Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nearly 37 million people were living worldwide with human immunodeficiency virus (HIV) infection in 2016, and about 2 million become infected every year.
HIV testing is recommended as a component of routine medical care, not just in individuals with known risk factors, including patients with cancer.
Acquired immunodeficiency syndrome (AIDS) is defined as HIV infection associated with an absolute CD4 count below 200/µL (age 6 and older) and/or an AIDS-defining opportunistic infection or AIDS-defining cancer, including Kaposi sarcoma, non-Hodgkin lymphoma, and cervical cancer.
About 40% of HIV-associated malignancies are associated with oncogenic viruses, including human papillomavirus (HPV), Epstein-Barr virus (EBV), and human herpesvirus 8 (HHV-8).
Although the incidence of AIDS-associated cancers has declined with combination antiretroviral therapy (cART), the incidence of other cancers has increased owing to aging of the HIV population and twofold higher rates of tobacco use than in the general population.
The prognosis for patients with HIV-associated lymphoma, Hodgkin lymphoma, and anal carcinoma is similar to the prognosis for patients in the general population, although cancer morality rates are higher in other cancers.
cART should be continued in those with HIV infection and cancer but may need to be modified to avoid drug-drug interactions with antineoplastic therapy.
Infection prophylaxis is required for those with severe immune deficiency and those receiving antineoplastic therapy associated with immune suppression. Colony-simulating factors are also commonly used to prevent neutropenic infections associated with chemotherapy.
About 37 million people were living worldwide with human immunodeficiency virus (HIV) infection in 2016 ( http://aidsinfo.unaids.org/ ). HIV testing is recommended as a component of routine medical care, not just individuals with known risk factors, including patients with cancer. Acquired immunodeficiency syndrome (AIDS) is defined as HIV infection associated with an absolute CD4 count below 200/µL (age 6 and older) and/or an AIDS-defining opportunistic infection or AIDS-defining cancer, including Kaposi sarcoma (KS), non-Hodgkin lymphoma (NHL), and cervical cancer. Combination antiretroviral therapy (cART) has led to substantial declines in mortality in HIV-infected individuals in the United States and worldwide, including mortality associated with HIV-associated cancers. Although overall mortality and the incidence of AIDS-associated cancers has declined with cART, other cancers have increased owing to aging of the HIV population and twofold higher rates of tobacco use than in the general population. About 40% of HIV-associated malignancies are associated with oncogenic viruses compared with 4% for malignancies in the general population. Oncogenic viruses include human papillomavirus (HPV), associated with cervical, anal, and oral cancer; Epstein-Barr virus (EBV), associated with Hodgkin lymphoma and NHL; human herpesvirus 8 (HHV-8), associated with KS, primary effusion lymphoma, and multicentric Castleman disease; and hepatitis B and C viruses, associated with liver cancer. The prognosis for patients with HIV-associated lymphoma, Hodgkin lymphoma, and anal carcinoma is similar to the prognosis in the general population, although cancer morality rates are higher in other cancers. Although cART should be continued in individuals with HIV infection and cancer, the regimen may need to be modified to avoid drug-drug interactions with antineoplastic therapy. Infection prophylaxis is indicated for those with severe immune deficiency, or those receiving antineoplastic therapy associated with immune suppression in accordance with established guidelines. Colony-simulating factors are indicated to prevent neutropenic infections associated with chemotherapy.
HHV-8, also known as Kaposi sarcoma–associated herpesvirus (KSHV), was first isolated from KS lesions in patients with AIDS in 1994 and was also found to be the etiologic agent for lymphoproliferative disorders such as primary effusion lymphoma and multicentric Castleman disease. There are substantial geographic differences in HHV-8 seroprevalence, ranging from more than 50% in endemic areas such as Africa, 10% to 25% in the Mediterranean, and less than 10% in North America, Northern Europe, and most of Asia. A meta-analysis including 93 studies with 58,357 subjects found that HIV-infected individuals were about 2-fold more likely to be HHV-8 seropositive than HIV-negative persons, with the strongest association among men who have sex with men, hemophiliacs, and children, in whom this relative risk increased about 4-fold, 3-fold, and 2.5-fold, respectively. Groups associated with about a 1.5-fold higher HHV seroprevalence included heterosexuals, injection drug users, and pregnant women. Thus HIV infection was associated with an increased HHV-8 seroprevalence in all population groups examined. The authors concluded that better understanding of HHV-8 transmission in different age and behavioral groups is needed in order to develop strategies to prevent HHV-8 transmission. Although the incidence of AIDS-associated KS has declined substantially since the routine use of cART in clinical practice, the risk of developing KS remains elevated by about 800-fold in patients with AIDS compared with the general population.
