earlier, distal NIVLs can be seen where the hypogastric artery crosses the external iliac vein, on either the right or left sides (see Fig. 18.4E and F ). Using the IVUS computerized, planimetry software, the percent area reduction of the stenosis can be calculated by comparing with a normal, adjacent, reference vessel (see Fig. 18.4G ); however, this is not our current practice.
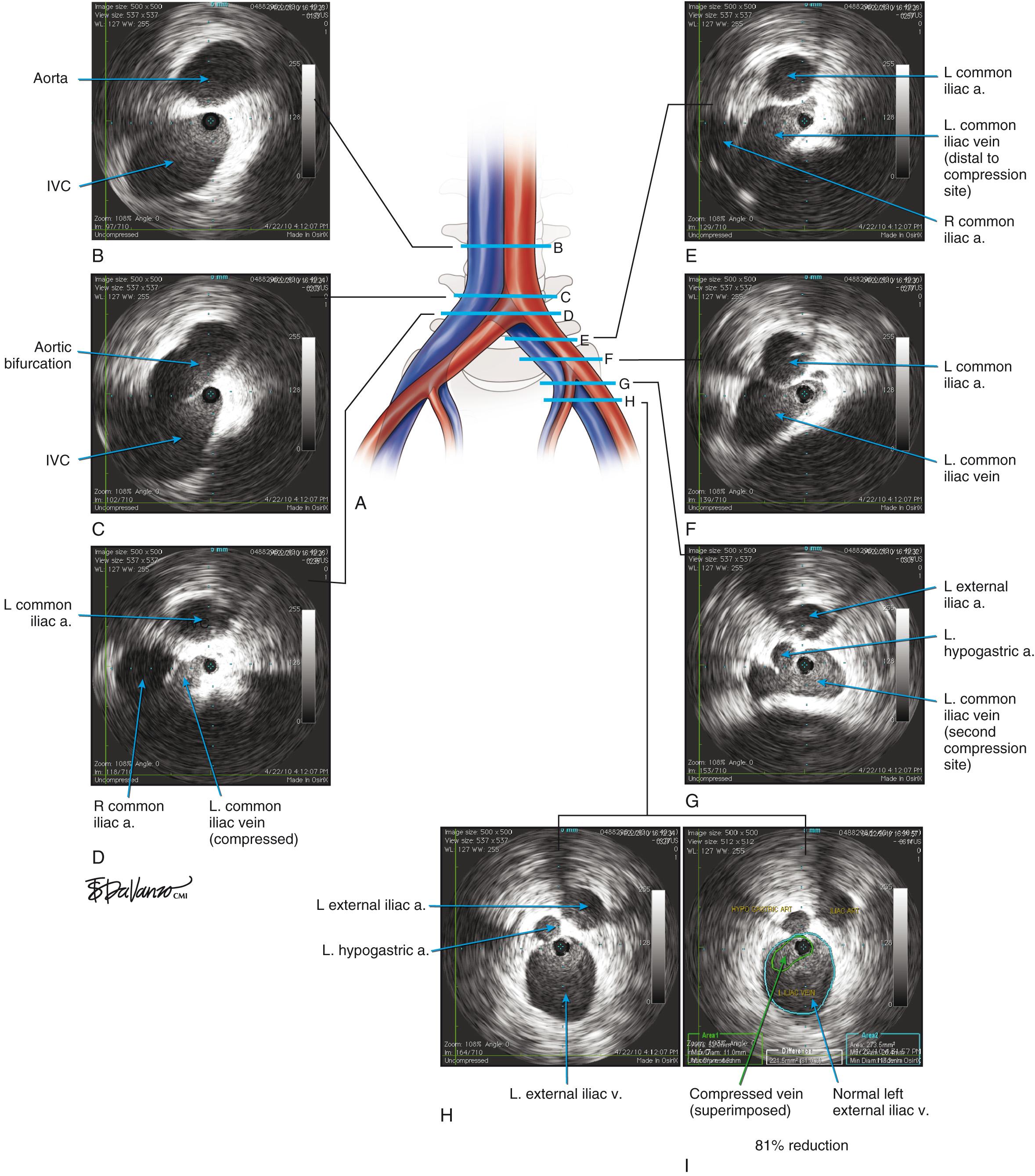
Optimum caliber values described by Raju for the entire iliac-femoral segments are shown in Chapter 2 , Table 2.2 . In current practice, the optimal caliber should be used as a reference in calculating common iliac vein stenosis. There are no validated criteria to determine what percent area reduction constitutes a hemodynamically significant lesion; however, as a rule of thumb, a 50% area reduction is the treatment threshold (see Table 18.2 ).
