Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The definition of the clinical syndrome of idiopathic ventricular fibrillation (IVF) has evolved over time and continues to do so. Historically, the term IVF was used to describe polymorphic ventricular tachycardia (VT)/ventricular fibrillation (VF) in the absence of ischemia, structural heart disease (SHD), or reversible metabolic-toxicologic conditions. As our ability to characterize, diagnose, and manage inherited arrhythmia syndromes has improved both clinically and genetically, the proportion of cases that are labeled as IVF has declined.
A detailed characterization and in-depth understanding of IVF has been difficult because it is an uncommon condition that, by definition, is a diagnosis of exclusion. IVF accounts for less than 10% of all VF episodes; however, IVF plays a major role in the context of unexplained cardiac arrest in otherwise healthy individuals. ,
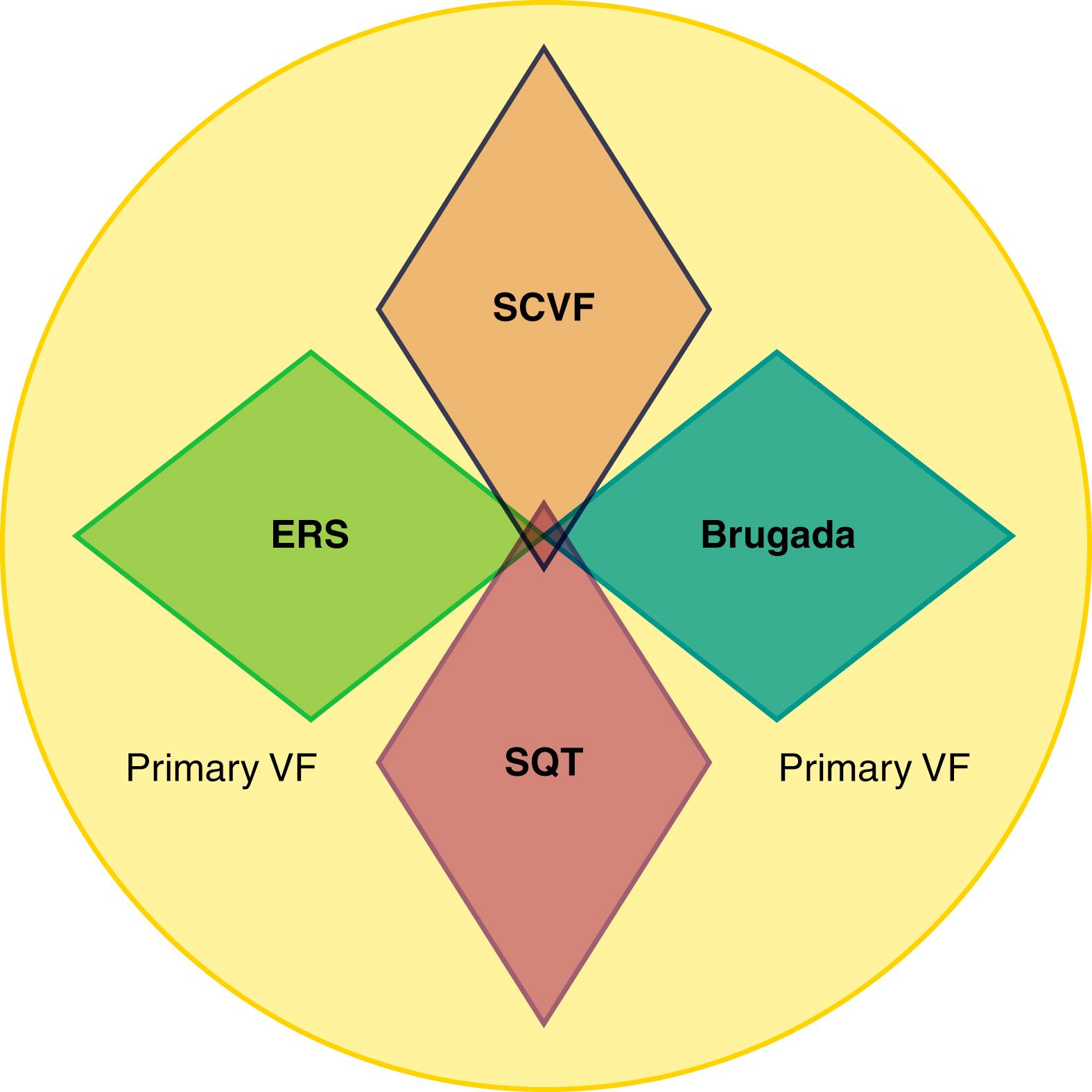
IVF has historically been an inclusive term for unexplained episodes of VF or sudden death but should now rather be considered as a descriptive working diagnosis from which a growing number of distinct primary electrical disorders with unique clinical and molecular features are identified. Because of this, the interpretation and applicability of the previous literature related to IVF is often confounded by the fact that the populations described were heterogeneous and included cases with other primary electrical conditions, such as Brugada syndrome, early repolarization (ER) syndrome, or short QT syndrome (SQT; see Chapter 96 ).