There are four different epidemiologic variants of KS that share common histologic features. AIDS-associated KS is the most aggressive variant that occurs in Western countries and sub-Saharan Africa, and often resolves with cART and immune reconstitution, but in some cases may be progressive despite control of HIV infection and immune reconstitution. Other forms not typically associated with HIV infection include (1) classic KS, an indolent variant with skin tumors affecting elderly men with Mediterranean or Eastern European ancestry, (2) endemic KS, including an aggressive lymphadenopathic variant occurring in children and a chronic cutaneous variant occurring in adults in sub-Saharan Africa, and (3) iatrogenic KS, associated with immunosuppressive therapy after organ transplantation, which usually regresses with immune reconstitution.
KS is an angioproliferative tumor that originates when HHV-8 infects cells of endothelial lineage and maintains replication during host cell division. Only a few HHV-8 genes are expressed in latent infection, whereas multiple genes (KSHV ORF74, viral interleukin-6, vIRF1, vIRF2, vIRF4 ) that promote endothelial cell proliferation, angiogenesis, and release of inflammatory cytokines are expressed during lytic infection when viral replication occurs.
Early initiation of cART in HIV-infected individuals is the only established preventive strategy. No effective early detection method currently exists.
Definitive diagnosis requires punch biopsy of the skin or biopsy of lymph nodes or other involved areas. Histologic examination reveals angioproliferative features combined with spindle-shaped cells, abnormal and leaky blood vessels, and an inflammatory infiltrate ( Fig. 62.1A ). Although the clinical presentation is fairly typical, the differential diagnosis includes bacillary angiomatosis, a vascular, proliferative form of Bartonella infection that occurs usually in immunocompromised individuals, including those with HIV infection, and that may also be diagnosed with skin biopsy. Disease most commonly involves the skin, oral cavity, and gastrointestinal tract but may also involve lymph nodes, lungs, and other organs.

Examples of clinical presentations associated with KS are shown in Fig. 62.1B-C . Most patients develop macular, papular, nodular, or plaquelike cutaneous lesions on the trunk and extremities and sometimes the face and oral cavity. The color of lesions ranges from pink to red or purple. Disease commonly involves the feet and legs and may be associated with edema, pain, and ulceration. Lymph nodes and visceral organs may also be involved, including the lung and gastrointestinal tract.
Staging requires at a minimum physical examination including the oral cavity and entire skin. Endoscopy, colonoscopy, or bronchoscopy may be indicated in patients with suspected gastrointestinal or pulmonary involvement, respectively. Evaluation of visceral disease should be performed in patients according to symptoms (e.g., cough, abdominal pain) and signs (e.g., hepatosplenomegaly). AIDS-associated KS is staged with the AIDS Clinical Trials Group TIS (tumor burden, immune status, systemic illness) staging system ( Table 62.1 ).
| Good Risk | Poor Risk | |
|---|---|---|
| (Any of the following) | (Any of the following) | |
| T (0) | T (1) | |
| Tumor extent (T) | Confined to skin and/or lymph nodes and/or minimal oral disease a | Tumor-associated edema or ulceration |
| Extensive oral KS b | ||
| Gastrointestinal KS | ||
| KS in other nonnodal viscera | ||
| I (0) | I (1) | |
| Immune system (I) c | CD4 cells ≥200/µL | CD4 cells <200/µL |
| S (0) | S (1) | |
| Systemic illness (S) | No history of opportunistic infections or thrush | History of opportunistic infections and/or thrush |
| None of the following “B” symptoms present: unexplained fever, night sweats, >10% involuntary weight loss, or diarrhea persisting >2 wk | “B” symptoms present | |
| Karnofsky Performance Status score ≥70% | Karnofsky Performance status score <70% | |
| Other HIV-related illness (e.g., neurologic disease or lymphoma) |
a Minimal oral KS is nonnodular KS confined to the palate.
b Extensive oral KS: nodular lesions (raised) and/or lesions in areas of the mouth besides the palate.
c New studies have revealed that cutoff of CD4 count at 150/µL rather than 200/µL might allow better discrimination among prognostic groups.
A proposed management algorithm is shown in Fig. 62.2A . Key considerations in management include the location, extent, and type of skin lesions, immune function, and control of underlying HIV infection.