| Vessel Segment | Diameter | Area |
|---|---|---|
| CIV | 16 mm | 200 mm 2 |
| EIV | 14 mm | 150 mm 2 |
| CFV | 12 mm | 110 mm 2 |
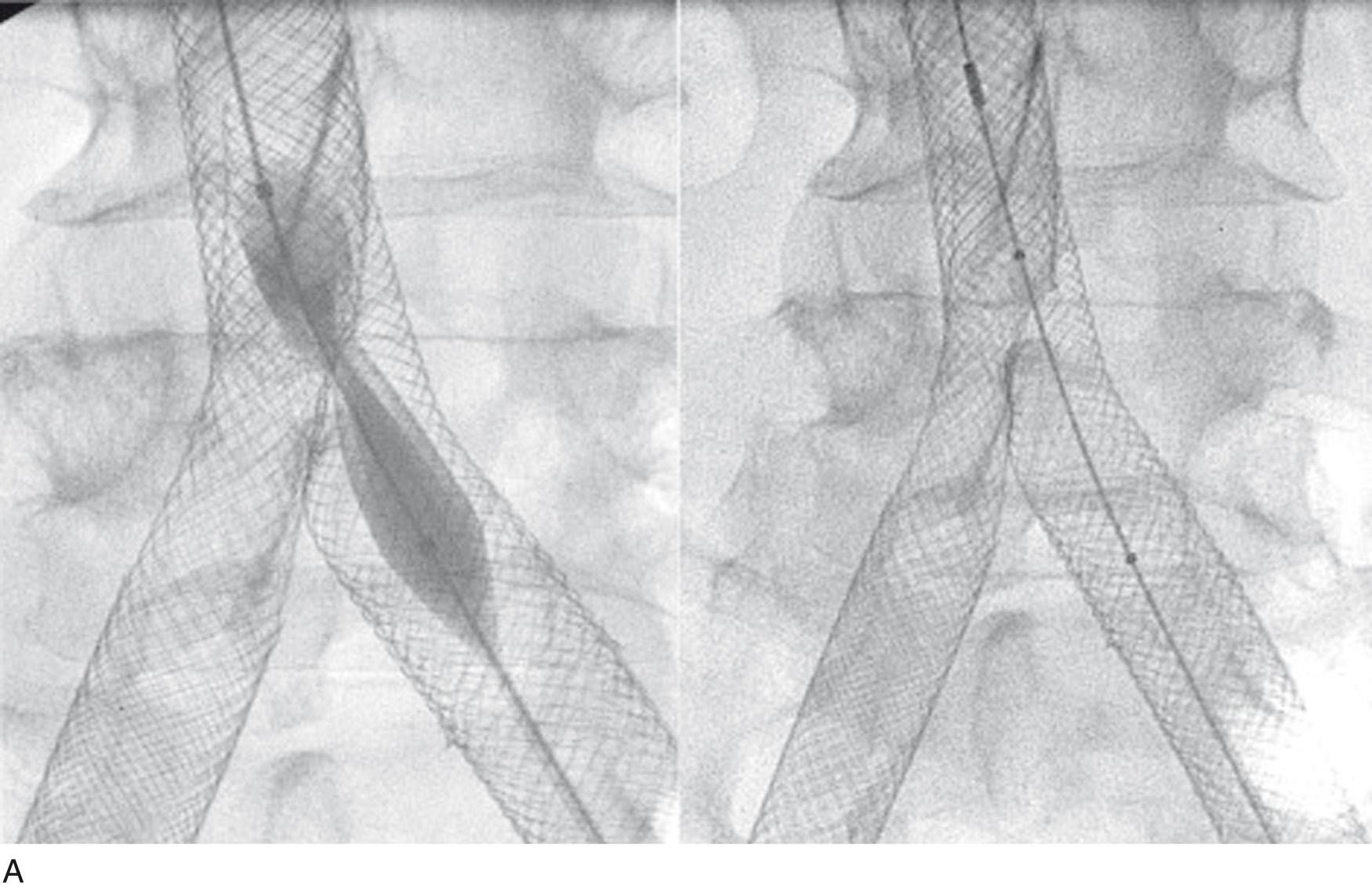
Once the decision to treat is made, a larger sheath, usually 11 Fr, must be placed to accommodate the larger stent delivery systems. In addition, stent delivery systems track easier over 0.035-inch (0.088-cm) stiff wires; therefore, if needed, an exchange must be performed if a stiff wire is not in place. It is critical not to lose access once a lesion has been crossed with a wire and an intermediate step is useful. A 5-Fr guide catheter will track over a glide wire into the IVC and through the heart into the innominate venous system; it can then be subsequently used for 0.035-inch (0.088-cm) stiff-wire placement. After the 0.035-inch (0.088-cm) stiff wire of exchange length is parked in the subclavian or jugular vein, the 5-Fr guide catheter is removed, and a balloon is brought into the field. Iliac veins are quite compliant and fairly resistant to rupture. A 16- to 20-mm-diameter Atlas balloon is usually chosen to dilate the lesion ( Fig. 18.5 ). The balloon is dilated to profile until the waist is obliterated. Sequential dilatations with larger balloons may be required to completely dilate the lesion. Because venous lesions almost always recoil after dilatation, stent deployment is required. Stent diameters of 