We prefer the term unexplained cardiac arrest because it applies to the apparently unexplained VF survivor, which can then be de-differentiated into etiologies based on a combination of deep phenotyping and monitoring for recurrence. This chapter covers the overarching unexplained cardiac arrest population with historically termed IVF, with a focus on the distinct arrhythmogenic syndrome that has gained attention under the IVF umbrella of short-coupled ventricular fibrillation (SCVF). There is now growing evidence that many previous reports of IVF actually described case series of SCVF, and our current understanding of this novel primary electrical disorder is summarized.
The 2013 Heart Rhythm Society (HRS)/European Heart Rhythm Association (EHRA)/Asia Pacific Heart Rhythm Society (APHRS) Expert Consensus on inherited arrhythmia defined IVF as “a resuscitated cardiac arrest victim, preferably with documentation of VF, in whom known cardiac, respiratory, metabolic, and toxicological etiologies have been excluded through clinical evaluation.”
This definition for the working diagnosis of IVF should be differentiated from bradycardia/pause-dependent VF/torsades de pointes and from SCVF. Reflecting its distinct electrophysiologic features, the following definition has been proposed for SCVF (presence of all required): (1) documentation of VF or polymorphic VT initiated by a PVC with a coupling interval of less than 330 ms; (2) absence of QTc prolongation; (3) absence of preceding bradycardia (heart rate <60 beats/min) or preceding sinus pause (>3 seconds) or R-R interval more than 3 seconds in the case of a ventricular paced rhythm or atrial fibrillation; (4) absence of type 1 Brugada pattern (spontaneous or inducible), early repolarization pattern, or SQT according to current definitions and guidelines at the index cardiac arrest or during follow-up; (5) absence of structural heart disease or other primary electrical disorder or arrhythmogenic cardiomyopathy; and (6) absence of reversible metabolic or pharmacologic/toxicologic conditions causing similar electrophysiologic findings.
The majority of patients with SCVF have a normal resting electrocardiogram (ECG) with an unremarkable corrected QT interval (QTc) and no J-point abnormalities. Nevertheless, subtle repolarization abnormalities may be present, with a variable degree of overlap of SQT syndrome (SQTS), ER, and SCVF in our current understanding ( Fig. 100.1 ). For example, the ER pattern is overrepresented in IVF patients , ; these patients have subsequently been “hived off” into a category called ER syndrome (ER pattern and symptoms). Similarly, evidence supports a weak male preponderance and shorter QTc intervals in IVF compared with the normal population. The most extreme of these have been defined as what is now formally called SQTS. One study reported QTc intervals of 360 ms or less in 35% of male patients with IVF compared with only 10% in healthy controls, with no patient meeting the formal criteria for SQTS. A substudy of the Japan Idiopathic Ventricular Fibrillation Study (J-IVFS) registry found mild PR and QRS prolongation in 22.5% of a small IVF cohort without signs of ER. The findings were unrelated to clinical end points or the recurrence of VF. This is discussed in more detail later in this chapter.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here