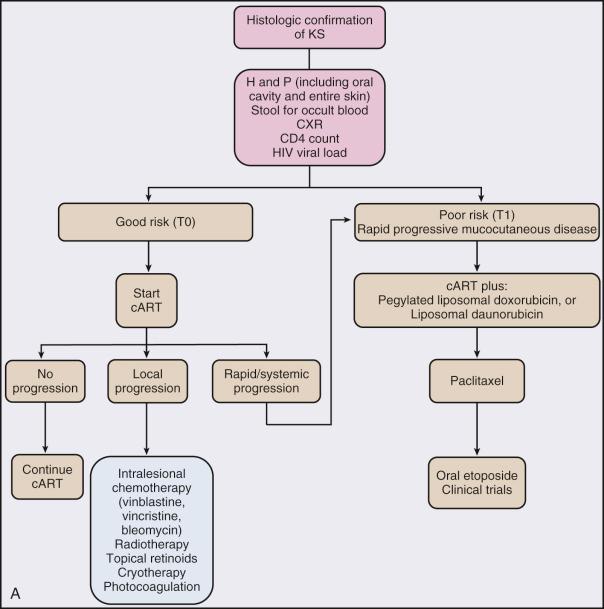
The use of cART is a cornerstone of therapy for patients with HIV-associated KS. cART inhibits HIV replication, enhances immune response against HHV-8, and may contribute to disease regression. Patients with early KS (T0) can achieve disease regression with cART alone. Patients with advanced KS (T1) may receive local therapy (e.g., intralesional chemotherapy [vinblastine, vincristine], topical ointments [alitretinoin, imiquimod], radiotherapy, cryotherapy, and/or surgical excision) if there are limited lesions. Systemic chemotherapy is indicated if there is widespread cutaneous disease, rapidly progressive disease, or visceral compromise. A systematic review of cytotoxic therapy for KS identified 26 studies over a 30-year period. The authors concluded that the eligible trials were of poor quality, and that the lack of standardized classification of disease activity and clinical outcomes precluded comparison of treatments. Subsequently, a prospective phase III trial comparing paclitaxel and pegylated liposomal doxorubicin showed comparable median progression-free survival and 2-year survival, although there was more toxicity in the paclitaxel arm; both agents produced significant improvement in pain (69%) and swelling (95%). Cytochrome P450, an important metabolic pathway for several chemotherapy drugs, is inhibited by protease inhibitors. However, despite higher exposure to paclitaxel, patients who took protease inhibitors while receiving paclitaxel did not have increased toxicity, suggesting that no dose adjustment is required for patients receiving paclitaxel concurrently with protease inhibitors that inhibit cytochrome P450.
A variety of other therapeutic strategies have been associated with objective tumor regression in KS. HHV-8 activates the PI3K pathway, and mammalian target of rapamycin (mTOR) inhibitors such as rapamycin have shown activity. Platelet-derived growth factor and c-KIT receptors are activated by HHV-8 and inhibited by imatinib, which also has shown activity. Antiangiogenic agents such as the vascular endothelial growth factor (VEGF-A) antibody bevacizumab have likewise been associated with response. Tumor necrosis factor–α (TNF-α), interleukin-6 (IL-6), VEGF, and CD4-CD8 costimulation are important steps in KS pathogenesis, which can be interrupted with immune modulators such as lenalidomide and pomalidomide. Current strategies being evaluated include treatment with pomalidomide alone (NCT01495598) or in combination with liposomal doxorubicin (NCT02659930), antiangiogenic agents targeting ephrin B2 (NCT02799485) or VEGF (NCT00923936), and immune checkpoint blockade with the anti-PD-1 antibody pembrolizumab (NCT02595866) or nivolumab plus the anti-CTLA4 antibody ipilimumab (NCT02408861).
In developed countries, the relative increase in risk of NHL in HIV infection has declined significantly since the advent of cART from about 80-fold to 10- to 20-fold. The median CD4 count at NHL diagnosis has increased, and median HIV RNA levels have decreased in the cART era. In contrast, Hodgkin lymphoma risk in people living with HIV (PLHIV) is less strongly associated with immunosuppression, and the relative increased risk has remained relatively stable at around 10- to 20-fold.
HIV infection itself appears not directly involved in carcinogenesis but results in disrupted immune surveillance of tumor antigens and oncogenic viruses. It also provides a milieu of chronic antigen stimulation, cytokine dysregulation, and genetic alterations, which is permissive for lymphomagenesis. The two oncogenic human gammaherpesviruses, EBV and HHV-8, are involved in lymphoma pathogenesis. EBV is present in more than 30% of all HIV-associated lymphomas. The EBV genome is present in virtually all cases of primary central nervous system lymphoma (PCNSL) and in most cases of diffuse large B-cell lymphomas with immunoblastic features (>80%), primary effusion lymphoma, plasmablastic oral lymphoma, and Hodgkin lymphoma. However, only 20% to 30% of HIV-associated Burkitt lymphomas are associated with EBV. The majority of primary effusion and plasmablastic lymphomas harbor HHV-8 in addition to EBV.
Most HIV-associated lymphomas arise from B cells, and several B-cell stimulatory cytokines are elevated in HIV infection for several years before lymphoma diagnosis. Genetic abnormalities frequently involved in HIV-associated lymphoma include TP53, MCY, and BCL-6.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here