16 to 20 mm are preferred because oversized stents are necessary. The most common stents used for iliac vein work are self-expanding, braided, Elgiloy Wallstents (Boston Scientific, Nantucket, Mass) ( Fig. 18.6–18.9 ). Gianturco Z-stents (Boston Scientific, Nantucket, Mass) are also used when projecting into the vena cava.

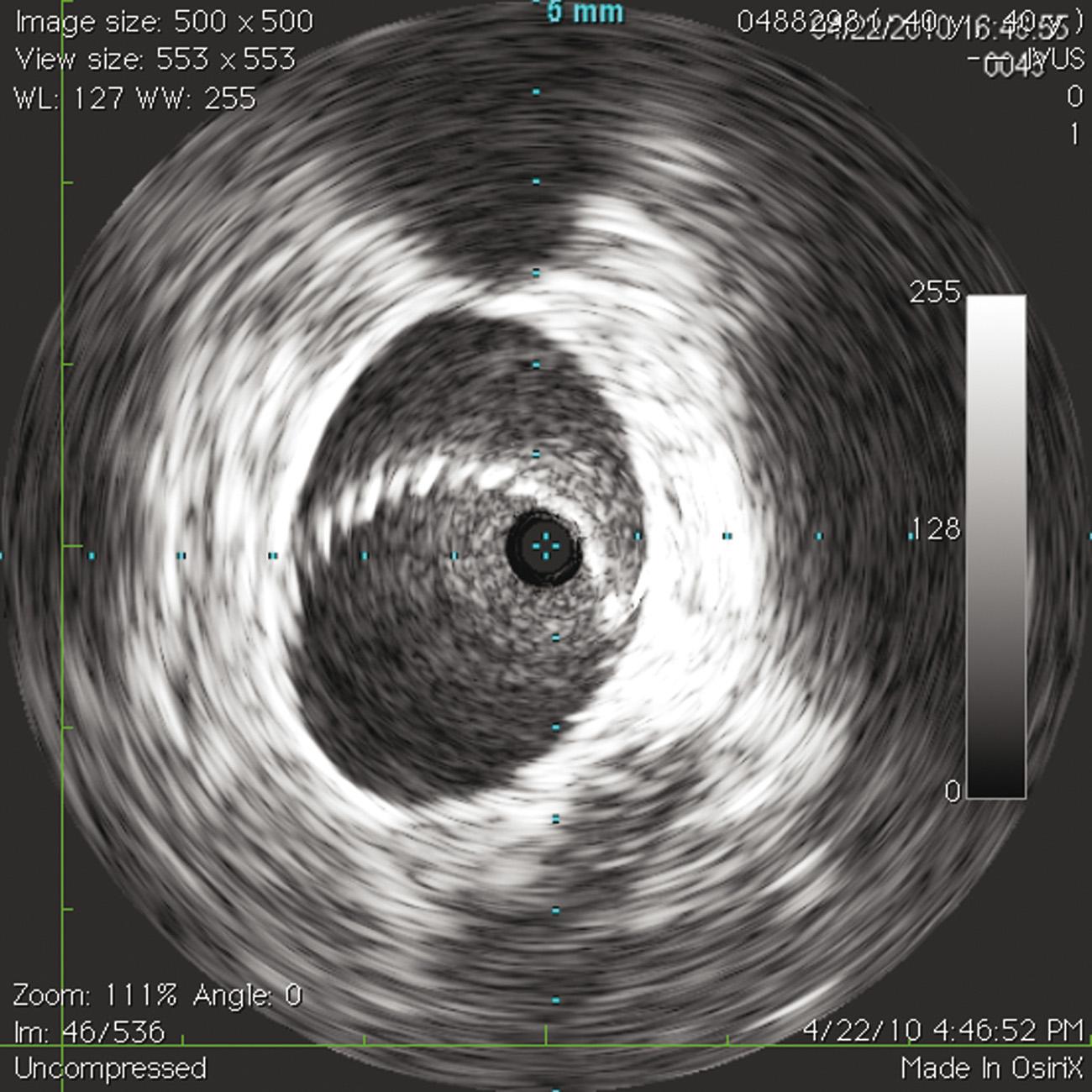
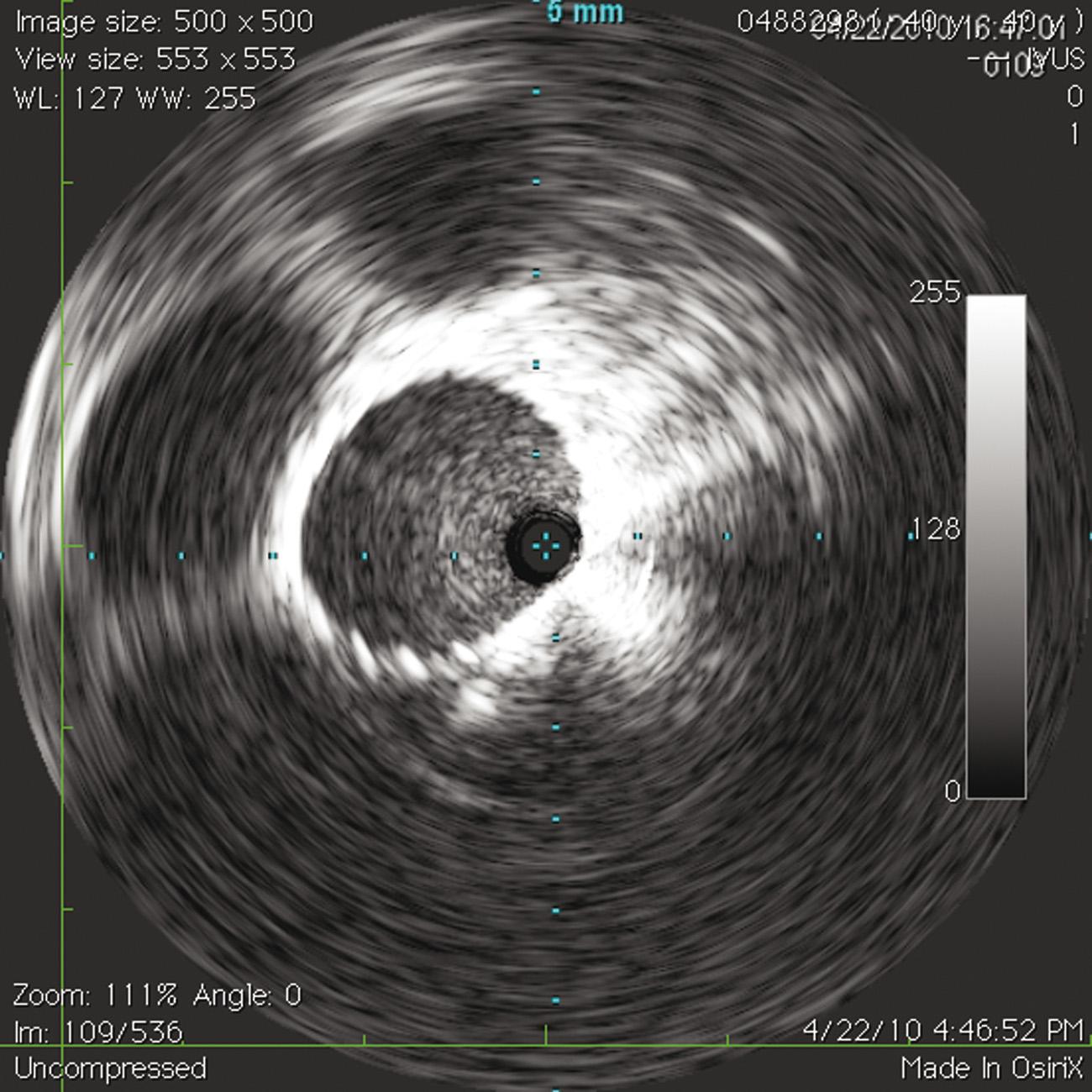
Raju et al. reported that the proximal NIVL was three times more frequently observed on the left side, whereas the distal NIVL was equally distributed bilaterally. The proximal NIVL was typically very focal on the left side and was located at the iliocaval junction; the right proximal NIVL was less focal and was located 1 to 2 cm distal to the iliocaval junction. The median area of the more severe stenosis (proximal or distal), as measured by IVUS, was 0.58 cm 2 (normal, 1.5 cm 2 ) representing approximately 70% stenosis. Most NIVLs were “soft” compared with postthrombotic syndrome (PTS) or arterial lesions, with waisting of the balloon often relieved at less than 2 atm.
The most dreaded complication is losing a stent and finding it in the heart. The phenomenon results when stents “jump” during deployment. Stents are packaged tightly in delivery sheaths where their potential energy is stored. During deployment, the potential energy converts to kinetic energy as it expands and finds its resting place. The stent will then apply its outward radial force to the vessel wall and maintain an open vessel.
If the stent has the opportunity to find an open area to quickly release its energy, it will. Iliocaval stent deployment for NIVL routinely deploys across a tight iliocaval stenosis into the IVC. The IVC represents a large space where a stent may quickly, and uncontrollably, convert its potential energy into kinetic energy. Thus the stent could jump into the IVC and float into the right ventricle if the operator is not careful.
Aside from careful deployment and stent oversizing, an important maneuver is parking the distal guidewire into the innominate, subclavian, or jugular vein before stent deployment. This technique will keep the stent “on a rail,” or not allow migration into the right atrium, the tricuspid valve, or worse, into the right ventricle. Stent retrieval with a snare, or capturing it with a balloon, and redeploying it in another vessel is much easier when the stent is on a wire.
In four studies, with a total of 1000 lower extremities, NIVL was specifically assessed. Technical success was achieved in 96% to 100% of cases, with a follow-up of 59 months (6–72 months). Primary patency (where the vein is open without any additional intervention) was 85% (79%–99%), and assisted primary (where the vein is patent, but an additional intervention is needed to keep it so) and secondary patencies (where the vein is patent after one or more additional interventions were required to treat an occlusion of the vein) were 100%. Rates of ulcer healing ranged from 82% to 85%, with 5% to 8% recurrence. There was statistically significant improvement at all points of the Chronic Venous Insufficiency Questionnaire (CIVIQ) and in the Visual Analogue Scale and Quality of Life scores. Edema decreased in 32% to 89% of cases, and hyperpigmentation improved in 87%.
Because of the considerable incidence of iliocaval thrombosis in patients with known DVT, clinical examination should include evaluating pelvic and abdominal components to ensure that more proximal vessels are not involved and contributing to the lower extremity complaints. Duplex ultrasound (US) allows for good visualization of lower extremity veins; however, for iliocaval disease, computed tomographic venography or magnetic resonance venography may help define the landscape and aid planning venography, IVUS, with or without intervention. For patients with iliocaval disease, the goal of therapy is to improve symptoms; curing the disease is not realistic. In these patients, always remember to document clinical severity with an appropriate index such as the revised Venous Clinical Severity Score (VCSS), Villalta score, and Comprehensive Classification System for Chronic Venous Disorders (CEAP) scores.
It has been shown that in two-thirds of patients with postthrombotic disease, it is necessary to implant stents down to the groin below the inguinal ligament to improve inflow into the reconstructed iliac veins. In a report by Raju, the common femoral vein was stented to the lower landing zone in 22 cases (56%). When the common femoral vein was occluded or stenosed, inflow from the profunda femoris vein was enough to maintain stent patency. When both the profunda and femoral veins have obstructive lesions, stents can be extended into them, but in this situation, there is a high risk of stent thrombosis because of poor inflow. If the popliteal vein is occluded, it may require tibial vein access to recanalize the popliteal and femoral veins to obtain inline flow.
Interventions distal to the groin, including endovenectomy or stenting further down into the femoral vein or profunda femoral vein, are also under investigation in select cases.
Once operative planning has begun, it is important to properly choose an access site. If the femoral vein is patent, it can be used for access to larger vessels. If the femoral vein is occluded, then venous drainage from the popliteal and profunda femoris veins should be evaluated. If the popliteal and profunda femoris veins are patent, the most proximal segment of an occluded femoral vein may often still be accessed. On occasion, it may be necessary to access the proximal profunda femoris vein, which may be challenging because of its depth.
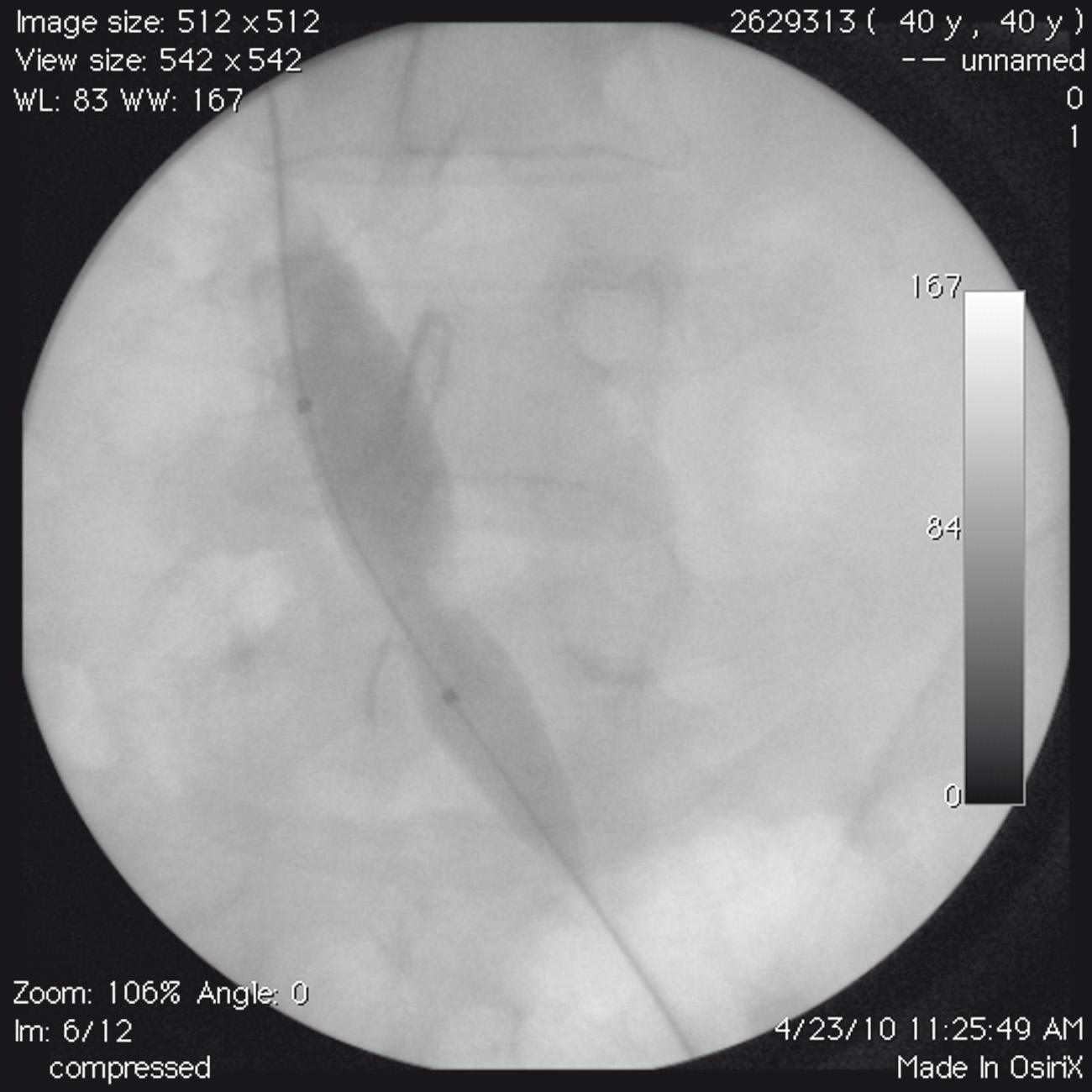
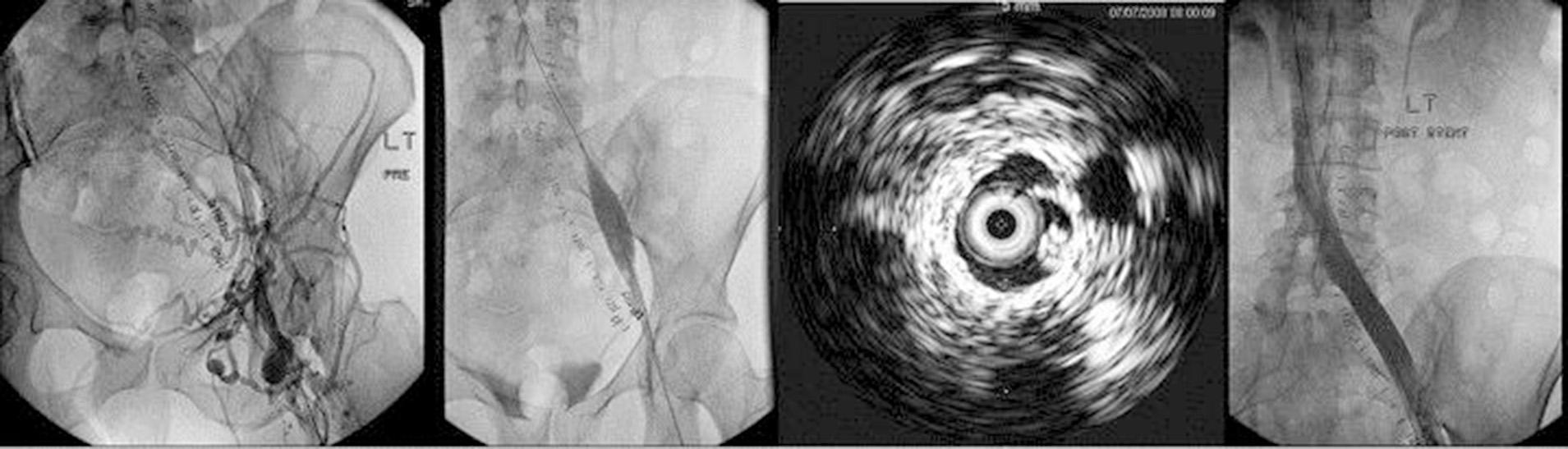
Patients presenting with iliac vein occlusive disease secondary to thrombosis are much more difficult to deal with technically, and stent patency is inferior to that of NIVL cases. Recanalization techniques are required ( Fig. 18.10 ). General endotracheal anesthesia is preferred for management of the airway in pain. A Foley catheter is placed for urinary drainage because these procedures can become lengthy.
Femoral vein access under US guidance is preferred at the midthigh level. The femoral vein is found posterolateral to the artery at midthigh. Midthigh access facilitates shorter-length instrumentation with superior pushability compared with popliteal or internal jugular access sites. We prefer an 11-Fr sheath of 11-cm length to allow space cephalad to the sheath and below the inguinal ligament to land a stent into the common femoral vein when necessary. The profunda femoris vein is usually open if the femoral vein is occluded and can be accessed 2 to 3 cm below the lesser trochanter; stent extension into the profunda femoris vein is performed without impeding inflow from an occluded femoral vein. If the femoral vein is occluded, access is often possible through the upper 3 to 5 cm of the vein, which tends to remain open.
To cross a chronic total occlusion (CTO), an antegrade venogram is performed via the sidearm of the sheath to define venous anatomy at the groin and pelvis. A 0.035-inch (0.088-cm) soft-glide or stiff-glide wire (Terumo Inc, Ann Arbor, Mich) is navigated up to the occlusion. Further progress into the occlusion is made with vigorous rotation of the glide-wire tip with a torque device; the enhanced kinetic energy at the wire tip facilitates wire passage into microchannels present in the organizing fibrous tissue within the vein. Usually a straight or angled support catheter (Quick-Cross support catheter; Spectranetics, Colorado Springs, CO, or CXI support catheter; Cook, Bloomington, IN) is required to facilitate progress. If added support is required, we prefer the Triforce system (Cook Medical, Bloomington, IN). This 5-Fr braided sheath with tungsten tip adds columnar strength to the inner 4-Fr CXI support catheter and a nice transition between the two devices placed coaxially.
Glide wire passage must be guided by knowledge of topographic course of the vein. In the frontal projection, the left femoral vein overlies the medial third of the femoral head, coursing up to the lower pelvic brim across the sacroiliac joint joining the IVC variably between the fourth and fifth lumbar vertebral bodies. The right femoral and iliac veins course in a straighter line (frontal projection) to their junction with the IVC. It is useful to view progress of the recanalization intermittently by rotating the C-arm gantry into 45-degrees or 60-degrees oblique projections to ensure that the glide wire initially follows the curve of the sacrum and then turns anteriorly towards the promontorium and anterior to the spine. It is critical to recognize that the glide wire may enter collaterals and tributaries. Interval contrast injections (puff angiograms) will help aid progress into the correct anatomy. An angled-tip catheter is useful in redirecting the glide wire in the proper direction when it seems to veer off course.
Passage of the glide wire away from the expected course of the vein with sudden ease denotes perforation. The glide wire can be withdrawn and usually manipulated in the proper direction without sequelae. Withdrawal of blood through the catheter may or may not be possible during the recanalization process and has no particular significance as long as the glide wire tracks approximate to normal anatomy. Entry into the IVC should be confirmed by fluoroscopy, contrast injection through a catheter placed in the IVC, and IVUS.
From this stage of the recanalization procedure, the use of IVUS becomes crucial to assure integrity of the recanalized channel, to select optimal proximal and distal landing sites preferably free of postthrombotic disease, to ensure proper deployment and expansion of the stents, and to minimize radiation exposure. The recanalized channel may be dilated, starting with smaller-sized (3-mm) balloons to allow passage of an 8-Fr IVUS catheter and large-caliber balloons. It is useful to use high-pressure balloons (16–18 atm) expanded at maximum level for at least a minute until the balloon pressure stabilizes at this level. Overdilatation and oversizing of the stent diameter by 2 to 4 mm for the anatomic location is recommended to compensate for the variable recoil of the recanalized channel. Optimal stent diameters after recoil are 18 mm for the common iliac vein, 16 mm for the external iliac vein, and 14 mm for the common femoral vein in normally sized adults. Self-expanding woven braided Elgiloy stents (Wallstent, Boston Scientific, Nantucket, Mass) in series with 3-cm to 4-cm overlap to minimize shelving along the complex course of the iliac vein are used. Because multiple stents are typically required, the maximum manufactured length for the various diameter sizes (typically 7-cm to 9-cm length) should be used, restricting shorter lengths for use at either end of the stack to tailor length. A completion IVUS examination and venogram terminate the procedure after noted defects are corrected by repeat ballooning. Patients are discharged home the same day.
Patients may require stenting of both limbs. Several techniques have been described by Neglén, but most noteworthy is the fenestration technique ( Fig. 18.11 ).
Occasionally, one may encounter very recalcitrant lesions where sharp recanalization techniques should be considered (i.e., stiff wire, Rosch-Uchida needle). In addition, access from above and below may be required to snare a wire to get through-and-access across the lesion (“body floss” technique). More advanced techniques and details of the endovascular instrumentation required will be discussed at the end of this chapter.
Previously placed IVC filters incorporated in the occluded caval segment or present above the occlusion in a patent segment pose a special technical problem. In the former instance, the filter must be displaced sideways or remodeled/fractured by repeated high-pressure balloon dilation to allow stent placement. In the latter case, the filter implantation site must be assessed for significant associated stenosis. If present, the IVC filter should be disrupted or displaced for placement of the stent across the stenosis; otherwise, it is left alone.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here